Hemodynamic Assessment
advertisement
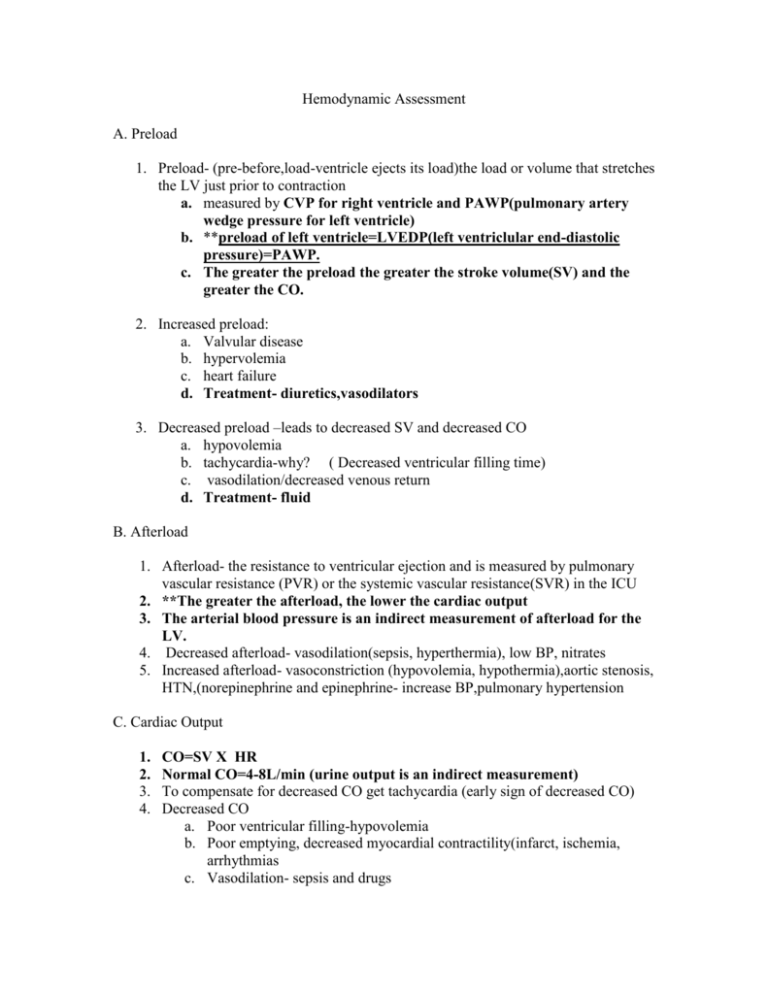
Hemodynamic Assessment A. Preload 1. Preload- (pre-before,load-ventricle ejects its load)the load or volume that stretches the LV just prior to contraction a. measured by CVP for right ventricle and PAWP(pulmonary artery wedge pressure for left ventricle) b. **preload of left ventricle=LVEDP(left ventriclular end-diastolic pressure)=PAWP. c. The greater the preload the greater the stroke volume(SV) and the greater the CO. 2. Increased preload: a. Valvular disease b. hypervolemia c. heart failure d. Treatment- diuretics,vasodilators 3. Decreased preload –leads to decreased SV and decreased CO a. hypovolemia b. tachycardia-why? ( Decreased ventricular filling time) c. vasodilation/decreased venous return d. Treatment- fluid B. Afterload 1. Afterload- the resistance to ventricular ejection and is measured by pulmonary vascular resistance (PVR) or the systemic vascular resistance(SVR) in the ICU 2. **The greater the afterload, the lower the cardiac output 3. The arterial blood pressure is an indirect measurement of afterload for the LV. 4. Decreased afterload- vasodilation(sepsis, hyperthermia), low BP, nitrates 5. Increased afterload- vasoconstriction (hypovolemia, hypothermia),aortic stenosis, HTN,(norepinephrine and epinephrine- increase BP,pulmonary hypertension C. Cardiac Output 1. 2. 3. 4. CO=SV X HR Normal CO=4-8L/min (urine output is an indirect measurement) To compensate for decreased CO get tachycardia (early sign of decreased CO) Decreased CO a. Poor ventricular filling-hypovolemia b. Poor emptying, decreased myocardial contractility(infarct, ischemia, arrhythmias c. Vasodilation- sepsis and drugs d. Increased SVR- hypertension, vasoconstriction, aortic stenosis, mitral insufficiency, ventricular septal defects 5. Increased CO a. Increased O2 demand (exercise) b. Sympathetic nervous system (fear, anxiety) D. Heart Rate 1. Tachycardia above 120 leads to decreased CO due to decreased ventricular filling 2. Causes- hypoxia, fear, anxiety, hypovolemia, catecholamines, pain, exercise 3. Bradycardia- sudden bradycardia leads to CO.Increased SV that leads to bradycardia can increase CO- athletes 4. Causes- vagal stimulation, heart blocks, drugs,athletes 5. Arrhythmias result in decreased CO due to loss of synchronized atrial and ventricular filling and ejection(mechanical events follow electrical events) E. Stroke Volume 1. The amount of blood ejected with each heartbeat. Initially with cardiac dysfunction, may not see a decrease in SV due to compensation (increased HR) 2. Normal SV=60-130cc/beat 3. Factors that determine SV a. preload b. afterload c. contractility F. Contractility 1. Defined as the ability of the cardiac muscle to contract. Starling’s Law= the greater the stretch of muscle fibers, the greater the force of contraction and volume of blood ejected. 2. Increased contractility a. sympathetic stimulation b. drugs (dig, dopamine, dobutamine, epinephrine calcium) 3. Decreased contractility a. loss of myocardial function (acute MI, cardiomyopathy b. hypoxemia c. electrolyte imbalance(K,Ca, Mg) d. drugs(lidocaine, calcium channel blockers, beta blockers) e. contractility is not measured directly but can be determined by the SV and the ejection fraction(EF) which is measured via and echocardiogram f. EF is defined as how much blood is pumped with each contraction in relation to how much blood is available to be pumped. Normal is 55%65%. Ex. 90/140=64% EF G. CVP 1. Measures the pressure in the RA and reflects the ability of the right side of the heart to pump blood 2. Normal 2-8mm Hg 3. Decreased CVP a. hypovolemia b. decreased venous return 4. Increased CVP a. hypervolemia b. increased venous return c. right sided heart failure, pulmonary hypertension d. tricuspid stenosis and regurgitation H. Pulmonary Artery Pressure (PAP) 1. **Normal pressure 20-30 mmHg systolic and 4-12 diastolic 2. PA systolic =RV pressure 3. Increased PAP a. increased systolic in pulmonary HTN b. increased diastolic from ventricular failure 4. Decreased PAP a. hypovolemia b. shock I. Pulmonary Artery Wedge Pressure 1. 2. 3. 4. Reflects preload of the LV or LVEDP Is equal to PA diastolic if no pulmonary problems Normal is 6-12mm Hg (<12mmHg) Decreased wedge a. low stroke volume b. hypovolemia 5. Increased wedge a. left ventricular failure b. mitral valve problems c. hypervolemia Hemodynamic Monitoring Study Questions 1. 1. What does CVP measure and what is a normal CVP? What would this mean in the care of my clients? ~ CVP is a measure of blood volume and venous return. It reflects RIGHTSIDED filling pressures. It is primarily used to monitor fluid volume status. ~ Normal range for CVP is 2-8 mmHg ~ Hypovolemia and shock DECREASE the CVP. Fluid overload, vasoconstriction, and cardiac tamponade INCREASE CVP. ~ If CVP is decreased, client needs fluid to increase preload. If CVP is increased, client needs diuresis, vasodilation to decrease afterload, or treatment for cardiac tamponade! 2. 2. What is a PA catheter; what does a PA catheter measure, and where is it placed? ~ A PA catheter is a flow-directed, balloon-tipped catheter, a.k.a. the SwanGanz. PA = pulmonary artery. ~ A PA catheter measures pressures in the right atrium, pulmonary artery, and left ventricle. It is used to evaluate left ventricular and overall cardiac function. ~ It is inserted into a central vein and threaded into the right atrium. A small balloon allows the catheter to be drawn into the right ventricle and from there into the pulmonary artery. Once in place, the balloon is deflated and the multiple lumens of the catheter allow measurement of pressures in the right atrium, pulmonary artery, and left ventricle. 3. 3. What is a normal PA pressure and under what conditions would a PA pressure be increased? What does it mean in the care of my clients? ~ Normal PA is around 25/10 mmHg. Normal mean pulmonary artery pressure is about 15 mmHg. ~ Pulmonary artery pressure is increased in left-sided heart failure. Manifestations of left-sided heart failure result from pulmonary congestion and decreased cardiac output. PA pressure measurement allows restoration of fluid balance while avoiding overcorrection of the problem. Nursing interventions for heart failure would be appropriate. 4. 4. What is PAWP (PCWP or PWP); what does it measure and what does this value mean? How does it relate to the Left Ventricular End Diastolic Pressure (LVEDP)? ~ PAWP is pulmonary artery wedge pressure. It measures pressures generated by the left ventricle. It is used to assess left ventricular function. Normal PAWP is 6-12 mmHg. PAWP is increased in left ventricular failure and pericardial tamponade. It is decreased in hypovolemia. ~ PAWP reflects LVEDP under normal conditions, that is, when LVEDP (ventricular preload) is increased, PAWP is increased also. 5. 5. How is PAWP obtained? The measurement of PAWP is obtained by slowly inflating the balloon with 1.5 mL of air while observing the distal lumen pressure tracing. As the line becomes “wedged,” the tracing changes shape and amplitude. When the tracing changes from arterial to atrial, the catheter is said to be wedged and PAWP is measured at the end of expiration. 6. 6. What is cardiac output/cardiac index and what do these values mean? What is normal cardiac output/cardiac index? ~ Cardiac output/cardiac index are used to assess the heart’s ability to meet the body’s oxygen demands. Because body size affects overall cardiac output, the cardiac index is a more precise measurement of heart function. ~ The cardiac index is a calculation of cardiac output per square meter of body surface area. The normal cardiac index is 2.2-4.0 L/min/m2. CO = SV x HR. Normal resting CO is 4-8 L/min and varies with body size. 7. 7. What is SVR; How is it determined? What is MAP? ~ SVR is systemic vascular resistance. SVR is primarily determined by vessel diameter and distensibility (compliance.) Factors such as SNS input, circulating hormones (epinephrine, norepinephrine, atrial natriuretic hormone, and vasopressin) and the reninangiotensin system affect SVR. ~ SVR is calculated by: SVR = (MAP – CVP) x 80/cardiac output * MAP is mean arterial pressure is the amount of arterial that is necessary to maintain adequate perfusion of vital organs…usually 60 mmHg and is calculated by Systolic BP + 2 (Diastolic BP) divided by 3








