Supplemental information on methods for online
advertisement
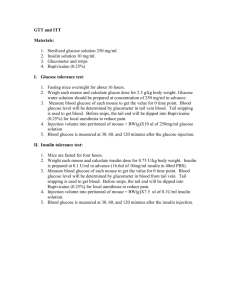
Supplemental information on Methods for on-line appendix Belonging to manuscript: PANCREATIC FAT CONTENT AND Β-CELL FUNCTION IN MEN WITH AND WITHOUT TYPE 2 DIABETES Running title: Pancreatic Fat and β-Cell Dysfunction Maarten E. Tushuizen, MD1, Mathijs C. Bunck, MD1, Petra J. Pouwels, PhD2, Saskia Bontemps, MSc1, Jan Hein T. van Waesberghe, MD, PhD3, Roger K. Schindhelm, MD, PhD1, Andrea Mari, PhD4, Robert J. Heine, MD, PhD, FRCP,1 and Michaela Diamant, MD, PhD1 1 Department of Endocrinology / Diabetes Center; 2Department of Physics & Medical Technology; 3Department of Radiology; VU University Medical Center, Amsterdam, The Netherlands; 4Institute of Biomedical Engineering, National Research Council, Padova, Italy Correspondence to: M. Diamant, MD, PhD Department of Endocrinology / Diabetes Center VU University Medical Center PO Box 7057 1007 MB Amsterdam, The Netherlands Phone: +31-204440534; Fax: +31-204440530 E-mail address: m.diamant@vumc.nl 1 Supplemental information on methods for on-line appendix Section 1. MR-Spectroscopy. MR examinations were performed using a 1.5-T whole-body system (Sonata; Siemens, Erlangen, Germany) in the supine position with the body-array coil positioned at the upper abdominal region. MR imaging and spectroscopy were performed using the body-coil for RF-transmission and spine-array and body-array coils for signal receiving. Axial and coronal steady-state free precession (SSFP) MR images (repetition time TR 3.8 ms, echo time TE 1.9 ms) during free breathing were employed for localization of the volume-of-interest (VOI). Single voxel spectra were recorded by using the stimulated-echo acquisition mode (STEAM) sequence with TR 5000 ms, TE 20 ms, and mixing time 30 ms. A total of 8 acquisitions were obtained, and stored and processed for each coil element separately (yielding typically 24 to 40 spectra – depending on the number of coil elements selected). The short TE and long TR were chosen to ensure optimal detectability of both lipid and water, which was used as an internal standard. User-independent spectral quantification was performed with LCModel (version 6.1)(12). This model is based on simulated lipid and water spectra (with resonances at 0.9 ppm (lipid methyl groups) and 1.3 ppm (lipid methylene groups) and at 4.65 ppm (water), respectively. After processing, the individual spectra were reviewed by an experienced observer, who was blinded for the group variable, in order to discard occasional poorquality spectra, e.g. due to deep breathing. Subsequently, the individual phase-corrected raw time-domain data were added (taking into account corresponding coil sensitivities (13)), yielding one time-domain dataset per VOI, which was quantified again with 2 LCModel. Spectroscopic lipid content is expressed as the percentage of the area under the methyl and methylene peaks relative to that under the water peak. Section 2. Modeling of -cell function parameters. The model consists of three blocks: a) a model for fitting the glucose concentration profile, the purpose of which is to smooth and interpolate plasma glucose concentrations; b) a model describing the dependence of insulin (or C-peptide) secretion on glucose concentrations; and c) a model of C-peptide kinetics, i.e. the two-exponential model proposed by Van Cauter et al (16), in which the model parameters are individually adjusted to the subject’s anthropometric data. The model expresses insulin secretion as the sum of two components. The first component represents the relationship between insulin secretion and absolute glucose concentration at any time-point, i.e. a dose-response function. The mean slope of the dose-response function is taken to represent β-cell glucose sensitivity. Insulin secretion at reference glucose levels representing the average basal glucose concentration (5 mmol/l in nondiabetic and 7 mmol/l in diabetic subjects) was calculated from the β-cell dose-response. The dose-response function is modulated by a time-varying factor, expressing a relative potentiation effect on insulin secretion. The potentiation factor, which encompasses various potentiating signals (glucose-induced potentiation, incretins, neural factors) was set to have a mean value equal to unity over the 2 hours of the study. As the potentiation factor typically increases during an OGTT, the ratio between the potentiation factor value at 2-h and that at time 0 was used as a parameter quantifying potentiation. The second insulin secretion component represents a dynamic dependence of insulin secretion 3 on the rate of change of glucose concentration. It is proportional to the time-derivative of glucose concentration when glucose rises and is zero otherwise. The proportionality constant, termed rate sensitivity, accounts for anticipation of insulin secretion as glucose levels rise. The potentiation factor and total insulin secretion (expressed in pmol/min per square meter of body surface area) were calculated every 5 min for the whole 2-h period, as detailed in (14,15). References (cited above as well as in the printed text) 12. Provencher SW: Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med 30:672-679, 1993 13. Wald LL, Moyher SE, Day MR, Nelson SJ, Vigneron DB: Proton spectroscopic imaging of the human brain using phased array detectors. Magn Reson Med 34: 440-445, 1995 14. Mari A, Schmitz O, Gastaldelli A, Oestergaard T, Nyholm B, Ferrannini E: Meal and oral glucose tests for assessment of beta -cell function: modeling analysis in normal subjects. Am J Physiol Endocrinol Metab 283:E1159-E1166, 2002. 15. Pacini G, Mari A: Methods for clinical assessment of insulin sensitivity and betacell function. Best Pract Res Clin Endocrinol Metab 17:305-322, 2003 16. Van Cauter E, Mestrez F, Sturis J, Polonsky KS: Estimation of insulin secretion rates from C-peptide levels. Comparison of individual and standard kinetic parameters for C-peptide clearance. Diabetes 41:368-377, 1992 4