1 - Université Lille 2 Droit et Santé
advertisement

-1-
Characterization of Discriminant Human Brain Antigenic
Targets
in
Neuropsychiatric
Systemic
Lupus
Erythematosus using an Immunoproteomic Approach
Didier Lefranc,1* David Launay,1,2* Jérôme de Seze,1,3 Sylvain Dubucquoi,1 Patricia Dussart,1
Marie Vermersch,1 Eric Hachulla,2 Pierre-Yves Hatron,2 Patrick Vermersch,1,3 and Lionel
Prin1
1
Didier Lefranc, MD, PhD, David Launay, MD, Jérôme de Seze, MD, PhD, Sylvain
Dubucquoi, MD, Patricia Dussart, Marie Vermersch, Patrick Vermersch, MD, PhD, Lionel
Prin, MD, PhD: Laboratoire d’Immunologie EA2686, IMPRT IFR 114, Faculté de Médecine,
1, Place de Verdun, 59045 Lille Cedex, France; 2David Launay, MD, Eric Hachulla, MD,
PhD, Pierre-Yves Hatron, MD: Service de Médecine Interne, Hôpital Claude-Huriez,
Université Lille 2; CHRU Lille; 1, Place de Verdun, 59037 Lille Cedex, France; 3Patrick
Vermersch, MD, PhD: Service de Neurologie D, Hôpital Roger Salengro, Université Lille 2;
CHRU Lille; 59037 Lille Cedex, France.
Address correspondence and reprint requests to Didier Lefranc, MD, PhD, Laboratoire
d’Immunologie, Faculté de Médecine – Pôle recherche, 1 Place de Verdun, 59045 Lille
Cedex, France. Tel.: +33 3 20 62 68 61; Fax: +33 3 20 62 68 93. E-mail: d-lefranc@chrulille.fr.
* the first two authors contributed equally to this work.
-2Abstract
Objective.
neuropsychiatric
To characterize discriminant human brain
systemic
lupus
erythematosus
(NPSLE)
antigenic targets in
using
a
standardized
immunoproteomic approach.
Methods. Serum self-IgG reactivities against normal and injured human brain tissues
were studied by western blotting in sera from 160 subjects, including 7 patients with NPSLE,
12 patients with SLE without neuropsychiatric manifestations (noNPSLE), 32 patients with
Sjögren’s syndrome with or without central nervous involvement, 82 patients with multiple
sclerosis and 27 healthy subjects. A proteomic approach was then applied to characterize
discriminant antigens identified after comparisons of all patterns.
Results. The serum self-IgG reactivity patterns against human brain tissue differed
significantly between patients with NPSLE and the control groups. Four normal brain
antigenic bands were specifically or preferentially recognized by sera from NPSLE patients
(p240, p90, p77, p24). The protein band p240 was characterized as microtubule-associated
protein (MAP)-2B, p77 as HSP 70-71 and p24 as triosephosphate isomerase. The protein band
p90 was not characterized. In contrast, one other protein band (p56, characterized as septin 7)
was never recognized by sera from NPSLE patients but was recognized by a majority of sera
from patients with noNPSLE.
Conclusion. This study shows that the immunoproteomic approach is a reliable
method to assess the serum self-IgG reactivities against human brain tissue in NPSLE. The
characterization of some identified discriminant antigens, such as p240, p24 and p56, suggests
that the stability of neuronal microtubules might be involved in the pathophysiology of
NPSLE.
-3Keywords: systemic lupus erythematosus; neuropsychiatric disorders; immunology;
proteomic;
-4Systemic lupus erythematosus (SLE) is a chronic autoimmune disease characterized by
multisystemic manifestations. Central nervous system (CNS) involvement has been reported
to occur in 14% or up to 95% of SLE cases depending of the criteria applied (1;2) and could
account for between 4% and 16% of deaths in SLE. The features of neuropsychiatric SLE
(NPSLE) are extremely diverse, including neurological and psychiatric syndromes. In 1999,
the American College of Rheumatology (ACR) Ad Hoc Committee on Neuropsychiatric
Lupus Nomenclature provided case definitions for 19 different neuropsychiatric syndromes
seen in patients with SLE (3). Diagnosis of NPSLE is difficult and remains a challenge
because drugs used in lupus management, infections or other non SLE-related pathological
conditions may be responsible for the neuropsychiatric manifestations in SLE and have to be
excluded. Moreover there is no “gold standard” investigation or diagnostic test to definitively
confirm NPSLE, which remains a largely clinical diagnosis (4). As the treatment is obviously
dependent of the underlying cause, many authors have underlined the need for new diagnostic
tools in NPSLE (4-6).
There are some lines of evidence that the autoimmune system plays a role since
NPSLE typically occurs in the presence of serologically and clinically active lupus (7).
However, while it is well established that autoantibodies can directly damage organs,
especially the kidney, the skin and the fetal heart (8), the brain molecular targets have not
been fully identified in NPSLE. Several investigators have sought to identify autoantibodies
that could bind directly to neurons in NPSLE and could serve as diagnostic markers in
NPSLE. A subset of anti-dsDNA antibodies from SLE patients were recently shown to crossreact with NR2 N-methyl-D-aspartate (NMDA) receptors in the CNS and to have the
functional capacity to cause neuronal death by excitotoxicity and apoptosis in vivo and in
vitro (9-11). IgG anti-NR2 glutamate receptor antibodies detected in cerebrospinal fluid were
reported to be associated with NPSLE in some studies (12). Other studies, however, found no
-5association
between
these
antibodies
and
cognitive
dysfunction
in
SLE
(13).
Antineurofilament antibodies have been found in NPSLE, particularly in patients with diffuse
subcortical white matter lesions (14). Recently, sera collected from patients with SLE were
tested for the presence of antibodies to microtubule-associated protein 2 (MAP-2), which
were particularly detected in NPSLE patients (15). Nevertheless, whether or not there is an
alteration of the immune recognition of brain self-proteins in NPSLE still requires further
investigation (5). Moreover, most of the previous studies employed techniques using purified
self-antigens and/or relevant peptides from pre-selected targets. To avoid a restricted analysis
with pre-selected antigenic targets, we chose to assess the global serum self-IgG reactivity
against healthy or injured human brain tissue extracts. In a previous study we found that the
serum self-reactive IgG antibody repertoire against such targets was different between
patients with multiple sclerosis (MS), patients with Sjögren’s syndrome (SS) and healthy
subjects and could help to identify brain antigen targets with a potentially important
diagnostic and pathophysiological role in MS (16).
Using a western blotting method and without any a priori assumptions, we compared
the serum self-IgG reactivities against human brain tissue extracts in NPSLE patients and in
control groups (patients with SLE but no neuropsychiatric manifestations [noNPSLE];
patients with SS with [SSCNS] and without [SSnoCNS] CNS involvement; patients with MS;
and healthy subjects). Then, using a proteomic approach, we characterized the most
discriminant brain antigenic targets in NPSLE. We confirmed previous results concerning the
presence of anti MAP-2 and anti triosephosphate isomerase antibodies in NPSLE and
characterized 2 other discriminant antigenic targets: HSP 70-71 and an unidentified p90
antigenic band. This characterization emphasizes the possible role of neuronal microtubules in
the pathophysiology of NPSLE.
-6PATIENTS AND METHODS
Patients. IgG antibody responses to brain tissues were studied in sera from 160
subjects. The SLE group included 19 patients who had definite SLE according to the 1997
updated American College of Rheumatology (ACR) criteria for classification of SLE (17) and
were followed up in the Department of Internal Medicine. Among the 19 SLE patients 7
presented NPSLE fulfilling the case definitions for NPSLE proposed by the ACR (3) and 12
had no evidence of neuropsychiatric manifestations (noNPSLE). Patients having clinically
active disease related to antiphospholipid syndrome were not included in this study. Thirtytwo patients had SS according the European revised criteria (18). Among them, 26 had CNS
involvement (SSCNS) and 6 had no CNS involvement (SSnoCNS). All SS patients were
followed up in the Department of Neurology. Eighty-two patients were diagnosed with MS
according to the criteria of McDonald et al. (19). All MS patients were followed up in the
Department of Neurology and were relapse free. Sera from 27 healthy subjects were tested as
normal controls. Presence of anti-DNA antibodies was assessed by Farr assay (Amerlex antidsDNA radioimmunoassay kit; Trinity Biotech, Bray, Ireland) and expressed in IU.
Antiphospholipid antibodies were evaluated by ELISA (ORGENTEC Diagnostika GmbH,
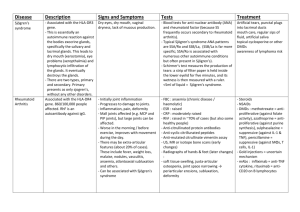
Mainz, Germany) with a cut-off value of 10 for IgG and 7 for IgM. Table 1 summarizes the
epidemiological parameters of the SLE group, SS and MS patients and controls. Table 2
details the characteristics of the NPSLE patients. All subjects gave their written informed
consent, and the study was approved by the local ethics committee.
Brain samples. Brain samples, dissected out at autopsy from the frontal lobe in
Brodmann’s area 10, were obtained from an MS patient (a 48-year-old man) and from a 68year-old man with no history of neurological disease (Department of Neuropathology, CHU
de Lille and INSERM U422, Lille, France). The 68-year-old man died as a result of an acute
-7myocardial infarction. The autopsies were performed within the framework of a tissuecollection program that was approved by the local ethics committee. In each case, the postmortem delay was less than 8 hours.
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis. The brain samples
were homogenized in a Tris buffer containing 5% sodium dodecyl sulfate (SDS) at a final
concentration of 10 mg/ml and heated at 95°C for 10 minutes; for each well, 80 µl of this
lysate was loaded onto a 10 to 20% gradient polyacrylamide gel, beside a molecular weight
marker (Amersham Pharmacia Biotech, Uppsala, Sweden). Just before electrophoresis, the
homogenates were reduced with 10 mM dithiothreitol (Sigma, St Louis, MO). Electrophoresis
was conducted for 14-16 hours in Laemmli buffer at 100 V (20).
Two-dimensional electrophoresis (2-DE). The brain sample homogenization and the
1-D protein separation were done essentially as previously described (16). Briefly, 100 mg of
brain tissue were homogenized in a detergent solution (4% Triton X100, 1X anti-protease
cocktail (Sigma, St Louis, MO) before protein precipitation using three volumes of ice-cold
acetone. The sample was centrifuged at 10,000 g, 4°C for 20 min. The supernatant was
removed and the pellet was air dried. Before electrophoresis, the pellet was resuspended in
500 µl of sample buffer (7 M urea, 2 M thiourea, 1% DTT, 4% Triton X100 (Sigma, St Louis,
MO), 1X anti-protease cocktail (Sigma, St Louis, MO) and 2% v/v ampholines (Amersham
Pharmacia Biotech, Uppsala, Sweden). After dissolution, the samples were used for overnight
in-gel rehydratation. Proteins were separated using the MultiPhor II (Amersham Pharmacia
Biotech) with anode (10 mM H3PO4) and cathode (10 mM NaOH) buffers. The firstdimension IEF program was as follows: 150 V, 1 h; 300 V, 1 h; 1000 V, 1 h; and 3500 V until
-8a minimum Vh product of 90 kVh was reached. After termination, the IPG strips were stored
at –70 °C until further use.
Prior to the second dimension, the IPG strips were equilibrated for 2 x 30 min in 2 mL
equilibration solution I (50 mM Tris-HCl, pH 8.8, 8 mM EDTA 10% w/v glycerol, 5% w/v
SDS, 1% w/v DTT) and 1 x 30 min in 2 ml of equilibration II (50 mM Tris-HCl, pH 8.8, 8
mM EDTA 10% w/v glycerol, 5% w/v SDS, 150 mM iodoacetamide). Equilibrated IPGs
were transferred to 9-16% or 10-20% polyacrylamide gradient gels containing the cross-linker
piperazine diacrylamide (C=2.6%; Bio-Rad) (21). Gels were polymerized overnight.
Electrophoresis was performed for 14-16 hours in a BioRad Protean II xi chamber (Bio-Rad,
Hercules, CA) with current limited to 40 mA per gel. For the identification of the antigens a
preparative 2-DE gel was stained with Coomassie Brilliant Blue (CBB) G-250 (preparative
gel) (Sigma, St Louis, MO) and then used for spot cutting and protein sequencing.
Western blotting and analysis procedures. For immunostaining, 1-DE or 2-DE gels
were blotted onto Hybond-P PVDF membranes (Amersham Pharmacia Biotech Europe
GmbH, Saclay, France) using a “semi-dry” protocol (0.8 mA per cm²) (22) and later saturated
with 5% non-fat dried milk. Western blotting was carried out with total sera, diluted 1/100 in
Tris buffer saline (TBS: 100 mM Tris, pH 8.0; NaCl 0.3 M) containing 0.5% Tween20 (w/v)
and 5% non-fat dried milk. After incubation for 1 night at 4°C, the IgG antibodies were
revealed with an anti-human Fc horseradish peroxidase conjugated antibody 1/10,000
(Sigma, St Louis, MO). Fluorograms were prepared using an enhanced chemiluminescence
kit (Amersham Pharmacia Biotech Europe GmbH). Immune profiles were analyzed when two
independent assays had produced identical patterns. Image analysis was performed on a GS800 calibrated densitometer (Biorad, Hercules, CA) apparatus to localize and compare the
IgG immune profile patterns. Superimposition and alignment of the antibody reactivities was
-9performed using Diversity database fingerprinting software version 2.2 (Biorad, Hercules,
CA) for 1-DE and PDQuest software (Bio-Rad) for 2-DE. We performed comparative
analysis using detection parameters that allowed us to consider as significant each band
intensity higher than 10% of global background intensity. In order to calibrate and define
more accurately the alignment of antibody reactivities, molecular weight marker proteins
(LKB Pharmacia molecular weight standards) as well as internal references were used.
Antibodies directed against several known proteins (alpha enolase (TEBU, ref: sc-7455),
glyceraldehyde 3-phosphate dehydrogenase: GAPDH (CHEMICON, ref: MAB374) and glial
fibrillary acidic protein: GFAP (Sigma, St Louis, MO; ref:G-3893), were used as landmarks
to secure superimposition and to facilitate rapid and better gel matching. Antigenic bands
were numbered by using their molecular weight preceded by the letter p if they were on
normal CNS or P if they were on MS CNS.
In-gel digestion and MALDI-TOF-MS analysis. Excised plugs from CBB-stained
gels were destained with 200 µL 50% acetonitrile in 10 mM NH4HCO3 and dried in a
SpeedVac concentrator. Protein was digested overnight at 37°C by sequencing grade trypsin
(5 µg/mL; Promega Madison, WI) in 50 mM NH4HCO3. The resulting peptides were
extracted twice with 25 µL 50% acetonitrile/0.1% TFA. The collected extracts were
lyophilized, and were resuspended in 10 µL 0.1% TFA and desalted on ZipTip C18microcolumns (Millipore, Bedford, MA). Elution was performed with -cyano-4hydroxycinnamic acid (5 mg/mL) directly onto the MALDI target (2 µL of the solution were
applied to a plated sample holder and introduced into the mass spectrometer after drying).
MALDI-TOF-MS was used to obtain mass fingerprinting for proteins using a Voyager DESTR instrument (Applied Biosystems, Framingham, MA). Ions were accelerated at 20 kV and
reflected at 21.3 kV. Spectra were acquired in the delayed extraction reflectron R mode. 100-
- 10 300 scans were averaged to produce final spectra. Spectra were externally calibrated using the
monoisotopic MH+ ion from three peptide standards (trypsin autodigestion products: 842.510,
1045.564 and 2211.1046 Da.).
Database search based on peptide mass fingerprint spectra. The obtained peptide
mass fingerprint spectra were analyzed by searching the National Centre for Biotechnology
Information
(NCBI)
nonredundant
protein
database
with
ProFound
(http://prowl.rockefeller.edu/cgi-bin/ProFound) Version 3.2 and verified using the Mascot™
search engine (http://www.matrixscience.com). The parameters for each search were varied in
order to achieve the best possible results. The standard parameters were as follows: Homo
sapiens, 0-250 kDa molecular mass (depending on the region where the spot occurred in gel),
tryptic digest with a maximum number of one missed cleavage. Peptide masses were stated to
be monoisotopic, and methionine residues were assumed to be partially oxidized. The identity
of proteins was annotated using the SWISS-PROT and TrEMBL database.
Statistical analysis. The data were expressed in binary mode (0 = absence of antigenic
band; 1 = presence of an antigenic band) in order to submit IgG antibody patterns to analysis
using either the Chi Square or Fisher exact test. This approach allowed us to select the most
relevant antigens that supported qualitatively different immune recognition. In a second stage,
we used linear discriminant analysis (LDA) to balance the discriminating antigens between
the populations of individuals, as previously detailed (16;23). Using a stepwise logistic
regression model and supported by the LDA method, we were able to isolate a sub-group of
brain antigens related to their strength of discrimination between the different populations
involved in the study.
By associating two parameters, for the presence (x 1) or absence (x 0) of each selected
antigen, and the coefficient previously defined by the LDA, a score was calculated for each
- 11 subject as a representative value of the individual immune profile, using the following
formula:
Score = Ag1coef1 x {0(absent) or 1(present)}+ Ag2coef2 x {0(absent) or 1(present)} + Ag3coef3...
Statisticians calculated all the scores blindly. The calculated scores were represented
graphically. A threshold value was determined using a receiver operating characteristic
(ROC) curve, and the sensitivity and specificity of this approach were evaluated. When the
number of patients was too small to apply LDA, Chi-Square and Fisher tests were performed.
RESULTS
Comparison of serum self-IgG reactivities in patients with autoimmune diseases
with or without CNS involvement, in MS patients and in healthy subjects. In a first step,
the degree of interindividual changes in serum self-IgG reactivities against MS and healthy
brain tissue was evaluated. This analysis was successively performed in patients with NPSLE,
noNPSLE, SSCNS, SSnoCNS and MS as well as in healthy subjects. A high degree of
heterogeneity in the IgG reactivities was found within a given group or between the different
groups of tested subjects with regard to the number and the nature of the antigenic bands
recognized by serum IgG. Quite different patterns were also observed when a given serum
was tested against healthy brain (normal CNS) or MS brain tissue (MS CNS). However,
despite this high degree of heterogeneity, we observed some conserved sets of IgG reactivities
against normal and MS CNS within a same group of subjects as well as between the different
groups. Figure 1 illustrates both the diverse and the common self-IgG reactivities within and
between the different groups of tested subjects. Quantitative changes were also noted when
patterns obtained either against normal CNS (n = 160) or MS CNS (n = 160) were compared.
Sera of patients with autoimmune diseases (NPSLE, noNPSLE, SSCNS and SSnoCNS)
recognized significantly fewer normal and MS CNS antigens than patients with MS and
- 12 healthy subjects. However, there was no significant difference in the number of antigenic
bands recognized by sera from MS patients and the number recognized by sera from healthy
subjects (Table 3).
Despite the qualitative and quantitative changes in self-IgG patterns, comparative
studies were performed between patients with autoimmune diseases (NPSLE, n = 7;
noNPLSE, n = 12; SSCNS, n = 26; SSnoCNS, n = 6), MS patients (n = 82) and healthy
subjects (n = 27). The mapping and alignment of 160 strips obtained either with normal CNS
or with MS CNS were then assessed. As illustrated in Figure 2A, LDA enabled us to identify
16 discriminant IgG reactivities against antigenic bands ranging from 16 to 140 kDa. They
included 12 protein bands on normal CNS (p140, p112, p105, p90, p85, p70, p66, p55, p53,
p50, p32 and p28) and 4 protein bands on MS CNS (P42, P39, P36, P16). The coefficient
values assigned by LDA for each discriminant antigenic band associated with the presence or
the absence of these antigens enabled us to calculate graphic coordinates for each individual.
The score assigned to each patient with an autoimmune disease, each MS patient and each
healthy subject revealed clear distinctive areas for each group (Figure 2B) with an excellent
degree of concordance with clinical data ( = 0.931).
Comparison of serum self-IgG reactivities in patients with autoimmune diseases
with or without neurological manifestations. Self-IgG reactivity against MS or normal CNS
was compared between patients with autoimmune diseases according to the presence
(NPSLE, n = 7; SSCNS, n = 26) or the absence (noNPSLE, n = 12; SSnoCNS, n = 6) of
neurological manifestations. Mapping and alignment of the 51 immunoreactive patterns
allowed us to compare the obtained self-IgG patterns between these 2 groups. As illustrated in
Figure 3, LDA found 5 protein bands (2 in normal CNS [p113 and p32] and 3 in MS CNS
[P66, P38 and P11]), which were highly discriminant between the self-IgG patterns of patients
with autoimmune diseases according to the presence or the absence of neurological
- 13 manifestations. Figure 3A shows these 5 antigenic bands and their frequencies in the 2
subgroups of patients. Two antigenic bands, p113 and P38, were only recognized by sera from
patients with autoimmune diseases with neurological manifestations. P66 was more frequently
recognized by sera from patients with autoimmune diseases having neurological
manifestations. Conversely, antigenic bands p32 and P11 were more frequently recognized by
sera from patients without neurological manifestations. A global score was then calculated for
each patient taking into account a coefficient value assigned by LDA for the 5 selected bands.
A graphic extrapolation of LDA on a single axis graph shows that patients with autoimmune
diseases with neurological manifestations (NPSLE or SSCNS) projected very distinctively
from those with autoimmune diseases but without neurological manifestations (noNPSLE or
SSnoCNS) with a sensitivity of 96.9% and a specificity of 94.5%) (Figure 3B). There was an
excellent degree of concordance with the clinical data ( = 0.960).
Comparison of serum self-IgG reactivities between patients with NPSLE,
noNPSLE and SSCNS. To further evaluate the significance of the patterns obtained with sera
from NPSLE patients we compared them to the patterns obtained in SLE without CNS
involvement (noNPSLE) and in another autoimmune disease with CNS involvement
(SSCNS). Because of the small number of patients in each group, LDA was not applicable
and Chi-square and Fischer tests were performed. Comparison of self-IgG patterns between
NPSLE and SSCNS patients revealed 8 discriminant antigenic bands only detected on normal
CNS (p240, p113, p112, p90, p77, p65, p56, p24) (Figure 4A). In terms of frequency, 5 of
these 8 bands were more often found in NPSLE patients (p240, p90, p77, p65 and p24).
Conversely, 3 of these 8 bands (p113, p112 and p56) were only recognized by patients with
SSCNS. Comparison of self-IgG patterns between NPSLE and noNPSLE revealed 9
discriminant antigenic bands detected either on normal CNS (p240, p126, p90, p77, p56, p37,
p32) or on MS CNS (P66, P39) (Figure 4B). The antigenic band p24 just missed statistical
- 14 significance as it was recognized by 3/7 (42.8%) patients with NPSLE, vs. 1/12 (8.3%)
patients with noNPLSE (P = 0.06). In terms of frequency, 3 bands were only found in NPSLE
patients (p126, p90 and p77), 4 bands were more often found in NPSLE patients (p240, p37,
P66, P39 and p24) and 2 bands were never found in NPSLE (p56 and p32). Taken together
(Figures 4 A and B), these data show that some antigenic bands only detected on normal CNS
were more frequently found in NPSLE (p240, p90, p77 and p24) or never found in NPSLE
(p56). p32, which was never recognized in NPSLE, was always found in noNPSLE and
occasionally found in SSCNS (11.5%). Table 4 shows which discriminant antigens were
recognized by each patient with NPSLE.
Characterization of the major discriminant antigens using a serologic proteomic
approach (SERPA). To further characterize discriminant antigens more frequently targeted
by sera from NPSLE patients (p240, p90, p77 and p24) or never detected by NPSLE patients
(p56), we used a SERPA. Identification of discriminant proteins was firstly performed by
comparison of 1-D immune and 2-D immune patterns. The 7 NPSLE sera were used to
identify antigenic candidates on a proteomic map obtained after 2-DE performed with normal
and MS CNS. The 2-DE followed by immunoblotting assays revealed the presence of
multiple antigenic spots (Figures 5A and B). Then, the superimposition of antigenic spots and
protein spots revealed by a standard colloidal Coomassie blue stained 2-DE enabled us to
select the proteins (Figure 5C) for further in-gel digestion and MALDI-TOF analysis as
previously described, on the basis of peptide mass matching (24). This approach allowed us to
identify some proteins as potent discriminant antigens using the SWISS-PROT database
(Table 5). Antigens p240 and p77 were characterized as the MAP-2B (MAP2_HUMAN,
P11137) and HSP 70-71 (HSP7C-HUMAN, P11142), respectively. p24 was identified as
triosephosphate isomerase (TRPIS_HUMAN, P60174). The protein spot corresponding to
- 15 antigenic band p90 could not be characterized by mass spectrometry in spite of repeated
assays. p56 was identified as septin 7 (SEPT7-HUMAN, Q16181).
DISCUSSION
To identify potentially relevant self-antigens in brain tissues, specifically targeted by
the serum self-IgG antibody repertoire in NPSLE, we applied an immunoproteomic approach,
previously standardized in our laboratory (16;25;26). To our knowledge, this is the first study
in NPSLE to assess, without any a priori assumptions, the serum self-IgG reactivities against
human brain tissue. It might therefore be expected to answer previous questions about the
significance of antibodies found in this disease (5). Proteins from healthy or injured brain
tissues were respectively used as targets. As injured brain tissue, MS CNS was chosen instead
of NPSLE CNS, which was unavailable during the present study.
Our analysis of IgG isotype antibodies allowed us to evaluate both the natural selfreactive responses (27) and the T-cell dependent adaptive humoral responses (28). In spite of
a high degree of heterogeneity in serum self-IgG response when all strips were mapped and
aligned, we found some conserved sets of IgG reactivities in healthy subjects as in patients.
Such conserved protein antigens possibly targeted by natural autoantibodies might reflect a
“footprint” of the innate immune system (27;29). The natural B- and T-cell self-reactive
repertoire is now recognized as determinant for the homeostasis of lymphoid cells and the
maintenance of self-tolerance (28). Unstable patterns of antibody repertoires, possibly related
to adaptive immune response, have been described in systemic autoimmune diseases such as
SLE (30). However, discriminant stable self-IgG patterns, probably related to pathogenic
events, were found in organ specific autoimmune disease such as MS, after one year of
follow-up (25). To define more precisely the significance of such stable and unstable changes
with regard to the pathological context, we compared the respective self-IgG responses
- 16 obtained in healthy subjects and patients with systemic or organ specific autoimmune
diseases, against healthy or injured brain tissues.
In a first step, we found reactivities towards 16 discriminant antigens when patterns
with sera from healthy subjects and MS, SS, and SLE patients with or without CNS
involvement were compared. Eleven of these 16 antigens had already been identified in our
previous study where only MS, SSCNS and healthy subjects were compared (16). Five new
antigenic targets were found in the present study when SLE and SSnoCNS patients were
included. Thus, organ-specific autoimmune diseases such as MS as well as systemic
autoimmune diseases such as SLE are associated with distinct serum changes in self-IgG
antibody repertoires against brain antigens. We also tested the hypothesis that the presence or
absence of CNS involvement could also shape the serum self-IgG patterns. We showed that
protein bands targeted by serum self-IgG antibodies allowed autoimmune diseases to be
differentiated according to the presence or absence of neurological symptoms. Some protein
bands were exclusively or frequently found when sera from SLE and SS patients with CNS
involvement were tested (p113, P38 and P66) whereas other protein bands were preferentially
found with sera from SLE and SS patients without CNS involvement (p32 and p11). In
NPSLE, some antigenic bands were either never recognized (p56) or often detected (p240,
p90, p77 and p24). This could be related to neuropathogenic or neuroprotective events (31).
The absence of detection of some serum IgG antibodies in patients with systemic autoimmune
diseases might be related to a defect in regulatory processes and explain the fewer antigenic
bands recognized compared to those found in MS patients and healthy subjects. However, the
presence of antibodies restricted to sera from NPSLE patients suggests a possible pathogenic
involvement. To try to define more precisely the significance of such changes, some of the
protein bands were characterized.
- 17 First, an antigenic band never detected in NPSLE (p56) was characterized. The protein
band p56 was identified as septin 7. Septins comprise a eukaryotic subfamily of guanine
nucleotide binding proteins and may play a conserved role in cytokinesis, exocytosis and
apoptosis in yeast and mammalian cells (32). Septins were found to regulate microtubule
stability through interaction with the microtubule-binding protein MAP4 (33). Septins have
the ability to block MAP4 binding to microtubules and thus reduce their stability (33).
Interestingly, antibody response against Nedd5, which belongs to the septin family and also
interacts with microtubules, was found in NPSLE (34). IgG antibody response against septin 7
was previously identified by using normal sera on healthy brain (25). The absence of antibody
response against septin 7 in NPSLE might reflect either the loss of pathogenic antibodies
linked to altered brain tissue or the absence of regulatory antibodies required for the
maintenance of self tolerance or neuroprotection. The latter hypothesis, involving
neuroprotective antibodies (31), has already been proposed in SLE (35;36).
Second, four antigenic bands were more frequently (p240, p90, p24) or exclusively
(p77) detected in normal CNS with sera from NPSLE patients. Such results were obtained
when patterns found with sera from NPSLE patients were successively compared to patterns
found with sera either from noNPSLE patients (comparative studies in SLE with or without
CNS involvement) or from SSCNS patients (comparative studies in distinct diseases having
CNS involvement). The more frequent presence of some IgG reactivities found with sera from
NPSLE patients suggests a possible specific pathogenic implication. Previous data have
demonstrated a potential neuropathogenic role of circulating IgG antibodies in animal models
and in cell cultures (11). Moreover, an IgG fraction of cerebrospinal fluid from NPSLE
patients revealed cytotoxic properties against proliferating brain cells (37). We failed to
identify p90 antigen because it remained uncharacterized in mass spectrometry in spite of
repeated assays. The protein bands p240, p77, and p24 were characterized as MAP-2B, HSP
- 18 70-71 and triosephosphate isomerase, respectively. MAP-2B is restricted to neurons. It
controls cytoskeletal integrity by stabilizing microtubules and is involved in the elaboration of
the neuritic compartments (38). In adult neurons, microtubules are enriched in MAP-2B in
dendrites and seem to exert a stabilizing effect on the dendritic morphology since its
suppression or degradation was correlated with dendritic loss or remodeling (39). Thus,
antibodies against MAP2 could modulate neuronal plasticity. Triosephosphate isomerase is a
highly conserved glycolytic enzyme present in all cells and expressed in brain at a high level
(40). It has been shown that inhibition of this key enzyme affects microtubule stabilization
(40) and leads to neuronal death in cultured murine cortical cells (41). Whether or not antitriosephosphate isomerase antibodies have a potential pathogenic role of in NPSLE remains
unclear. On the one hand, it has been proposed that triosephosphate isomerase–antitriosephosphate isomerase immune complexes could initiate complementary cascades near the
choroid plexus, thereby causing brain damage (42). On the other hand, it has been suggested
that binding of anti-triosephosphate isomerase antibodies could result in inhibition of enzyme
activity. A defect in this enzyme activity was found to be associated with neurological
symptoms (43). Thus, it could be hypothesized that anti-triosephosphate isomerase antibodies
present in sera from NPSLE patients could lead to a sustained inhibition of triosephosphate
isomerase, leading in turn to neuropsychiatric disorders in NPSLE. Whatever the pathogenic
or regulatory role of anti-MAP2 and anti-triosephosphate isomerase antibodies, they have
recently been identified as good markers of NPSLE (15;42). In previously published data, no
association has been reported between NPSLE and anti-HSP 70-71 antibodies. An elevated
expression of a member of the HSP 70 family has been described in SLE (44). Recent reports
suggest that HSP 70 promotes antigen presentations of autoantigens and converts T-cell
tolerance to autoimmunity in vivo, and therefore has immunostimulatory properties (45). HSP
70 can also induce cytotoxic responses (46). In contrast, HSP 70 overexpression in brain has
- 19 been associated with neuroprotective effects after cerebral injury (47). A similar frequency of
autoantibodies against HSP 70 was found in SLE patients and in healthy subjects (48)
whereas we found a higher frequency of such antibodies in NPSLE patients. Anti-HSP 70-71
antibodies have also been reported in the cerebrospinal fluid of MS patients as well as in that
of patients with schizophrenia (49;50). The latter findings thus also indicate a possible
relationship between CNS involvement and detectable antibodies against HSP70-71, though
without prejudging their pathogenic or neuroprotective role.
In conclusion, the immunoproteomic approach appears to be a reliable method to
study the self-IgG antibody repertoires against brain antigens in patients with NPSLE. It
confirmed recent reports by showing that MAP-2B and triosephosphate isomerase are brain
antigenic targets in NPSLE (15;42;51). Conversely, anti-septin 7 antibodies were never
observed in patients with NPSLE. Interestingly, MAP-2B, triosephosphate isomerase and
septin 7 are together involved in neuronal microtubule stability, suggesting a role of
microtubules in the pathophysiology of NPSLE. We also found 2 new potent brain antigenic
targets: HSP70-71 and an unidentified p90 antigenic band. Our approach suggests that the
combination of IgG antibody responses against a cluster of antigens may be more determinant
than a single response, as previously suggested (16). Interestingly, the four discriminant
antigenic bands were found in one of the two patients with biological markers of
antiphospholipid syndrome without clinical manifestations of thrombosis. The diagnosis and
the pathophysiological roles of these antibodies in NPSLE merit further studies. We plan to
corroborate this hypothesis in a broader population using homemade proteo-chips with
discriminant proteins synthesized in vitro.
- 20 REFERENCES
1. Brey RL, Holliday SL, Saklad AR, Navarrete MG, Hermosillo-Romo D, Stallworth CL
et al. Neuropsychiatric syndromes in lupus: prevalence using standardized definitions.
Neurology 2002; 58:1214-1220.
2. Ainiala H, Hietaharju A, Loukkola J, Peltola J, Korpela M, Metsanoja R et al. Validity
of the new American College of Rheumatology criteria for neuropsychiatric lupus
syndromes: a population-based evaluation. Arthritis Rheum 2001; 45:419-423.
3. The American College of Rheumatology nomenclature and case definitions for
neuropsychiatric lupus syndromes. Arthritis Rheum 1999; 42:599-608.
4. Hanly JG, Harrison MJ. Management of neuropsychiatric lupus. Best Pract Res Clin
Rheumatol 2005; 19:799-821.
5. Senecal JL, Raymond Y. The pathogenesis of neuropsychiatric manifestations in
systemic lupus erythematosus : a disease in search of autoantibodies, or autoantibodies
in search of a disease ? J Rheumatol 2004; 31:2093-2098.
6. Trysberg E, Carlsten H, Tarkowski A. Intrathecal cytokines in systemic lupus
erythematosus with central nervous system involvement. Lupus 2000; 9:498-503.
7. Tomita M, Khan RL, Blehm BH, Santoro TJ. The potential pathogenetic link between
peripheral immune activation and the central innate immune response in
neuropsychiatric systemic lupus erythematosus. Med Hypotheses 2004; 62:325-335.
8. Buyon JP. Neonatal lupus. Curr Opin Rheumatol 1996; 8:485-490.
9. DeGiorgio LA, Konstantinov KN, Lee SC, Hardin JA, Volpe BT, Diamond B. A subset
of lupus anti-DNA antibodies cross-reacts with the NR2 glutamate receptor in systemic
lupus erythematosus. Nat Med 2001; 7:1189-1193.
10. Rice JS, Kowal C, Volpe BT, DeGiorgio LA, Diamond B. Molecular mimicry : antiDNA antibodies bind microbial and nonnucleic acid self-antigens. Curr Top Microbiol
Immunol 2005; 296:137-151.
11. Huerta PT, Kowal C, DeGiorgio LA, Volpe BT, Diamond B. Immunity and behavior :
antibodies alter emotion. Proc Natl Acad Sci U S A 2006; 103:678-683.
12. Yoshio T, Onda K, Nara H, Minota S. Association of IgG anti-NR2 glutamate receptor
antibodies in cerebrospinal fluid with neuropsychiatric systemic lupus erythematosus.
Arthritis Rheum 2006; 54:675-681.
13. Harrison MJ, Ravdin LD, Lockshin MD. Relationship between serum NR2a antibodies
and cognitive dysfunction in systemic lupus erythematosus. Arthritis Rheum 2006;
54:2515-2522.
14. Bell CL, Partington C, Robbins M, Graziano F, Turski P, Kornguth S. Magnetic
resonance imaging of central nervous system lesions in patients with lupus
erythematosus. Correlation with clinical remission and antineurofilament and
anticardiolipin antibody titers. Arthritis Rheum 1991; 34:432-441.
- 21 15. Williams RC, Jr., Sugiura K, Tan EM. Antibodies to microtubule-associated protein 2 in
patients with neuropsychiatric systemic lupus erythematosus. Arthritis Rheum 2004;
50:1239-1247.
16. Lefranc D, Almeras L, Dubucquoi S, de Seze J, Vermersch P, Prin L. Distortion of the
self-reactive IgG antibody repertoire in multiple sclerosis as a new diagnostic tool. J
Immunol 2004; 172:669-678.
17. Hochberg MC. Updating the American College of Rheumatology revised criteria for the
classification of systemic lupus erythematosus. Arthritis Rheum 1997; 40:1725.
18. Vitali C, Bombardieri S, Jonssopn R, Moutsopoulos HM, Alexander EL, Carsons SE et
al. Classification criteria for Sjogren's syndrome: a revised version of the European
criteria proposed by the American-European Consensus Group. Ann Rheum Dis 2002;
61:554-558.
19. McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lunlin FD et al.
Recommended diagnostic criteria for multiple sclerosis: guidelines from the
International Panel on the diagnosis of multiple sclerosis. Ann Neurol 2001; 50:121127.
20. Laemmli UK. Cleavage of structural proteins during the assembly of the head of
bacteriophage T4. Nature 1970; 227:680-685.
21. Hochstrasse DF, Merril CR. 'Catalysts' for polyacrylamide gel polymerization and
detection of proteins by silver staining. Appl Theor Electrophor 1988; 1:35-40.
22. Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from
polyacrylamide gels to nitrocellulose sheets: procedure and some applications. 1979.
Biotechnology 1992; 24:145-149.
23. Marshall G, Baron AE. Linear discriminant models for unbalanced longitudinal data.
Stat Med 2000; 19:1969-1981.
24. Henzel WJ, Billeci M, Stults JT, Wong SC, Grimley G, Watanabe C. Identifying
proteins from two-dimensional gels by molecular mass searching of peptide fragments
in protein sequence databases. Proc Natl Acad Sci U S A 1993; 90:5011.
25. Almeras L, Lefranc D, Drobecq H, de Seze J, Dubucquoi S, Vermersch P et al. New
antigenic candidates in multiple sclerosis: identification by serological proteome
analysis. Proteomics 2004; 4:2184-2194.
26. Zephir H, Almeras L, El Behi M, Dussart P, de Seze J, Steibel J et al. Diversified serum
IgG response involving non myelin CNS proteins during Experimental Autoimmune
Encephalomyelitis. J Neuroimmunol (in press) 2006.
27. Mouthon L, Haury M, Lacroix-Desmazes S, Barreau C, Coutinho A, Kazatchkine M.
Analysis of the normal human IgG antibody repertoire. Evidence that IgG
autoantibodies of healthy adults recognize a limited and conserved set of protein
antigens in homologous tissues. J Immunol 1995; 154:5769-5778.
- 22 28. Sobel ES, Kakkanaiah VN, Kakkanaiah M, Cheek RL, Cohen PL, Eisenberg RA. T-B
collaboration for autoantibody production in lpr mice is cognate and MHC-restricted. J
Immunol 1994; 152:6011.
29. Francoeur AM, Heitzmann JG. Autoantibodies: terms and concepts. Clin Immunol
Immunopathol 1988; 47:245-252.
30. Ferreira C, Mouthon L, Nobrega A, Haury M, Kazatchkine MD, Ferreira E et al.
Instability of natural antibody repertoires in systemic lupus erythematosus patients,
revealed by multiparametric analysis of serum antibody reactivities. Scand J Immunol
1997; 45:331-341.
31. Schwartz M. Physiological approaches to neuroprotection : boosting of protective
autoimmunity. Surv Ophtalmol 2001; 45 (Suppl 3):S256.
32. Kinoshita M, Noda M. Roles of septins in the mammalian cytokinesis machinery. Cell
Struct Funct 2001; 26:667-670.
33. Kremer BE, Haystead T, Macara IG. Mammalian septins regulate microtubule stability
through interaction with the microtubule-binding protein MAP4. Mol Biol Cell 2005;
16:4648-4659.
34. MArgutti P, Sorice M, Conti F, Delunardo F, Racaniello M, Alessandri C et al.
Screening of an endothelial cDNA library identifies the C-terminal region of Nedd5 as a
novel autoantigen in systemic lupus erythematosus with psychiatric manifestations.
Arthritis Res Ther 2005; 7:R896-R903.
35. Senecal JL, Rauch J, Grodzicky T, Raynauld JP, Uthman I, Nava A et al. Strong
association of autoantibodies to human nuclear lamin B1 with lupus anticoagulant
antibodies in systemic lupus erythematosus. Arthritis Rheum 1999; 42:1347-1353.
36. Shoenfeld Y, Toubi E. Protective autoantibodies: role in homeostasis, clinical
importance, and therapeutic potential. Arthritis Rheum 2005; 52:2599-2606.
37. Sakic B, Kirkham DL, Ballok DA, Mwanjewe J, Fearon IM, MAcri J et al. Proliferating
brain cells are a target of neurotoxic CSF in systemic autoimmune disease. J
Neuroimmunol 2005; 169(1-2):68-85.
38. Maccioni RB, Cambiazo V. Role of microtubule-associated proteins in the control of
microtubule agency. Physiol Rev 1995; 75:834.
39. Sharma N, Kress Y, Shafit-Zagardo B. Antisense MAP-2 oligonucleotides induce
changes in microtubule assembly and neuritic elongation in pre-existing neurites of rat
cortical neurons. Cell Motil Cytoskeleton 1994; 27:234-247.
40. Orosz O, Wagner G, Liliom K, Kovacs J, Baroti K, Horanyi M et al. Enhanced
association of mutant triosephosphate isomerase to red cell membranes and to brain
microtubules. Proc Natl Acad Sci U S A 2000; 97:1026-1031.
41. Sheline CT, Choi DW. Neuronal death in cultured murine cortical cells is induced by
inhibition of GAPDH and triosephosphate isomerase. Neurobiol Dis 1998; 5:47-54.
- 23 42. Watanabe H, Seino T, Sato Y. Antibodies to triosephosphate isomerase in patients with
neuropsychiatric lupus. Biochem Biophys Res Commun 2004; 321:949-953.
43. Hollan S, Fujii H, Hirono A, Karro H, Miwa S, Harsanyi V et al. Hereditary
triosephosphate isomerase (TPI) deficiency: two severely affected brothers one with and
one without neurological symptoms. Hum Genet 1993; 92:486-490.
44. Dhillon VB, McCallum S, Norton P, Twomey BM, Erkeller-Yuksel F, Lydyard P et al.
Differential heat shock protein overexpression and its clinical relevance in systemic
lupus erythematosus. Ann Rheum Dis 1993; 52:436-442.
45. Millar DG, Garza KM, Odermatt B, Elford AR, Ono N, Li Z et al. Hsp 70 promotes
antigen-presenting cell function and converts T-cell tolerance to autoimmunity in vivo.
Nat Med 2003; 9:1469-1476.
46. Blachere NE, Li Z, Chandawarkar RY, Suto R, Jaikaria NS, Basu S et al. Heat shock
protein-peptide complexes reconstituted in vitro elicit peptide-specific cytotoxic T
lymphocyte response and tumor immunity. J Exp Med 1997;186: 1315). J Exp Med
1997; 186:1315-1322.
47. van der Weerd L, Lythgoe MF, Badin RA, Valentim LM, Akbar MT, de Belleroche JS
et al. Neuroprotective effects of HSP70 overexpression after cerebral ischaemia--an
MRI study. Exp Neurol 2005; 195:257-266.
48. Conroy SE, Tucker L, Latchman DS, Isenberg DA. Incidence of anti Hsp 90 and 70
antibodies in children with SLE, juvenile dermatomyositis and juvenile chronic arthritis.
Clin Exp Rheumatol 1996; 14:99-104.
49. Kim JJ, Lee SJ, Toh KY, Lee CU, Lee C, Paik IH. Identification of antibodies to heat
shock proteins 90 kDa and 70 kDa in patients with schizophrenia. Schizophr Res 2001;
52:127-165.
50. Chiba S, Yokota SI, Yonejura K, Tanaka S, Furuyama H, Kubota H et al.
Autoantibodies against HSP 70 family proteins were detected in the cerebrospinal fluid
from patients with multiple sclerosis. J Neurol Sci 2006; 241:39-43.
51. Sasajima T, Watanabe H, Sato S, Sato Y, Ohira H. Anti-triosephosphate isomerase
antibodies in cerebrospinal fluid are associated with neuropsychiatric lupus. J
Neuroimmunol 2006 (in press).
- 24 Table 1. Clinical and demographic characteristics of the NPSLE patients and the control
subjects
Patients and control subjects
No. Mean age SD (years)
Female/male
SLE patients
19
37.7 ± 14.4
17/2
NPSLE
7
43.6 ± 19.2
6/1
SLE without neurological manifestations
12
34 ± 9.7
11/1
82
42.3 ± 11.1
42/40
Relapsing-remitting
45
37.4 ± 12.1
28/17
Secondary progressive
15
52.7 ± 10.3
9/6
Primary progressive
22
47.5 ± 9.6
5/17
32
43.3 ± 7.4
23/9
SS with central nervous involvement
26
44.8 ± 7.4
19/7
SS without central nervous involvement
6
41.5 ± 7.9
4/2
27
32.8 ± 8.3
14/13
MS patients
SS patients
Healthy subjects
SLE = systemic lupus erythematosus; NPSLE = neuropsychiatric systemic lupus
erythematosus; MS = multiple sclerosis; SS = Sjögren’s syndrome
- 25 Table 2. Clinical and biological manifestations of neuropsychiatric systemic lupus
erythematosus patients at the time of blood sampling for the study
Age
Neurological
Renal
Anti DNA antibodies by Antiphospholipid
Immunosuppressive
(years) manifestations
involvement
Farr assay (IU)
antibodies
treatment
F
59
Cervical myelitis
No
8
Absent
Corticosteroids
F
18
Cerebral angiitis
Yes
9
Absent
Sex
Corticosteroids
Azathioprine
Corticosteroids
F
30
Cervical myelitis
No
20
Absent
Azathioprine
F
60
Seizure
Seizure,
F
45
No
8
Absent
Azathioprine
No
9
Present
Corticosteroids
optical
neuritis
M
26
Tetraparesis
Yes
22
Present
Corticosteroids
F
67
Stroke
No
50
Absent
None
- 26 Table 3. Number of antigenic bands recognized by serum IgG antibodies on normal and MS
CNS in patients with autoimmune diseases, in MS patients and in healthy subjects
Number of antigenic Number of antigenic
bands recognized on bands recognized on
Sera
normal CNS
MS CNS
mean ± SD (median)
mean ± SD (median)
12.2 ± 6.9 (12.0)
9.9 ± 5.5 (9.0)
20.8 ± 4.9 (21.0)**
16.0 ± 4.7 (16.0)**
21.0 ± 4.6 (21.0)***
16.7 ± 5.9 (16.0)***
Autoimmune diseases*
(n=51)
MS
(n=82)
Healthy subjects
(n=27)
*NPSLE, noNPSLE, SSCNS, SSnoCNS
** P < 0.001 between MS and autoimmune diseases
*** P < 0.001 between healthy subjects and autoimmune diseases
- 27 Table
4
- 28 Table
5.
- 29 Acknowledgement: This work was supported in part by grants from the Association Française
du Gougerot-Sjögren et des syndromes secs and from G4-Interrégion Nord-Ouest (France).
We also thank Dr Hervé Drobecq for the mass spectrometry analysis (Institut Biologie de
Lille). The authors are grateful to Nicholas Barton for his advice in editing the manuscript.
- 30 Figure Legends
Figure 1. Illustrative patterns obtained in NPSLE patients and in various controls. Two sera
from each of the groups (healthy subjects [1-2]; noNPSLE [3-4], NPSLE [5-6], SSnoCNS [78], SSCNS [9-10] patients; and MS patients [11-12]) were successively tested against healthy
(normal CNS) and MS (MS CNS) brain homogenates. A high degree of diversity was found
with the serum of a same patient tested against normal or MS CNS and among all groups of
tested subjects. However, some conserved sets of IgG reactivities were detected within a same
group, as indicated by black arrows, as well as between the different groups, as indicated by
gray arrows.
Figure 2. Identification of discriminant antigenic bands between patients with autoimmune
diseases with or without CNS involvement, MS patients and healthy subjects. A. Two
schematic illustrative western blotting strips depict the 16 brain antigens which support
discriminant immune reactivities on both healthy and MS brain homogenates with sera from
patients with autoimmune diseases (NPSLE, noNPSLE, SSCNS, SSnoCNS), from MS
patients and from healthy subjects. The coefficient values assigned by LDA (coefficient for X
and Y axis) were specified for each antigen. B. Graphic extrapolation of LDA obtained in the
3 groups of subjects tested. Coefficient values, associated with the presence or absence of
each discriminant antigen, led us to calculate graphic coordinates for each individual. The
graph clearly shows that the calculated scores of each subject are distributed in 3 distinct areas
corresponding to the 3 groups: patients with autoimmune diseases (NPSLE, noNPSLE,
SSCNS, SSnoCNS), MS patients and healthy subjects. A ROC curve delineated a threshold
value of 0.650 (data not shown) which differentiated MS patients from healthy subjects (y)
with a sensitivity of 95% and a specificity of 95.1%. A threshold value of 1.2 distinguished
- 31 patients with autoimmune diseases from patients with MS and healthy subjects (x) with a
sensitivity of 100% and a specificity of 100%. The results showed an excellent degree of
concordance with clinical data (=0.931). Antigenic bands were named by using their
molecular weight preceded by p if they were on normal CNS or P if they were on MS CNS.
Figure 3. Identification of discriminant antigenic bands between autoimmune diseases with or
without CNS involvement. A. Two schematic illustrative western blotting strips depict the 5
antigens that support discriminant immune reactivity on both healthy and MS brain
homogenates with sera from patients with autoimmune diseases according to the presence
(NPSLE, SSCNS) or absence of neurological manifestations (noNPSLE, SSnoCNS). The
coefficient values assigned by LDA (coefficient for X axis) were specified for each antigen.
B. Graphic extrapolation of data obtained in the 2 groups: coefficient values, associated with
the presence or absence of each discriminant reactivity, led us to calculate graphic coordinates
for each individual. The graph clearly shows that the calculated scores of each subject are
distributed in two areas corresponding to the two groups of patients, with an excellent degree
of concordance with clinical data (=0.960). Antigenic bands were named by using their
molecular weight preceded by p if they were on normal CNS or P if they were on MS CNS.
Figure 4. Respective frequencies of discriminant antigens obtained by comparing either
SSCNS and NPSLE (A) or noNPSLE and NPSLE (B). Common discriminant reactivities
obtained in A and B are indicated in bold and underlined characters. x: antigenic bands were
named by using their molecular weight preceded by p if they were on normal CNS or P if they
were on MS CNS. *P < 0.05 **P <0 .01
- 32 Figure 5. Characterization of discriminant antigens by serologic proteomic approach. The 2D
immunoblottings were treated with sera of NPSLE patients (representative data are shown in
A with the serum of NPSLE patient n°3) or SSNCS (representative data is shown in B with
one serum). Antigenic spots, matched with CBB-stained gel (in C), are marked with SwissProt or TrEMBL accession numbers (see Table 5).