here
advertisement
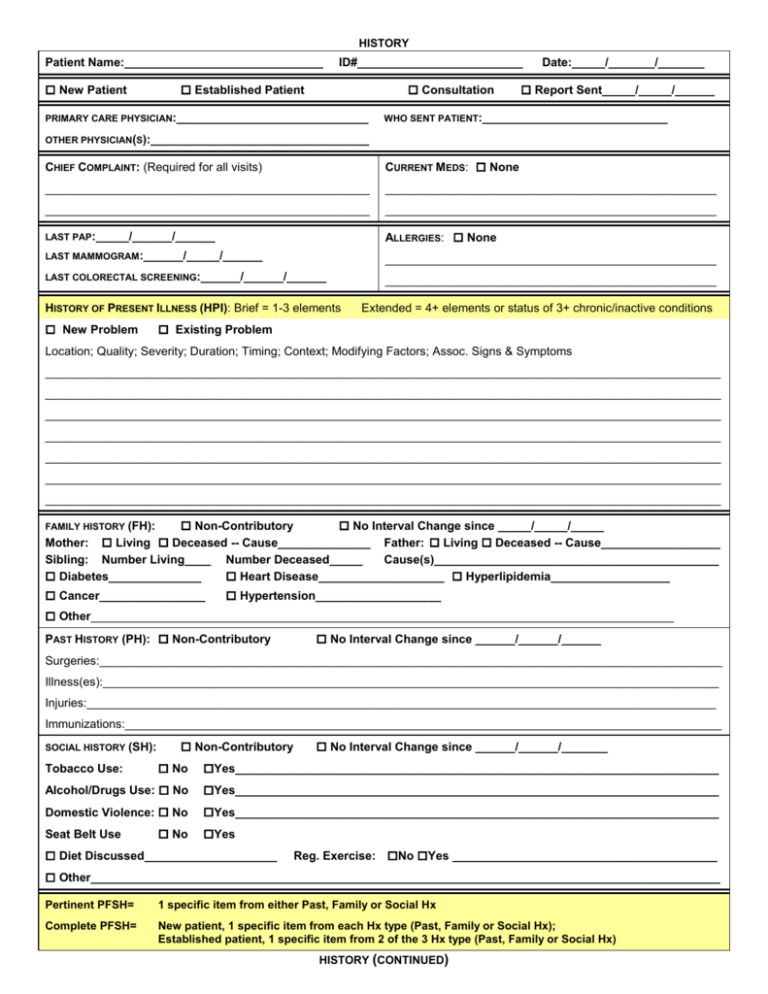
HISTORY Patient Name:______________________________ New Patient ID#_________________________ Established Patient Consultation PRIMARY CARE PHYSICIAN:_____________________________ Date:_____/_______/_______ Report Sent_____/_____/______ WHO SENT PATIENT:____________________________ OTHER PHYSICIAN(S):_________________________________ CHIEF COMPLAINT: (Required for all visits) CURRENT MEDS: None _________________________________________________ __________________________________________________ _________________________________________________ __________________________________________________ LAST PAP:_____/______/______ ALLERGIES: None LAST MAMMOGRAM:______/_____/______ __________________________________________________ LAST COLORECTAL SCREENING:______/______/______ __________________________________________________ HISTORY OF PRESENT ILLNESS (HPI): Brief = 1-3 elements New Problem Extended = 4+ elements or status of 3+ chronic/inactive conditions Existing Problem Location; Quality; Severity; Duration; Timing; Context; Modifying Factors; Assoc. Signs & Symptoms ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ Non-Contributory No Interval Change since _____/_____/_____ Mother: Living Deceased -- Cause______________ Father: Living Deceased -- Cause__________________ Sibling: Number Living____ Number Deceased_____ Cause(s)___________________________________________ Diabetes______________ Heart Disease___________________ Hyperlipidemia__________________ FAMILY HISTORY (FH): Cancer________________ Hypertension___________________ Other________________________________________________________________________________________ PAST HISTORY (PH): Non-Contributory No Interval Change since ______/______/______ Surgeries:______________________________________________________________________________________________ Illness(es):_____________________________________________________________________________________________ Injuries:_______________________________________________________________________________________________ Immunizations:__________________________________________________________________________________________ SOCIAL HISTORY (SH): Non-Contributory No Interval Change since ______/______/_______ No Yes_________________________________________________________________________ Alcohol/Drugs Use: No Yes_________________________________________________________________________ Domestic Violence: No Yes_________________________________________________________________________ Tobacco Use: Seat Belt Use No Yes Diet Discussed____________________ Reg. Exercise: No Yes ________________________________________ Other_______________________________________________________________________________________________ Pertinent PFSH= 1 specific item from either Past, Family or Social Hx Complete PFSH= New patient, 1 specific item from each Hx type (Past, Family or Social Hx); Established patient, 1 specific item from 2 of the 3 Hx type (Past, Family or Social Hx) HISTORY (CONTINUED) REVIEW OF SYSTEMS (ROS) Problem Pertinent ROS = Pos. & Pert. Neg responses related to problem Extended ROS = Pos. & Pert. Neg. responses for 2-9 systems Complete ROS = Pos. & Pert. Neg. responses for at least 10 systems No Changes Since_______/__________/________ 1. Constitutional Negative Wt loss Wt gain Fever Fatigue Other____________________________________________________________ Negative 2. Eyes Vision chg Glasses/contacts Other____________________________________________________________ 3. ENT/Mouth Negative Ulcers Sinusitis Tinnitus Headache Other____________________________________________________________ 4. Cardiovascular Negative Orthopnea Chest pain DOE Edema Palpitation Other____________________________________________________________ 5. Respiratory Negative Wheezing Hemoptysis SOB Cough Other____________________________________________________________ 6. Gastrointestinal Negative Diarrhea Bldy stool N/V Const. Flatulence Pain Other____________________________________________________________ 7. Genitourinary Negative Hematuria Dysuria Urgncy Frqncy Incomp. emptying Incontinent Abn Bldng Dyspareunia Other____________________________________________________________ 8. Musculoskeletal Negative Mscl wkness Other____________________________________________________________ 9. Skin/breast Negative Mastalgia Discharge Masses Rash Ulcers Other____________________________________________________________ 10. Neurological Negative Syncope Seizures Nmbnss Trouble walking Other____________________________________________________________ 11. Psychiatric Negative Depression Crying Other 12. Endocrine Negative _________________________________________________________ Diabetes Hypothyroid Hyperthyroid Hot flashes Other____________________________________________________________ 13. Hemat/Lymph Negative Bruises Other Bleeding Adenopathy _________________________________________________________ 14. Allergic/Immuno (see first page) TOTAL NUMBER SYSTEMS REVIEWED:_____________________ CC HPI ROS PFSH Level of History Required Required Brief Brief N/A Problem Pertinent N/A N/A Required Extended Extended Pertinent Problem Focused Expanded Problem Focused Detailed Required Extended Complete Complete Comprehensive PHYSICAL EXAMINATION ORGAN SYSTEMS CONSTITUTIONAL (Vital Signs, General Appearance Vital signs Ht___________ Wt___________ BP______________ T___________ P_________ R_______ General appearance:________________________________________________________________________________ EYES:_________________________________________________________________________________________________ ______________________________________________________________________________________________________ EARS, NOSE, MOUTH, THROAT:_______________________________________________________________________________ ______________________________________________________________________________________________________ CARDIOVASCULAR:________________________________________________________________________________________ ______________________________________________________________________________________________________ RESPIRATORY:___________________________________________________________________________________________ ______________________________________________________________________________________________________ GASTROINTESTINAL:______________________________________________________________________________________ ______________________________________________________________________________________________________ GENITOURINARY:_________________________________________________________________________________________ ______________________________________________________________________________________________________ SKIN:__________________________________________________________________________________________________ ______________________________________________________________________________________________________ MUSCULOSKELETAL:______________________________________________________________________________________ _ ______________________________________________________________________________________________________ NEUROLOGICAL:__________________________________________________________________________________________ ______________________________________________________________________________________________________ HEMATOLOGIC/LYMPHATIC:__________________________________________________________________________________ ______________________________________________________________________________________________________ PSYCHIATRIC:____________________________________________________________________________________________ ______________________________________________________________________________________________________ BODY AREAS Head/face:__________________________________________________________________________________________ Neck:______________________________________________________________________________________________ Chest/Breasts/Axillae:_________________________________________________________________________________ Abdomen:__________________________________________________________________________________________ Genitalia/Groin/Buttocks:______________________________________________________________________________ Back/Spine:_________________________________________________________________________________________ Each Extremity: Content and Documentation Requirements For each level of examination, the following must be documented in the chart: Specific abnormal and relevant negative findings for affected or symptomatic body area(s)/organ system(s) Abnormal or unexpected findings of unaffected or asymptomatic body area(s)/organ system(s) “Normal” or “negative” is only sufficient for unaffected area(s) or asymptomatic organ system(s) Level of Exam Perform and Document Problem Focused Expanded Problem Focused Detailed Comprehensive Limited exam of one body area or organ system Limited exam of the affected body area or organ system plus any other symptomatic or related organ system(s) - commonly interpreted by HCFA auditors to mean 2-4 systems total. Extended exam of the affected body area(s) and other symptomatic or related organ system(s) - commonly interpreted by HCFA auditors to mean 5-7 systems total. General Multisystem: Documentation of 8 or more findings about the 12 organ systems Single Organ System: Not formally defined and left up to the discretion of the auditor, but CPTdefined as a complete exam of a single organ system MEDICAL DECISION MAKING AMOUNT AND COMPLEXITY OF DATA REVIEWED: Test(s) ordered: Laboratory_________________________________________________________________________________________ Radiology/Ultrasound________________________________________________________________________________ Review of Records: Previous Test results:____________________________________________________________________________ Discussion of test results with other physician_______________________________________________________ Old records reviewed:____________________________________________________________________________ History obtained from other source:________________________________________________________________ Minimal/None = 1 from above, Limited = 2 from above, Moderate = 3 from above, Extensive = 4+ from above DIAGNOSES/MANAGEMENT OPTIONS: Minimal = Minor problem Established Problem New Problem Limited = Established problem, stable/improved Multiple = Established problem, uncertain status; New problem, stable Extensive = New problem uncertain status ASSESSMENT AND PLAN:______________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ _________________________________________________________________________________________________ RISK OF COMPLICATIONS AND/OR MORBIDITY/MORTALITY FROM DIAGNOSES, DIAGNOSTIC PROCEDURES AND MANAGEMENT CHOICES: Minimal (eg, Cold, Aches & pains, insect bite) Low (eg, Cystitis, vaginitis, minor surgery w/no risk factors, OTC meds) Moderate (eg Breast mass, irreg. bleeding, headaches, biopsy, minor surgery w/risk factors, Rx drug management) High (eg, Pelvic pain, rectal bleeding, Multiple complaints, Major surgery planned, Chemotherapy,) PATIENT COUNSELED RE: ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ Minutes Counseled__________________ Total Encounter Time______________________ Signature____________________________________________________Date______/_____/_____ 2 of the 3 elements must be met or exceeded to qualify for a given type of medical decision making Amt/Complexity Data Diagnoses/ Mgt Risk of Complications Type of Decision-Making Options Minimal/ None Minimal Minimal Straight-forward Limited Limited Low Low Complexity Moderate Multiple Moderate Moderate Complexity Extensive Extensive High High Complexity