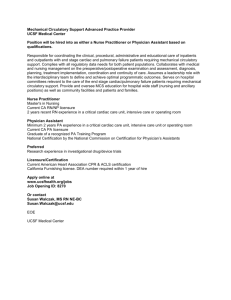
Chapter 14: Nursing Management: Patients With Coronary Vascular
advertisement

Chapter 14: Nursing Management: Patients With Coronary Vascular Disorders *The following is a sample care plan meant for adaptation. Always revise to meet your facility’s protocols and the latest research and nursing diagnoses. PLAN OF NURSING CARE Care of the Patient After Cardiac Surgery NURSING DIAGNOSIS: Decreased cardiac output related to blood loss and compromised myocardial function GOAL: Restoration of cardiac output to maintain organ and tissue perfusion Nursing Interventions Rationale Expected Outcomes 1. Monitor cardiovascular 1. Effectiveness of cardiac ● The following status. Serial readings output is determined by parameters are within of blood pressure, other continuous monitoring. the patient’s normal hemodynamic ranges: parameters, and cardiac Arterial pressure rhythm and rate are CVP obtained, recorded, and Pulmonary artery correlated with the pressures patient’s overall PAWP condition. Heart sounds a. Assess arterial blood a. Blood pressure is pressure every 15 one of the most minutes until stable; important physiologic then arterial or cuff parameters to Pulmonary and systemic vascular resistance Cardiac output and cardiac index blood pressure every monitor; Peripheral pulses 1 to 4 hours × 24 vasoconstriction Cardiac rate and rhythm hours; then every 8 after Cardiac biomarkers to 12 hours until cardiopulmonary Urine output hospital discharge. bypass may require treatment with an IV vasodilator. b. Auscultate for heart sounds and rhythm. b. Auscultation provides evidence of cardiac tamponade (muffled distant heart sounds), pericarditis (precordial rub), arrhythmias. c. Assess peripheral c. Presence or pulses (pedal, tibial, absence and quality radial). of pulses provide data about cardiac output as well as obstructive lesions. d. Monitor d. Rising CVP and hemodynamic PAWP may indicate parameters to congestive heart Skin and mucosal color Skin temperature assess cardiac failure or pulmonary output, volume edema. Low status, and vascular pressures may tone. indicate need for volume replacement. e. Watch for trends in e. Trends are more hemodynamics and important than note that mechanical isolated readings. ventilation may alter Mechanical hemodynamics. ventilation increases intrathoracic pressure. f. Monitor ECG pattern f. Arrhythmias may for cardiac occur with coronary arrhythmias and ischemia, hypoxia, ischemic changes. bleeding, acid-base or electrolyte disturbances, digitalis toxicity, or cardiac failure. STsegment changes may indicate myocardial ischemia. Pacemaker capture and antiarrhythmic medications are used to maintain heart rate and rhythm and to support blood pressure. g. Assess cardiac g. Elevations may biomarker results. indicate myocardial infarction. h. Measure urine h. Urine output less output every half than 30 mL/h hour to 1 hour at indicates decreased first, then with vital renal perfusion and signs. may reflect decreased cardiac output. i. j. Observe buccal i. Duskiness and mucosa, nail beds, cyanosis may lips, earlobes, and indicate decreased extremities. cardiac output. Assess skin; note j. Cool moist skin temperature and indicates color. vasoconstriction and decreased cardiac output. 2. Observe for persistent 2. Bleeding can result from ● Less than 200 mL/h of bleeding: excessive surgical trauma to drainage through chest chest tube drainage of tissues, anticoagulant tubes during first 4 to 6 blood; hypotension; low medications, and hours. CVP; tachycardia. clotting defects. ● Vital signs stable. Prepare to administer blood products, IV solutions. 3. Observe for cardiac 3. Cardiac tamponade ● CVP and other tamponade: results from bleeding hemodynamic hypotension; rising CVP into the pericardial sac parameters within and PAWP, pulsus or accumulation of fluid normal limits. paradoxus; muffled in the sac, which heart sounds; weak, compresses the heart thready pulse; jugular and prevents adequate ● Skin color normal. vein distention; filling of the ventricles. ● Respirations unlabored, decreasing urinary Decrease in chest output. Check for drainage may indicate diminished amount of that fluid and clots are ● Urinary output within normal limits. clear breath sounds. ● Pain limited to incision. blood in chest drainage accumulating in the collection system. pericardial sac. Prepare for reoperation. 4. Observe for signs of 4. Cardiac failure results cardiac failure. Prepare from decreased to administer diuretics, pumping action of the digoxin, IV inotropic heart; can cause agents. deficient perfusion to vital organs. NURSING DIAGNOSIS: GOAL: Impaired gas exchange related to chest surgery Adequate gas exchange Nursing Interventions Rationale Expected Outcomes 1. Maintain mechanical 1. Ventilatory support is ● Airway patent. ventilation until the used to decrease work patient is able to of the heart, to maintain breathe independently. effective ventilation, and ● ABGs within normal range. ● Endotracheal tube to provide an airway in correctly placed, as the event of evidenced by x-ray. complications. 2. Monitor arterial blood 2. ABGs and ventilator gases, tidal volume, parameters indicate peak inspiratory effectiveness of pressure, and ventilator and changes ● Breath sounds clear bilaterally. ● Ventilator synchronous with respirations. extubation parameters. that need to be made to improve gas exchange. ● Breath sounds clear after suctioning/coughing. 3. Auscultate chest for breath sounds. 3. Crackles indicate pulmonary congestion; decreased or absent ● Nail beds and mucous membranes pink. ● Mental acuity consistent breath sounds may with amount of indicate pneumothorax, sedatives and hemothorax, analgesics received. dislodgement of tube. ● Oriented to person; able to respond yes and no appropriately. 4. Sedate patient 4. Sedation helps the ● Able to be weaned adequately, as patient to tolerate the successfully from prescribed, and monitor endotracheal tube and ventilator. respiratory rate and to cope with ventilatory depth. sensations. 5. Suction 5. Retention of secretions tracheobronchial leads to hypoxia and secretions as needed, possible infection. using strict aseptic technique. 6. Assist in weaning and 6. Extubation decreases endotracheal tube risk of pulmonary removal. infections and enhances ability of patient to communicate. 7. After extubation, 7. Aids in keeping airway promote deep breathing, patent, preventing coughing, and turning. atelectasis, and Encourage use of the facilitating lung incentive spirometer and expansion. compliance with breathing treatments. Teach incisional splinting with a “cough pillow” to decrease discomfort. NURSING DIAGNOSIS: Risk for imbalanced fluid volume and electrolyte imbalance related to alterations in blood volume GOAL: Fluid and electrolyte balance Nursing Interventions Rationale Expected Outcomes 1. Monitor fluid and 1. Adequate circulating ● Fluid intake and output electrolyte balance. blood volume is necessary for optimal cellular activity; fluid and balanced. ● Hemodynamic assessment parameters electrolyte imbalance negative for fluid can occur after surgery. overload or hypovolemia. a. Accurately document a. Provides a method intake and output; to determine positive record urine volume or negative fluid every half hour to 4 balance and fluid hours while in critical requirements. care unit; then every 8 to 12 hours while hospitalized. b. Assess blood b. Provides information pressure, about state of hemodynamic hydration. ● Normal blood pressure with position changes. ● Absence of arrhythmia. parameters, weight, ● Stable weight. electrolytes, ● Arterial blood pH 7.35 to hematocrit, jugular 7.45. ● Serum potassium 3.5 to venous pressure, breath sounds, 5.0 mEq/L (3.5 to 5.0 urinary output, and mmol/L). nasogastric tube drainage. c. Measure c. Excessive blood loss ● Serum magnesium 1.3 postoperative chest from chest cavity can to 2.3 mg/dL (0.62 to drainage; cessation cause hypovolemia. 0.95 mmol/L). ● Serum sodium 135 to of drainage may indicate kinked or 145 mEq/L (135 to 145 blocked chest tube. mmol/L). ● Serum calcium 8.6 to Ensure patency and integrity of the 10.2 mg/dL (2.15 to 2.55 drainage system. mmol/L). Maintain autotransfusion system if in use. d. Weigh daily and correlate with intake d. Indicator of fluid balance. and output. 2. Be alert to changes in serum electrolyte levels. 2. A specific concentration of electrolytes is necessary in both extracellular and intracellular body fluids to sustain life. a. Hypokalemia (low a. Causes: inadequate potassium) intake, diuretics, Effects: arrhythmias: vomiting, excessive ● Serum glucose less than 110 mg/dL. PVCs, ventricular nasogastric tachycardia. drainage, stress from Observe for specific surgery. ECG changes. Administer IV potassium replacement as prescribed. b. Hyperkalemia (high b. Causes: increased potassium) intake, hemolysis Effects: ECG from changes, tall peaked cardiopulmonary T waves, wide QRS, bypass/mechanical brachycardia. Be assist devices, prepared to acidosis, renal administer diuretic or insufficiency. The an ion-exchange resin binds resin (sodium potassium and polystyrene promotes intestinal sulfonate excretion of it. IV [Kayexalate]); IV sodium bicarbonate sodium bicarbonate, drives potassium into or IV insulin and the cells from glucose. extracellular fluid. Insulin assists the cells with glucose and potassium absorption. c. Monitor serum c. Low levels of magnesium, sodium magnesium are and calcium. associated with arrhythmias, muscle spasm, and tetany. Low levels of sodium are associated with weakness and neurological symptoms. Low levels of calcium can lead to arrhythmias and muscle spasm. d. Hyperglycemia (high d. Cause: stress blood glucose) response to surgery. Effects: increased Affects both patients urine output, thirst, with diabetes and those metabolic acidosis without diabetes. Administer insulin as prescribed. NURSING DIAGNOSIS: Disturbed sensory perception related to excessive environmental stimulation, sleep deprivation, physiological imbalance GOAL: Reduction of symptoms of sensory perceptual imbalance; prevention of postcardiotomy delirium Nursing Interventions Rationale Expected Outcomes 1. Use measures to 1. Postcardiotomy delirium ● Cooperates with prevent postcardiotomy may result from anxiety, delirium: sleep deprivation, a. Explain all increased sensory input, procedures and the disorientation to night need for patient and day. Normally, cooperation. sleep cycles are at least b. Plan nursing care to procedures. ● Sleeps for long, uninterrupted intervals. ● Oriented to person, place, time. ● Experiences no 50 minutes long. The perceptual distortions, provide for periods of first cycle may be as hallucinations, uninterrupted sleep long as 90 to 120 disorientation, with patient’s normal minutes and then delusions. day–night pattern. shorten during c. Promote continuity of care. d. Orient to time and place frequently. successive cycles. Sleep deprivation results when the sleep cycles are interrupted or Encourage family to inadequate in number. visit. e. Assess for medications that may contribute to delirium. 2. Observe for perceptual 2. Delirium can indicate a distortions, serious medical hallucinations, condition such as disorientation, and hypoxia, acid-base paranoid delusions. imbalance, metabolic abnormalities, and cerebral infarction. NURSING DIAGNOSIS: Acute pain related to surgical trauma and pleural irritation caused by chest tubes GOAL: Relief of pain Nursing Interventions Rationale Expected Outcomes 1. Record nature, type, 1. Pain and anxiety ● States pain is location, intensity, and increase pulse rate, duration of pain. oxygen consumption, and cardiac workload. decreasing in severity. ● Reports absence of pain. ● Restlessness decreased. 2. Encourage routine pain 2. Analgesia promotes ● Vital signs stable. ● Participates in deep- medication dosing for rest, decreases oxygen the first 24 to 72 hours consumption caused by breathing and coughing and observe for side pain, and aids patient in exercises. effects of lethargy, performing deep- hypotension, breathing and coughing complaints of pain each tachycardia, respiratory exercises; pain day. depression. medications is more ● Verbalizes fewer ● Positions self; effective when taken participates in care before pain is severe. activities. ● Gradually increases activity. NURSING DIAGNOSIS: Ineffective renal tissue perfusion related to decreased cardiac output, hemolysis, or vasopressor drug therapy GOAL: Maintenance of adequate renal perfusion Nursing Interventions Rationale Expected Outcomes 1. Assess renal function: 1. Renal injury can be ● Urine output consistent caused by deficient with fluid intake; greater perfusion, hemolysis, than 30 mL/h. low cardiac output, and use of vasopressor agents to increase blood pressure. ● Urine specific gravity 1.003 to 1.030. a. Measure urine a. Less than 30 mL/h ● BUN, creatinine, output every half indicates decreased electrolytes within hour to 4 hours in renal function. normal limits. critical care then every 8 to 12 hours until hospital discharge. b. Monitor and report b. Indicate kidneys’ lab results: BUN, ability to excrete serum creatinine, waste products. serum electrolytes. 2. Prepare to administer 2. Promote renal function rapid-acting diuretics or and increase cardiac inotropic drugs (eg, output and renal blood dobutamine). flow. 3. Prepare patient for 3. Provides patient with the dialysis or continuous opportunity to ask renal replacement questions and prepare therapy if indicated. for the procedure. NURSING DIAGNOSIS: Ineffective thermoregulation related to infection or postpericardiotomy syndrome GOAL: Maintenance of normal body temperature Nursing Interventions Rationale Expected Outcomes 1. Assess temperature every hour. 1. Fever can indicate infectious or ● Normal body temperature. inflammatory process. 2. Use aseptic technique when changing 2. Decreases risk of infection. dressings, suctioning ● Incisions are free of infection and are healing. ● Absence of symptoms endotracheal tube; maintain closed systems of postpericardiotomy for all intravenous and syndrome: fever, arterial lines and for malaise, pericardial indwelling urinary effusion, pericardial catheter. friction rub, arthralgia. 3. Observe for symptoms 3. Occurs in approximately of postpericardiotomy 10% of patients after syndrome. cardiac surgery. 4. Obtain cultures and other lab work (CBC, 4. Antibiotics treat documented infection. ESR); administer antibiotics as prescribed. 5. Administer antiinflammatory agents as directed. 5. Relieve symptoms of inflammation. NURSING DIAGNOSIS: GOAL: Deficient knowledge about self-care activities Ability to perform self-care activities Nursing Interventions Rationale Expected Outcomes 1. Develop teaching plan 1. Each patient will have ● Patient and family for patient and family. unique learning needs. members explain and Provide specific comply with therapeutic instructions for the regimen. ● Patient and family following: ● Diet and daily members identify weights necessary lifestyle ● Activity progression changes. ● Exercise ● Has copy of discharge ● Deep breathing, instructions (in the coughing, lung patient’s primary expansion exercises language and at ● Temperature appropriate reading monitoring level; has an alternate ● Medication regimen format if indicated). ● Pulse taking ● Keeps follow-up ● Access to the appointments. emergency medical system 2. Provide verbal and 2. Repetition promotes written instructions; learning by allowing for provide several teaching questions and sessions for clarification of reinforcement and misinformation. answering questions. 3. Involve family in teaching sessions. 3. Family members responsible for home care are usually anxious and require adequate time for learning. 4. Provide contact 4. Arrangements for information for surgeon contacts with health and cardiologist and care personnel help to instructions about allay anxieties. follow-up visit with surgeon. 5. Make appropriate 5. Learning, recovery and referrals: home care lifestyle changes agency, cardiac continue after discharge rehabilitation program, from the hospital. community support groups.