here - Greater Louisville Medical Society
advertisement

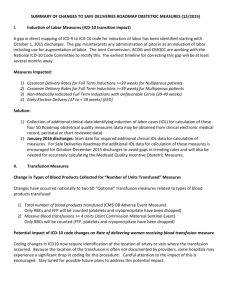
GLMS PPAC Business meeting and Part 2 of the GLMS/PPAC Education Series The Business Impact of ICD-10 – presented by Jessica Williams, Manager Greater Louisville Medical Society Physician Education & Practice Support July 12, 2012 7:00 A.M. Baptist Hospital East Education Center Auditorium Trudi Rash, MD - Chair WELCOME AND INTRODUCTIONS – DR. TRUDI RASH Dr. Rash welcomed the committee and guests to the second part of a three-part series of educational workshops. Summary approved APPROVAL OF JUNE MEETING SUMMARY UPCOMING MEETINGS (send agenda items to stephanie.woods@glms.org) Aug. 16, 2012 Anthem IIRC GLMS Offices August 30, 2012 CGS IIRC GLMS Offices September 7, 2012 Passport IIRC GLMS Offices Sept 13, 2012 UHC IIRC Roundtable GLMS Offices Sept. 27, 2012 Humana IIRC GLMS Offices Dr. Rash reminded the committee to submit hassles/agenda items as soon as possible for the upcoming GLMS/UHC Roundtable to be held on September 13, 2012 in order to allow the insurer ample time to get responses to the issues. NEW BUSINESS Committee to submit hassles and/or agenda items for UHC IIRC Roundtable on 9.13.12 Advocacy House calls Stephanie reported that she made a house call to Internal Medicine & Pediatric Associates which was very successful. Many issues were discussed and not all were about insurance. Stephanie reminded the committee to call GLMS to set up a house call to discuss any issues, including those about PQRS, Meaningful Use, etc. Dr. Rash stated that GLMS will be holding a Small Practice Forum on July 18 at 7:30 am at their location at 101 W. Chestnut Street. This meeting is in response to the June PPAC presentation on Meaningful Use and it’s purpose will be to discuss issues and problems that small practices are having complying to the new Medicare regulations and other concerns. GLMS to hold Small Practice Forum on 7.18.12 to discuss Medicare regs and other concerns GLMS to hold Dr. Rash reminded the committee that there will be a Town Hall Meeting on July 26 at 7 am at GLMS Town Hall on 7.26.12 with attorneys from Wyatt, Tarrant & Combs who will be talking about the implications and regarding the controlled substance law. requirements of the controlled substance law. COUNTDOWN TO ICD-10 - THE BUSINESS IMPACT OF ICD-10 – JESSICA WILLIAMS Entire presentation can be viewed on the GLMS Website under Advocacy, Up to this point, the “Countdown to ICD-10” series has given examples of how the number of codes Physician Practice will increase under ICD-10 and how greater specificity in documentation will be required for payment. Advocacy and PPAC. However, the transition to ICD-10 will also impact the business operations of the practice. Everyone 2 who currently touches an ICD-9 code will be affected – front desk, nurses, physicians, clinical area, managers, lab, billing and, of course, coding. Currently, a proposed rule has ICD-10 implementation scheduled for October 2014. By starting on planning, communication and awareness, and assessment now, practices can have a smooth transition to ICD-10. The Centers for Medicare and Medicaid Services has produced an ICD-10 implementation guide for small and medium practices that contains helpful checklists and timelines: (www.cms.gov/Medicare/Coding/ICD10/ProviderResources.html) There are numerous other ICD-10 resources available, many for free, that can be utilized. Planning 9:57 The top leadership of the practice must understand the significance of the transition to ICD-10. This should be clear to physicians, particularly those in smaller practices who realize how coding affects the bottom line. Transitioning to ICD-10 will be an involved process, and the practice manager should not try to handle all aspects. He or she should establish a project management structure. Key staff members, perhaps a lead coder, should be identified and empowered to develop education for staff, for example. Practices will need to know when their external vendors are ICD-10-ready. If vendors are not prepared, the practice’s preparation will be useless. All entities need to be ready ahead of the compliance deadline so that practices can run end-to-end testing ahead of time. For this planning process, creating a well-defined timeline and accountability for the practice will be important. Coding is the currency of your practice. Communication and Awareness 13:14 When it comes to communication, start making each staff member aware of what ICD-10 is and how it will affect each person’s job duties. Keep the explanation simple and repeat it as necessary. The truth is that everyone will need education. For coding staff members, perform a detailed assessment of their current knowledge. Some may need additional education in the areas of anatomy and physiology to prepare. Closer to the implementation date, each coder will need at least 20 hours of intense training. To practice documentation under ICD-10, try selecting a high-volume code and using the ICD-10 codes now. Choose one code per month or one per quarter. This exercise will familiarize everyone with the changes and make a difference later on. About three to six months before the implementation date, physicians will need specialty-specific training on documentation. Unfortunately, the transition to ICD-10 will have an impact on the practice’s budget, but the cost can be spread over a few years. The implementation budget must include: Hardware, software, EHR templates and maintenance fees Communication (new forms, internal communications) Training Outsourcing or consultant fees Temporary staffing needs Data conversion Report design and reprinting paper forms Systems testing 3 31:49 In addition, there will need to be a budget after the transition for monitoring code compliance, ongoing education and revenue stream analysis. The practice must ensure that the new codes are being paid at the correct rate. An initial loss of revenue is to be expected as coding takes longer, claims are adjudicated more slowly and claims are rejected. The practice can prepare for cash flow delays by prepaying with vendors if possible, managing accounts receivable, collecting co-pays and deductibles at the time of service and checking with the bank on an increased credit line, to be used if payers experience problems with ICD-10. Assessment The practice should monitor the status of both vendors and payers on ICD-10 readiness. Healthcare Information and Management Systems offers a “VitalVendor” readiness tool (www.himss.org/ASP/topics_icd10playbook.asp) where major vendors are reporting their status. Ask vendors these questions and track their answers in a spreadsheet: Will software be replaced or updated? Is a demo available? What is the timeline for go-live? Will there be a new service level agreement, contract or fees? For payers, find out when testing will begin, how the referral/authorization will change and whether contracts will change. GLMS plans to gather this information from payers through its five Insurance Issues Resolution Committees. GLMS to gather information regarding: Vendor ICD-10 testing dates How referral/auths will change, and whether contracts will change. These steps can help make the transition to ICD-10 manageable for the practice. Now is the best time to begin planning, communication and assessment – the keys to successful implementation. ICD-10 Resources: - CMS ICD-10 Implementation Guide for Small and Medium Practices o http://www.cms.gov/Medicare/Coding/ICD10/downloads/ICD10SmallandMediumP ractices508.pdf - Enroll for CMS ICD-10 email updates o https://www.cms.gov/Medicare/Coding/ICD10/CMS_ICD10_Industry_Email_Updates.html - AHIMA ICD-10-CM/PCS Readiness Assessment and Prioritization Tool o http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_046262.pdf - ICD- 10 Form Letter and Vendor Questionnaire o https://www.glms.org/Default.aspx?PageID=500 - ICD-10 Vendor Readiness Tool – online self-reported readiness by vendors, courtesy of HIMSS o http://www.himss.org/ASP/topics_icd10playbook_vitalVendors.asp?faid=573&tid= 100 - AHRQ Article on the Impact of ICD-10 in Quality Reporting and Physician Monitoring http://www.qualityindicators.ahrq.gov/Downloads/Resources/Publications/2011/ICD10%20Report%2002-08-11%20Final.pdf NEXT MEETING: August 9, 2012, 7:00-9:00 am, Baptist Hospital East Auditorium – ICD-10 Documentation ADJOURN 4 GLMS/PPAC Educational Series The Business Impact of ICD-10 July 12, 2012 Physicians: Trudi Rash, MD, Chair Berberich, Susan MD Dee, Michael MD Martin, Alvin MD ATTENDANCE Practice Mgmt Representatives: Beckman, Libby Breedlove, Julie Carlisle, Laura Christian, Terri Collier, Melissa Dawling, Michelle Esterle, Elaine Gossman, Jan Haworth, Sandy Hilton, Demetria Hyland, Jane Kastanis, Terry Kissell, Lynn Kustes, Brenda Leep, Bunny Mattingly, Sherry McCallister, Mary Pat McGary, Annette McGregor, Amy Nave, Nona Priddy, Sherry Ray, R Sacra, Patti Thomas, Sherry GLMS Staff: Lelan Woodmansee, GLMS, Executive Director Jessica Williams, GLMS Manager, Physician Education and Practice Support Stephanie Woods, GLMS Senior Advocacy Specialist Joyce Goldin, GLMS Administrative Assistant Ellen Hale, GLMS Communications Associate LMS Executive Committee: Russ Williams, MD, President David Bybee, MD, Board Chair James P. Murphy, MD, Pres Elect Robert Zaring, MD, Treasurer 5