Part nurse, part doctor, no job
advertisement

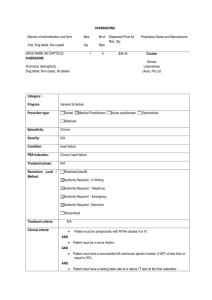
Part nurse, part doctor, no job By Richard Watts, Times Colonist March 11, 2010 Nick Fitterer is a UVic student in the masters program to become a nurse practitioner, but government policies have made it difficult to find work. Most recently graduated nurse practitioners are working as registered nurses, a job they are over-qualified for. Photograph by: Debra Brash, Times Colonist University of Victoria master's degree student Nick Fitterer is just months away from graduating as a nurse practitioner, and is anxious to get out in the community treating patients in his role as part-nurse, part-doctor. But Fitterer, a 32-year-old father of two, is caught in what even health officials admit is a conundrum. He's studying for a job that is supposed to be the next new trend in health care, yet he'll have a hard time finding work because the system hasn't kept pace, and doesn't have any spaces for him. "Everything about [becoming a nurse practitioner] made sense. It was logical. I thought there would be a need for it. But politically speaking, we've hit a bit of wall," he said. Nurse practitioners were first recognized in B.C. in May 2005 through changes to the provincial Health Professions Act. They are registered nurses who have a bachelor's degree in nursing and have worked for at least two years, then returned to university for two more years to earn a master's degree. The extra qualifications put them a step above RNs, but not on par with a general-practice physician. They can prescribe most medications, but not narcotics and botox, can deal with most common ailments, and can order most tests and x-rays. The position was touted as an effective way to deliver primary health by taking over some of the duties now mostly delivered through GPs, who are in short supply. According to 2008 data from Statistics Canada, 132,000 British Columbians don't have a general practitioner, or about four per cent of the population age 12 and over. A 2009 study by Victoria-based Hollander Analytical Services Ltd. found that patients with chronic diseases who don't have family doctors cost the health system nearly three times more than those who don't. For example, diabetes patients without a general practitioner cost the health system on average $17,000 a year, compared to $5,900 for those who see their doctor regularly, says the study. But the concept of nurse practitioners has failed to catch on enough to absorb the numbers who are graduating, leaving many out of work, or forced to work as registered nurses -- jobs for which they are overqualified. "There is a big need there and we could make a dent in that need, if we could just go to work," said Lynn Guengerich, president of the B.C. Nurse Practitioners' Association. According to Guengerich, 179 nurse practitioners held active licences in B.C. as of September. But about 50 are looking for a job or are working below their qualifications. She said those figures show six nurse practitioners were working in private practices with doctors, one was employed by government, and 117 were attached to various health authorities. Meanwhile, the combined universities of Victoria, B.C. and Northern B.C. are graduating about 45 nurse practitioners every year. The province supports the idea of nurse practitioners -- it set aside $62.7 million for health authorities to fund the positions between 2005 and 2010 -- and says they can offer substantial savings in primary health care. On average, a nurse practitioner in B.C. makes $119,000 a year, compared to $98,411 for a registered nurse, and $247,517 for general practitioner (from which office rent and staff are paid.) Yet the Ministry of Health agrees the health-care system isn't quite sure how to make best use of nurse practitioners' skills. In a prepared statement, the ministry said that "because the nurse practitioner role is very new in our province, the ministry and health authorities are building innovative models to support placement of nurse practitioners." One hurdle for nurse practitioners is that while the legislation allows them to treat patients without direct supervision by a physician, they are not allowed to bill the Medical Services Plan on a fee-for-service basis, like doctors. That means nurse practitioners can't hang up their shingles and start seeing patients in their own private practices -- they either have to work in a practice alongside a doctor, or in a clinic funded by a health authority. But without the fees paid for their services, few practices can support nurse practitioners. So that takes the nurse practitioners back to the health authorities, which concentrate the biggest portion of their resources on hospitals, leaving little for clinics offering primary care. According to the Vancouver Island Health Authority's 2009-2012 service plan, more than $900 million of its $1.7-billion budget goes to acute care, compared to just $58 million to population health and wellness -- the money that would be used for nurse practitioners. "It's a bit of a conundrum," said Victoria Power, director of primary health care and chronic-disease management for VIHA. Indeed, of VIHA's more than 17,000 employees, there are only 17 nurse practitioners -- they work in urban clinics like the Access Health Centre at 713 Johnson St., and in clinics in smaller communities like Cortes Island and at Mount Washington. It's a different story in Ontario, where government policy has pushed harder with a variety of funding models to get nurse practitioners into the system since they were first recognized in the 1970s. Paula Carere, president of the Nurse Practitioners' Association of Ontario, said about 1,600 are now registered in Ontario. They work in a variety of clinics, providing primary care, and their salaries -- $87,000 to $89,000 -- are paid directly by the Ontario Ministry of Health. They can work on family health teams with doctors, in nurse practitioner-led clinics and in community health centres, set up to tend those who traditionally find themselves without a family doctor, like immigrant populations or the mentally ill. Carere said the Ontario government is so committed to nurse practitioners, it plans to increase the numbers of nurse practitioner-led clinics from 11 to 25 within the year. "It's very interesting to watch the momentum," said Carere. "It's kind of exciting here." The Ontario experience is encouraging for people like Dr. Rita Schreiber, program co-ordinator for UVic's nurse practitioner program, who believes it's only a matter of time before B.C. follows suit. "We are only five years into this project," said Schreiber. "It can be expected that we would have bumps in the road. "We just push forward and say what needs to happen and it will eventually change. And it will because logic does win out occasionally." rwatts@tc.canwest.com © Copyright (c) The Victoria Times Colonist