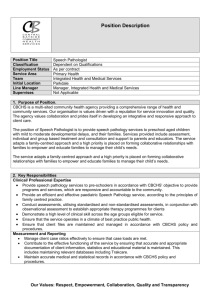
Family-centred, person-centred practice
advertisement

Working with children, adolescents and young adults with a disability and their families Family-centred, person-centred practice A guide for everyday practice and organisational change Published by Disability Services Division Victorian Government Department of Human Services 50 Lonsdale Street Melbourne Victoria Australia June 2012 © Copyright State of Victoria, Department of Human Services and Department of Education and Early Childhood Development, 2012. This publication is copyright. No part may be reproduced by any process except in accordance with the provisions of the Copyright Act 1968. ISBN 978-0-7311-6522-3 (online version) Authorised and published by the Victorian Government 50 Lonsdale Street, Melbourne (0210212) If you would like to receive this publication in another format, please phone 1300 336 731, using the National Relay Service 13 36 77 if required. This document is available as a word file and a PDF file on the Internet at www.dhs.vic.gov.au Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 2 Acknowledgements The Department of Human Services and the Department of Education and Early Childhood Development wish to acknowledge the contribution of colleagues from around Victoria who provided information and feedback during the development of the family-centred practice guides suite. This project aimed to be family centred in its approach; grateful thanks to all the families and people with a disability who shared their stories and ideas for the project with generosity, courage and candour. The project team were: from Red Tree Consulting, consultants, researchers and writers Sarah Marlowe, Elizabeth Wheeler and Cara Brough; from the Association for Children with a Disability, project manager and Chief Executive Officer Elizabeth McGarry, project worker Janice Chan and other ACD staff and members; and researchers and critical readers Carmel Laragy from the RMIT School of Global Studies and her colleagues Mary Collins and Enza Santangelo. Suggested citation: Department of Human Services and Department of Education and Early Childhood Development 2011, Family-centred, person-centred: a guide for everyday practice and organisational change, State Government of Victoria, Melbourne. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 3 Contents Families and young people quoted ............................................................................................. 7 1 Introduction ............................................................................................................................. 9 About this guide .......................................................................................................................................... 9 The suite of resources ................................................................................................................................. 9 An evolving approach ................................................................................................................................ 10 Isn’t it just good practice?.......................................................................................................................... 10 Policy context ............................................................................................................................................ 10 2 Foundations .......................................................................................................................... 13 Defining family-centred practice ................................................................................................................ 13 Underpinning beliefs and values ............................................................................................................... 13 Findings from the literature ....................................................................................................................... 14 Who is ‘family’? ......................................................................................................................................... 16 Family and person centred........................................................................................................................ 17 Working with children and adolescents ............................................................................................... 17 Working with young adults .................................................................................................................. 18 Family-centred, culturally responsive services ......................................................................................... 19 Working with Aboriginal families and communities ................................................................................... 20 Learning to support cultural respect, responsiveness and safety ....................................................... 21 Working with culturally and linguistically diverse families ......................................................................... 22 Learning to support cultural responsiveness ....................................................................................... 22 3 Family-centred practice model ............................................................................................. 25 A model for everyday practice................................................................................................................... 25 Element 1: Practices that build relationships ............................................................................................ 25 Element 2: Practices that support choice and participation ...................................................................... 26 Element 3: Technical quality ..................................................................................................................... 26 4 Practices that build relationships: values, attitudes and beliefs ....................................... 27 Looking within ........................................................................................................................................... 27 The importance of values .......................................................................................................................... 28 Discrimination, safety and trust ................................................................................................................. 29 Sharing power ........................................................................................................................................... 30 5 Practices that build relationships: interpersonal behaviours and skills .......................... 32 Communication ......................................................................................................................................... 32 Listening .............................................................................................................................................. 32 Non-verbal communication .................................................................................................................. 33 Communicating directly and respectfully with children and young people .......................................... 34 Communicating across language, educational and other barriers ...................................................... 34 Gathering information................................................................................................................................ 35 Supporting informed choice ...................................................................................................................... 36 Offering information ............................................................................................................................. 36 Meeting people’s learning needs and supporting online research ...................................................... 37 Connecting families with other families ............................................................................................... 37 Emotional responsiveness ........................................................................................................................ 38 Affirming the importance of family ....................................................................................................... 39 Communicating about medical and developmental issues ................................................................. 40 Building trust ........................................................................................................................................ 40 When resources don’t meet people’s needs ............................................................................................. 40 Ongoing communication ........................................................................................................................... 41 Information about service levels and provision ................................................................................... 41 Keeping families in the picture ............................................................................................................ 42 Respecting young people’s privacy ..................................................................................................... 42 6 Practices that support choice and participation: decision making and action ................ 44 Self-determination, inclusion and choice .................................................................................................. 44 Supporting choice ..................................................................................................................................... 45 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 4 Ask and offer ............................................................................................................................................. 45 Collaborative goal setting .......................................................................................................................... 46 Choice in the context of limited resources ................................................................................................ 47 Children and young people’s role in decision making ............................................................................... 47 Supporting children and young people’s input .................................................................................... 48 When family-centred and person-centred practices come into tension .............................................. 48 Supporting action ...................................................................................................................................... 50 Tailoring support for action .................................................................................................................. 51 ‘Releasing’ people’s capacity to take action ........................................................................................ 52 When families are dissatisfied with the service’s approach ................................................................ 53 If you are concerned about people’s choices............................................................................................ 53 7 Practices that support choice and participation: flexible, responsive services and supports ................................................................................................................................ 56 Fitting in with family life ............................................................................................................................. 56 Family schedules and routines ............................................................................................................ 56 Childcare needs................................................................................................................................... 57 Transport ............................................................................................................................................. 57 Service hours....................................................................................................................................... 58 Communication preferences ............................................................................................................... 58 Service levels ...................................................................................................................................... 58 Reducing the demands on families ........................................................................................................... 58 Offering support with administration .................................................................................................... 59 Maximising continuity of care .............................................................................................................. 59 Sharing information ............................................................................................................................. 59 Following up and paying attention to detail ......................................................................................... 59 Improving service integration .............................................................................................................. 59 Tailoring services and supports ................................................................................................................ 59 Taking a lead from families ................................................................................................................. 60 Common areas of difference ............................................................................................................... 60 Identifying appropriate locations and services, supporting inclusion .................................................. 62 Supporting parents and caregivers ..................................................................................................... 63 Supporting siblings .............................................................................................................................. 64 Linking people into community ............................................................................................................ 65 Tailoring supports to people’s capacity ............................................................................................... 67 Responding to change .............................................................................................................................. 67 8 Technical quality ................................................................................................................... 69 Family-centred practices as core professional skills ................................................................................. 69 Using family-centred tools and methodologies ......................................................................................... 70 Working towards service integration ......................................................................................................... 71 Referring and using secondary consultation ............................................................................................. 72 Self-care and maintaining appropriate boundaries ................................................................................... 72 9 Family-centred organisations .............................................................................................. 75 The barriers to change .............................................................................................................................. 76 A framework for action .............................................................................................................................. 76 Supporting staff to be family centred ........................................................................................................ 77 Professional development and orientation .......................................................................................... 77 Supervision .......................................................................................................................................... 77 Reflective practice, team-based approaches and using written materials .......................................... 78 Service development ........................................................................................................................... 78 Management practices ........................................................................................................................ 79 Systems, policies and procedures....................................................................................................... 79 Family participation in organisations ......................................................................................................... 80 A family-centred service system ............................................................................................................... 80 Creating more family-centred professions ................................................................................................ 81 Family-centred organisations as learning organisations ........................................................................... 81 10 Maintaining and improving practice .................................................................................... 82 Monitoring and seeking feedback ............................................................................................................. 83 Reflective practice ..................................................................................................................................... 83 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 5 Using this suite of guides .......................................................................................................................... 84 Next steps ................................................................................................................................................. 84 Endnotes ..................................................................................................................................... 86 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 6 Families and young people quoted Thank you to the families and young people with a disability who generously shared their stories and ideas for these guides. Here we list those people to acknowledge them, and to convey a sense of the diversity of those who took part. Names and identifying details have been changed to protect anonymity. Alison, mother of Mark (who has a genetic syndrome resulting in a mild physical and intellectual disability) Amina, a parent from a support group for families from a Middle Eastern community Amy and Colin, parents of Emily (who has complex medical needs), her older brother, Anthony, and her younger sister, Lisa Anita and Peter, parents of Michael (who has Down syndrome), his younger brother, Ryan, and his sister, Claire Anthea, an advocate and a young person with a disability Betty, a parent from a support group for families from a North Asian community Caitlin, a young person with a disability Cass, mother of Abel (who has autism spectrum disorder and epilepsy and is visually impaired), his younger sister, Julie, and younger brother, Jack (who has a learning delay) Cathy and Richard, parents of Cameron (who has Asperger’s syndrome), Angela (who has an intellectual disability and issues with mobility, hearing and sight) and Natasha Daniela and Joe, parents of Ben (who has autism spectrum disorder) and his younger sister, Allegra Deborah and Saul, parents of Ruth (who has Down syndrome), and her siblings, Aaron, Leah and Nate Donna, mother of Casey (who had an intellectual disability and complex medical needs and passed away aged 10) and her older brother, Ben Fatima, a parent from a support group for families from a Middle Eastern community Ingrid and Dan, parents of Ella (who has Down syndrome), her older brother, Justin, younger sister, Rose, and younger brother, Luka Jan and Sean, parents of Louise (who has a mild intellectual disability) and her younger brother, Lachlan Julia, a parent from a support group for families from a North Asian community Kate and Greg, parents of Jamie (who has a pervasive developmental disorder) and his younger siblings, Melanie and Callum (who both have Asperger’s syndrome) Lilly, a parent from a support group for families from a South-East Asian community May, a parent from a support group for families from a North Asian community Melissa and Roland, parents of Michelle (who has Down syndrome) and her younger brothers, Stefan and Tad Miriam, a parent from a support group for families from a Middle Eastern community Natasha, a parent from a support group for families from a Middle Eastern community Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 7 Paula and David, parents of Samuel (who has an intellectual and physical disability) and several other children Sue, mother of Nicky (who had atypical Rett syndrome and passed away aged 19); Sue is also the principal of a special school Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 8 1 Introduction About this guide This guide aims to support people who work with children, adolescents and young adults with a disability or developmental delay to work in more family-centred ways. It is for educators, respite workers, allied health practitioners, early childhood intervention professionals, case managers and the myriad other professionals involved in the lives of children and young people and their families. Family-centred approaches will already inform the work of many readers in different ways. This guide seeks to strike a balance between orienting less experienced professionals to the approach and supporting their more experienced colleagues to reflect on and improve this aspect of their work. A fundamental premise of the guide is that there is always more that any professional can do to strengthen and deepen their family-centred practice. This is backed up by research demonstrating that a gap can arise between how family-centred professionals think their practice is and the experience of those they work with;1,2 and that even professionals dedicated to family-centred practices can find them difficult to sustain fully over time.3 Leading family-centred practice researcher Carl Dunst, drawing on feedback from service users over many years, suggests that many professionals excel in what he calls the ‘relational’ elements of family-centred practice but find it challenging to maintain its ‘participatory’ elements – those that support family choice and participation, and potentially impact on the nature of services themselves.4 In consultations for this guide, many families, young people and professionals described examples of excellent practice. Many also described instances when families or young people felt let down, frustrated or not respected, heard or understood. These stories highlight the need for professionals, organisations and the system as a whole to be more family centred. Most children, young people and families are involved with a constellation of services. Improved communication, coordination and integration between them make it more likely that a family’s needs, preferences and priorities will shape the supports they receive. This guide draws on the literature, the practice wisdom of many skilled Victorian professionals, and the views and experiences of diverse families and young people with a disability. The stories and voices of families and young people with a disability and practice examples from professionals feature extensively throughout, providing evidence, inspiration and many concrete ideas for good practice. The guide begins with a discussion of some foundational concepts related to family-centred practice, including what the literature says and what the approach offers to working with adolescents and adults with a disability. An outline then follows of the practice model on which the guide is based. The following five chapters explore various aspects of the model and their implications for practice. The guide ends with discussion about how organisations can be more family centred, and how reflective practice and regular feedback from service users can contribute to maintaining and improving practice. The suite of resources This is the foundation document in a suite of seven family-centred practice guides. It provides the context, conceptual framework and evidence for the approach, explores issues relevant to translating theory into everyday practice and organisational change, and offers many practical suggestions. Five of the shorter guides provide more tips and ideas for practice in specific settings: Family-centred, child-focused support in the early childhood years: a guide for early childhood intervention service professionals Family-centred, person-centred planning: a guide for professionals in intake, planning and case management roles All subsequent references will be to ‘people with a disability’ only for ease of reading. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 9 Family-centred, person-centred allied health: a guide for practitioners in private practice, schools and clinical settings Family-centred, person-centred support: a guide for disability support workers Working with students with a disability and their families: a guide for school staff with student support roles. The sixth shorter guide is Family-centred, person-centred organisations: a guide for managers and governance bodies to support whole-of-organisation approaches to family-centred practice. It provides support for management and boards to implement whole-of-organisation approaches to strengthening familycentred practice. An evolving approach The origins of family-centred practice as a term are in early childhood intervention (ECI). But family-centred practice as a philosophy arose from the consumer movement, which also drove the development of personcentred practice. As this ECI service manager acknowledged: We like to claim family-centred practice now, with the literature and the research. What we have to remember is that it was consumer driven. It was parents refusing to put their children in institutions … that made the change. Although family-centred practice has informed work in some sectors for years, it remains a work in progress, both as a field of research and a way of working with children, young people and families. Good practice and better understanding of the more complex and challenging aspects of family-centred practice will continue to grow as individuals and organisations in every sector reflect on and adjust their ways of working, seek feedback from service users, change and reflect again. Australian families and the demographics of service catchments are also changing, as is understanding of the disabilities that affect children, adolescents and adults. Responsiveness is vital to family-centred practice, and all of these shifts contribute to the ongoing evolution of family-centred practice in theory and application. Isn’t it just good practice? Family-centred practice is a crucial component of high-quality services and supports because it enables professionals in this field to do their jobs more effectively. Some elements of family-centred practice are the fundamentals of good human services practice, including skilled communication and offering supports that meet people’s needs. Others – especially those related to decision making – take it beyond those fundamentals. Family-centred practice requires a shift in power and authority away from the professional as ‘expert’ and key decision-maker (as in ‘medical model’ approaches) and towards the person with a disability and their family. In fact, additional expertise is required to empower people with a disability and their families. Some professionals wonder what this shift in power and authority means for their skills, knowledge and experience. Family-centred practice does not undermine these assets but helps professionals use them more effectively, in partnership with the people they work with. Evidence shows that this can help services make a greater, more lasting difference to the lives of children and young people and their families. Policy context The policy context for family-centred practice differs somewhat between sectors but, broadly, change is towards greater emphasis on: evidence-based and reflective practice; inclusion and participation; choice, self-determination and self-directed support; service integration; and partnership with families. In general, thinking around family-centred practice is most developed within ECI, where it has informed a reorientation of services in the past decade towards community-based supports and greater partnership with parents and caregivers. This is reflected in the Early childhood intervention practitioner competencies5 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 10 developed for the Victorian Government by the Early Childhood Intervention Association (Victorian chapter). These competencies inform this and the ECI guide. The Victorian early years learning and development framework (VELDF)6 and its associated practice principles also inform the guides and provide a context for early years educators and ECI professionals. Services for children and young people with a disability over the age of six (that is, post-ECI) have also undergone a significant paradigm shift, with moves towards self-directed support and individualised funding. The National disability strategy highlights growing Australian and international support for ‘person-centred and self-directed’ supports7 that maximise choice.8 Choice is a key Victorian Government principle underpinning these guides (see box) and is supported by both family-centred and person-centred practice. Person-centred practice is a critical element of disability services, yet the reality is that many adults with a disability live with or rely on continuing support from family (although who those people are might change). As children grow to adolescence and adulthood, professionals working with them need to draw on both family-centred and person-centred approaches. Legislative and policy frameworks also support the related principle of inclusion.9 This recognises that the choices available to people with a disability and their families will always be limited unless government, service providers and the community work together to address barriers that prevent their full inclusion and participation in every aspect of community life. For educators and allied health practitioners working in schools with older children and young adults, a number of policy documents, standards and resources (listed in the relevant guides) provide support and context for family-centred approaches. In general, family-centred practice in these settings reflects a shift within schools’ perception of students from being passive recipients to active participants in their education. It also reflects the widening of the family’s role from ensuring their child gets through the school gate to active partnership in the child’s learning and development. These guides are also informed by the principles of the Victorian Government’s Cultural and linguistic diversity strategy relating to equality, dignity and self-determination, valuing diversity and non-discrimination, as well as those in Enabling choice for Aboriginal people living with disability, relating to improving access, promoting least intrusive early intervention, supporting participation, and building cultural competence through partnership with Aboriginal organisations and communities. Family-centred practice has the potential to unite key aspects of all these policy directions and philosophical strands in a coherent model of practice and an adaptable set of values, skills, behaviours and knowledge that can strengthen the work of professionals in each sector addressed in these guides. Pull out Box - Principles Children and young people with a disability or developmental delay and their families are best placed to know what mix of services and supports are likely to meet their needs. Services should be based on the priorities of children and young people and their families, responding to the particular stage of the child or young person’s development. A child- and family-centred approach based on a partnership between parents and professionals should maximise the choices and opportunities available to children and young people with a disability or developmental delay and their families. Services provided to children, adolescents and young adults with a disability or developmental delay and their families should be guided by the following principles: The best interests of children and young people are paramount. Services and supports protect and promote human rights, including the rights of the child and young person with a disability or developmental delay. Services and supports adopt a child- and family-centred approach that promotes choice and opportunity. Services and supports are accessible and coordinated to intervene early and adopt a life-cycle approach to the planning and provision of services. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 11 Services and supports are integrated to meet the holistic needs of children and young people with a disability or developmental delay and their families. Services and supports promote social inclusion. Services and supports are accessible and appropriate for children and young people from diverse cultures and their families. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 12 2 Foundations Key messages Family-centred practice is underpinned by key values about children, young people and families, including that children and young people are agents in their own life, and that families have significant expertise in relation to their children’s lives, and have the right to seek the best possible services and supports for them. Family-centred practices have been widely adopted in Australia and elsewhere in the past decade. There is now strong evidence for the approach, including that it improves child behaviour and wellbeing, family functioning, levels of social support available to families and family satisfaction with services, and that it contributes to these primarily by increasing parental self-efficacy. The approach is also supported in school settings by evidence of the benefits of family–school partnerships for all students. Professionals need to combine family-centred and person-centred approaches, especially in work with young people. This means respecting their choices and supporting the relationships that are important to their longterm wellbeing. It also includes responding to family members’ concerns and knowledge about their child and offering information that might add to their understanding of their child’s needs or options in the future. Culturally responsive practice is deeply linked with family-centred practice because culture profoundly shapes human development and family structures. It asks that professionals address discrimination and ensure that culture informs all aspects of service provision. Family-centred practice can help services improve their relevance to diverse communities in the catchment because family is central to the lives of people in Aboriginal and many culturally and linguistically diverse (CALD) communities. The basic approaches to culturally responsive practice with Aboriginal and CALD families are similar, but the practices and key issues are very different. Defining family-centred practice Family-centred practice is a set of values, skills, behaviours and knowledge that recognises the centrality of families in the lives of children and young people. It is grounded in respect for the uniqueness of every person and family, and a commitment to partnering with families and communities to support children and young people with a delay or disability to learn, grow and thrive. It puts family life – and the strengths, needs and choices of people with a disability and their families – at the centre of service planning, development, implementation and evaluation. Family-centred practice is not an end it itself, rather it enables professionals to do what they do more effectively. It is no less important because of that. Evidence shows that the way supports are provided has an impact on families, as well as the supports themselves.10 The centrality of ‘family life’ is crucial. It goes beyond the child or young person and their family. It is them and everything that makes up their world: their relationships, resources and daily lives; their culture, community and language; their stresses, needs and tensions; their preferences, interests and priorities; and their goals, hopes and aspirations. Underpinning beliefs and values The skills and behaviours that family-centred practice requires are underpinned by certain beliefs and values, including that children, adolescents and young adults with a disability: are agents in their own life, and have their own strengths and assets do best growing up in family settings, in safety, and with stable relationships, consistent support and opportunities for continuing connections with their parents, broader family and culture into adulthood Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 13 are entitled to the support and opportunities they need to achieve their full potential; to create connections, make contributions and feel a sense of belonging to their family, community and culture; and to participate in the social, economic, cultural, political and spiritual life of society have the right, as adults, to make and act on their own choices, or to contribute to decision making according to their capacity, and are entitled, as they grow towards adulthood, to support that helps them develop the skills and confidence to do so. Family-centred practice is also grounded in the belief that: human development is best understood as an interaction between the person as an active individual and their environment – that is, all the interactions and relationships that make up their world, 11 which for children and young people primarily means their family every family is unique, with its own strengths and assets, and is made up of those people who consider themselves family, whether or not they live together or are related by blood or marriage families have significant expertise in relation to their children’s lives; are central to providing an environment in which their children grow, learn and thrive; and are best placed to advocate for and support them families care deeply about their children’s development and wellbeing, and with the right support, most who are struggling can successfully adapt to the changes that their child’s developmental delay, disability or medical issue brings to their lives, and provide a safe, caring and stimulating environment families have the right to seek the best possible services and supports for their child, and to not be judged for doing so. Pull out Box - Personal perspective: Alison and Mark When Alison’s son, Mark, was diagnosed with a rare genetic condition (resulting in intellectual and physical disability), his doctor gave the family the ‘textbook’ prognosis. ‘It was the very worst example of what can happen,’ Alison says. ‘He said Mark would never be independent, never be able to do things for himself.’ This contradicted Alison’s own understanding of her son’s potential. ‘I looked at my gorgeous, smiling boy and thought, Who is right here? I had to make some decisions about how to deal with this.’ Part of that meant coming to terms with Mark’s disability. ‘I felt I’d lost my child,’ Alison says. ‘I had to re-learn who he was.’ Finding a paediatrician who focused on working with the family made a huge difference: ‘He listened. He responded appropriately. He followed up. He was gorgeous with Mark, and celebrated his milestones.’ Throughout their journey Alison has particularly valued professionals who recognised when she needed them to ‘step up, but not take over’. One was Mark’s occupational therapist (OT) at school – a great communicator, who also became Mark’s advocate: ‘She would see him every week, and see what was happening. I didn’t, because I was at work.’ Together the OT and Alison encouraged Mark’s school to meet his needs, and when it didn’t happen, the OT helped Alison explore other options. Mark recently returned from an overseas trip, moved into supported accommodation and got a part-time job, which he loves. He’s ‘excited about life,’ Alison says. ‘This is what I want for both my children – to want to live their life to the fullest.’ Findings from the literature Evidence for the efficacy of various elements of family-centred practice is cited throughout the guides. Below is a summary of what key investigations into the approach have revealed. Family-centred approaches have been widely adopted in work with young children with a disability and their families in the past decade in Australia, New Zealand, Canada, the United States and United Kingdom.12,13 Family-centred practices are also informing work with older children and young people, especially in allied health and other health service provision, 14 planning and disability support.15 Both family-centred practice Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 14 and inclusion are key practices within Victorian early childhood education settings, 16 while family–school partnership is increasingly informing approaches within Australian schools. 17 In recent years even stronger evidence has begun to emerge about the efficacy and effects of family-centred practice in various settings. A 2005 Australian literature review found that family-centred practice produces ‘positive parent and family benefits beyond those produced by structural intervention factors (such as the form and frequency of services provided) and non-intervention factors (such as employment, housing and health care)’.18 In 2007 a synthesis of 47 studies investigating the effects of family-centred practices reported: increased family satisfaction with the helpfulness of services increased parental self-efficacy (see page 50) increased levels of social support improved child behaviour and wellbeing improved family functioning.19 In 2008 another Australian literature review concluded that theoretical evidence for the approach is strong but that ‘the relationship between the provision of family-centred services and the achievement of positive outcomes for children and their parents is complex and is yet to be fully understood’. 20 Significant progress was made towards this in 2010, with a further synthesis of 52 studies concluding that: family-centred approaches had both direct and indirect effects on parent, family and child behaviour and functioning; indirect effects were the strongest; and these occurred through strengthened parental self-efficacy. That is, parental wellbeing and belief in their abilities (such as to problem-solve and get the resources their family needs) influenced parent–child interactions, which in turn had a positive effect on child development.21 A 2010 review of the evidence for family-centred practice in early childhood education settings concluded that family-centred practice: promotes parental involvement in education, which is associated with improved learning outcomes promotes continuity of care and more secure attachments for children enables professionals to develop responsive learning programs that build on children’s prior learning experiences.22 Research in educational settings beyond the early years also supports greater partnership between schools and families, suggesting these are achieved when: early childhood services and schools engage with all families families have a say in and can directly contribute to programs, such as extracurricular activities there is a shared understanding of the importance of academic and personal development between families, early childhood services and schools. 23 Further research demonstrates significant impacts for students of all ages, including: better learning and development outcomes in the early years and at school increased engagement in learning and development smoother transition to and from school higher retention rates increased confidence, social skills, emotional resilience, communication skills, classroom behaviour and general wellbeing reduction in the effects of disadvantage among children from low socioeconomic backgrounds. 24 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 15 Who is ‘family’? Family-centred practice requires that services recognise the diversity of Australian families, and who family is to the child, adolescent or young adult with a disability. For young children, family is whoever the adults closest to them (usually, but not always, their parents at birth) say it is. In adolescence, this can become more fluid, and by early adulthood, ‘family’ includes anyone a young person identifies as such, including perhaps a partner, trusted caregiver or close friend. Often who we expect family to be is not the reality. There are people who become terribly important to the ‘management’ of disability that you wouldn’t expect – a neighbour, or whoever. Within an hour of my daughter dying at age 19, her taxi driver was at my door, distraught. He’d known her for 12 months, the whole of her post-school time. He picked her up every morning and delivered her home in the evening. Anybody else who wanted a booking at that time could go jump. Periodically the two of them would turn up late, and he’d announce that they’d been for a chocolate or a milkshake! He’d already told us he’d be wearing a suit at her 21st birthday. He self-nominated to be someone in my daughter’s life – but without him and his flexibility, our family would have been in trouble. – Sue, mother of Nicky and principal of a special education school Definitions of family are deeply cultural. In many CALD families, grandparents or other relatives often provide primary care, while Aboriginal definitions of family can encompass a broad community of care beyond biological relationships, and can include a special role for grandparents and Elders, all of which has implications for whom the professional will work with: I can go into a home and teach a boy to sign. One week I’ll have his mother and his siblings learning too, but then the next week I’ll have his grandmother and his aunts and uncles, and then another week I’ll have a new set of cousins. I have to start at the beginning each time. You need to be flexible to engage the whole family. – Jody Saxton-Barney, Victorian Aboriginal Disability Network These guides use ‘family’ to include siblings and all consistent non-professional caregivers in a child or young person’s life (including foster carers) – in fact, those people who regard themselves as family, regardless of whether they are biologically related or living with the child or young person. Family-centred practice also requires that professionals understand the complex, reciprocal relationships between all members of a family. It comes down to communication. Families need to communicate the needs of each individual, their joys as a whole family, and the involvement that each person has. Services need to work with the family as a whole to be effective. – Cass (see family listing on page 7) To me, my relationship with my sister is completely normal. Have I missed out on things in life? Probably, but I have gained much more than I have lost … I think by matter of circumstances that [siblings of people with a disability] grow up a little bit quicker. We see what life is truly about, and we witness and are part of the unfairness of the world … Our early insight into what life is all about gives us a good understanding of who we are. It is early maturation. It is unchosen responsibility. It is compassion and it is caring. And it is something people do not expect of children, teenagers and even young adults. But wrong it is not. It is love.25 – Adult who grew up with a sister with a disability In practice, working with the family usually means engaging mothers, who are most often the primary caregiver by choice or circumstance.26 Yet support for the whole family is critical. Families deeply appreciate services that work to engage with other family members: They had a playgroup on Saturdays so dads could come with the children – siblings as well … my younger kids still attend and love the siblings group. It’s a great time to chill out with other kids who understand what they go through. There’s also a lot of family nights – you might have dinner there, and some sort of entertainment, like a puppet show. It’s amazing how much the kids love going. My kids have been asking me all term about it. So they get support, and I get support. – Melissa (see family listing on page 7) Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 16 Family and person centred Professionals need to combine family-centred and person-centred approaches, especially with older children, adolescents and young adults. Person-centred and self-directed approaches increasingly inform disability service provision within Australia and internationally. 27 The National disability strategy recognises that ‘[p]eople with disability have lived experience of disability and must play a central role in shaping and implementing policies, programs and services that affect them’, and provides direction for ‘[a] sustainable disability support system which is person centred and self directed, maximising opportunities for independence and participation in the economic, social and cultural life of the community’. 28 Working with children and adolescents As mentioned, the term ‘family-centred practice’ originated in ECI, which works with children from birth to six years. In that context, it is largely about responding to a family’s wishes, except where they conflict with a child’s best interests. The child is the reason for a service’s involvement, however, and remains at the centre of the professional’s relationship with the family. Therefore the intersection of family- and person-centred approaches in an ECI context is best characterised as ‘family centred, child focused’. Yet almost all children, as they mature, want an increasing say in decisions that affect them, a right recognised by the United Nations Convention on the Rights of the Child.29 Professionals can support even young children’s input into decisions by recognising and responding to indications of their preferences. Children and young people who are non-verbal communicate these in many ways, including through sound, posture, expression, gaze and the use of communication aides. Many parents and caregivers work hard to support their children’s growing independence, to maximise their decision-making capacity and to ensure their preferences, goals and ambitions inform services and supports. Anita (see page 68) has used her son Michael’s supports in different ways as he has matured, to give him choices, foster his independence and support him to achieve his goals. Anthea’s mother, after years of nurturing her daughter’s skills and confidence, ‘works in tandem’ with Anthea (now 19) to support her to direct her own services. Paula (see page 188) says of her now 22-year-old son: Samuel is totally reliant on other people, so we’ve done our best to support him to be as self-assertive as possible. He does have speech, and he loves to tell people about what his rights are. If someone says, ‘No,’ he’ll tell them, ‘It is my right to do – ’ whatever it might be. We’re very proud of him. Other families might be less keen to prioritise their child’s input into decision making, perhaps due to their family or cultural values, because they are not optimistic about their child gaining the necessary skills, or if their views differ significantly from their child’s. In a world where adults often make the decisions, it can be difficult for any child or young person to have their choices heard and respected consistently. It can be even harder for those with a disability: Generally the people who are in power are people without disabilities … Often it’s too easy for the person with a disability not to be listened to. Usually it’s the parents who complain. The young person is the least likely to be vocal but the most likely to be affected by the decisions that are made. So you need to make a lot of effort to not ignore the person who has got the most at stake. – George Taleporos, Youth Disability Advocacy Service Coordinator Professionals need to respect and respond to family members’ views, concerns and knowledge of their child. Yet sometimes it will also be appropriate to offer information that might add to the family’s understanding of their child’s needs or options, especially as the child grows towards adulthood, including perhaps addressing the family’s fears about their child’s future. It can often be valuable to offer families an opportunity to learn from others facing the same challenges. Both person-centred and family-centred approaches can deepen everyone’s knowledge of the person with a disability, and lead planning and other work in unexpected and fruitful directions. As one mother said: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 17 I thought I knew my son so well until we started planning with John. This changed our whole way of thinking about what John was capable of doing now and in his future.30 Pull out Box - Personal perspective: Paula, David, Samuel and family Paula and David have an adult son, Samuel (who has a physical and intellectual disability), and several other children. ‘Samuel had a really dedicated team of therapists in both primary and secondary school,’ Paula says. ‘They knew it would be really important to train his new team of support workers so that he would be assisted properly and, at the same time, encouraged to do what he could for himself.’ The family also appreciated the flexibility of Samuel’s therapists. ‘They wouldn’t say, “Your next appointment will be …” and look in their diary. They would say, “What are you doing? When and where can we see you that best suits you?” When the kids were little we’d have to be in four places at once. So they’d fit in therapy with us. Or they’d use their knowledge and resources to find equipment for us to trial – which is really time consuming – and sometimes they’d even deliver it to our doorstep.’ As Samuel matured, Paula expected professionals to consult directly with him. ‘Not the high-level negotiating,’ she says, ‘but what he wants to do, or who he wants to mix with. I modelled what I would expect … We’ve always encouraged him to ask questions. It blows me away how he makes people accountable. If they have a conversation that doesn’t include him, he’ll say, “What’s an ISP?” or “When are we going to do that?”.’ Paula and David continue to advocate both for and with Samuel, supporting him to develop an ‘increasing capacity to challenge systems and people himself’. Working with young adults Unless under guardianship order, from the age of 18 young people are entitled to make their own decisions. All young people need support to develop the skills and confidence to make good choices, or to contribute to decision making according to their capacity. For those with a disability, this should include the freedom to learn by trial and error, like any other young person. In this context, it’s important that professionals respect young people’s privacy and confidentiality, except if a duty of care issue arises. Many young people (especially if their disability is primarily physical) can become completely independent in advocating for themselves. Others will always require some assistance to identify their needs and perhaps make some types of decisions. Over time, this might come from their family of origin, from others who become family to them, from advocates or from other services. Sometimes young people make choices that clash with the preferences of family members. It can be difficult to determine what family-centred practice means in this context. The reality is that a lot of young people with a disability rely on their family of origin into adulthood. For many, these are their most lasting and supportive relationships. As Caitlin says (see box below), service providers should strive for ‘a balance’: being mindful of everyone’s needs, the age of the person, and how each decision impacts on everyone involved. When such issues arise, they often relate to autonomy, independence, identity, risk taking and sexuality. Issues to do with sexuality might include a young person wanting to have sex, enter a relationship, move in with a partner or explore their sexuality, including whether they are (like 8.6 per cent of men and 15.1 per cent of women in Australia31) same-sex attracted. Professionals need to respect young adults’ choices and support the relationships that are vital to their longterm wellbeing. The latter includes ensuring good communication with family, coordinating with the young person’s ‘natural supports’ (in their family of origin and beyond) and understanding the role of family and community in the young person’s life. Family and community can be especially important to the identity of young people whose culture puts strong emphasis on relationship and family. Those working with young adults with a disability need to hear and value family members’ concerns and knowledge of their child. It is often important, too, that they find ways respectfully to extend family members’ sense of what might be possible (and even necessary) for their child in the future. This might include, for example, information about services available to support independent living, 32 or assistance with transitioning from school-based to adult disability services. Creative, inclusive planning approaches, incorporating networks of support beyond immediate family, can help. 33 Professionals also need to validate the ongoing role of family members, and acknowledge that it isn’t always easy to ‘step away’: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 18 It helps if the parents are confident that their young person is having good outcomes, and that the service system is responding to their needs. [But if] a service is failing them, they’re not going to let go of control. It’s their instinct to make sure that their child is supported. The system isn’t very good at letting parents step away because there’s so much dependence on unpaid, informal support … [and] when they’re providing a lot of the care needs, it doesn’t feel very natural to switch off. – George Taleporos, Youth Disability Advocacy Service Person-centred and family-centred approaches can look very different in practice, but philosophically they are both grounded in the right to self-determination and appropriate support. What happens if they come into tension depends on many factors, including the young person’s age and capacity, the decision in question and its impacts on everyone involved, and the professional’s role and relationship with all parties. Pull out Box - Personal perspective: Caitlin Caitlin (a young woman with a disability) is ‘in two minds’ about family-centred approaches. ‘On the one hand I can see it’s very important, that having one person with a disability can impact on the whole family. But I know from personal experience that it can be detrimental, when my parents’ opinions were given more weight than mine.’ An example for Caitlin is when her school and family pressured her to do Year 12 over two years. She thought she could do it in one, and felt strongly about graduating with her friends. She stood her ground, with support from the school counsellor, and did Year 12 the way she wanted. ‘You hope that as you mature, [professionals] will listen to what you want more,’ Caitlin says. ‘I guess it’s about establishing a balance, and being mindful of the needs of each person within the family. But also considering how much the decision impacts on each person. The Year 12 decision impacted more on me than on my parents. After all, it’s my life.’ ‘It’s also about the person’s age. I was 17 – more than old enough to start making my own decisions. Maybe if I had been younger it would have been more appropriate to listen to my parents. Although I also think children always have an opinion about how things should be. It’s just that when you’re younger, you don’t take all factors into consideration.’ A complicating factor for Caitlin was that her mother also had a mental illness, which Caitlin was unwilling to disclose because she already felt ‘a bit stigmatised’ at school because of her disability. Her mother’s mental health services should themselves have been more family centred, Caitlin says. ‘No one followed up with her kids and [asked] where were we. It was up to me to find my own support services. I was lucky the school counsellor was quite supportive.’ Family-centred, culturally responsive services The Victorian community is very diverse. Victorians come from more than 200 nations and 120 faiths, speak more than 200 languages and dialects, and include more than 30,000 Aboriginal people representing more than 30 distinct communities. Almost a quarter of Victorians were born overseas, 74 per cent from nonEnglish-speaking countries; one in five speak a language other than English at home.34 Culturally responsive practice is when professionals and organisations have the capacity to respond respectfully and skilfully to the needs of diverse communities. It can be seen as part of a broader concept of cultural competence, described as a set of ‘congruent behaviours, attitudes and policies that come together in a system or agency or among professionals’ that enable effective work in cross-cultural situations.35 Culturally responsive practice and family-centred practice are deeply linked because culture profoundly shapes both human development and family structures, whatever a family’s cultural background. Understanding and responding skilfully to this is crucial to: … looking at the whole child and not just the presenting problem, looking at the whole extended family and not just the parents, and looking at the whole community and not just the family … culture is a key mediator between people and their social environments.36 Many of the behaviours, skills and values needed for culturally responsive and family-centred practice are similar, including development of respectful partnerships with families, promoting self-efficacy, understanding and respecting a family’s values and priorities, and working skilfully to adapt services to each family’s needs. Family-centred practice can help services improve their relevance to diverse families and communities in Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 19 their catchment37 because of the centrality of (often extended) family to the lives and identity of people in Aboriginal communities and in many CALD communities. The principles and basic approaches to cultural responsiveness with Aboriginal and CALD families are similar, but the practices and key issues are very different. This is in part due to cultural differences, but also because of Aboriginal communities’ experiences of colonisation, institutional racism and exclusion. Many CALD families also experience racism,38 and some have experienced colonisation. Yet their origins – like those of all non-Aboriginal or Torres Strait Islander people in Australia – are in migration, whereas Aboriginal and Torres Strait Islander people are the First Peoples of this land and custodians of the world’s oldest continuing cultures. Working respectfully with Aboriginal families requires professionals to engage with the strengths and survival of Aboriginal people and the adverse impact of colonisation: the loss of land, life, resources, power, language, culture, community and family. Culturally responsive practice is therefore about addressing discrimination and supporting diversity by recognising culture, and ensuring it informs all aspects of service provision: from intake, assessment and planning to implementation, monitoring and evaluation. Working with Aboriginal families and communities Aboriginal people experience 1.4 times the rate of disability of the non-Indigenous population nationally39 but are under-represented in disability and ECI services. 40 Aboriginal people with a disability are generally cared for within communities and families,41 but they and their families also need opportunities to access highquality, culturally respectful services and supports. Increasing engagement with Aboriginal families and communities requires that professionals learn about families’ cultural needs and address the ongoing impacts of colonisation. For example, Aboriginal people’s experiences of dispossession, removal of children and ongoing discrimination (including from services) 42 contribute to their self-exclusion from services, and shape dynamics between professionals and families. Partnership is crucial to increasing engagement and building capacity. Mainstream agencies and professionals must actively engage with Aboriginal families and communities, and learn from and partner with Aboriginal community-controlled organisations (ACCOs). This will enable them to: build trust and connections with the community and with families over time provide more accessible information to families about support options offer Aboriginal families the choice of receiving support from Aboriginal or mainstream services, or from both, working in partnership (choice, self-direction and self-determination are important for all families, but have an added dimension for Aboriginal people given the historical context) build Aboriginal families’ skills and knowledge, and provide culturally respectful services and supports. Partnership can include formal agreements and protocols between services. For professionals it can include networking, secondary consultation, referral relationships, co-case management and project work: There might be an Aboriginal worker who works well with community; he’s respected so much that everybody goes to him, and not to other workers. If he can work together with another worker, and teach them, mentor them, and show them how to communicate properly, if that is a respectful process, then the other worker will get that knowledge, and peer support. – Jody Saxton-Barney, Victorian Aboriginal Disability Network The Victorian Aboriginal Child Care Agency’s (VACCA’s) Aboriginal cultural competence framework43 offers helpful strategies for professionals and services to build productive and respectful partnerships with ACCOs, Aboriginal workers and Aboriginal communities, while the Department of Human Services’ Enabling choice44 booklet also provides guidance. A holistic approach and broader partnerships are also important because, for Aboriginal families, disability is often combined with the impacts of chronic disease and other stressors. In 2006, for example, 36 per cent of Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 20 Aboriginal parents nationwide caring for a child with a disability aged under 12 had a chronic disease themselves.45 Many families have experience of contact with many different kinds of services but not necessarily of receiving support that meets their needs. This makes good communication between services (with a family’s permission) and taking a case history before working with a family very important. Learning to support cultural respect, responsiveness and safety For some Aboriginal communities, there is no cultural concept or generic term for disability. For many it is not separated from health or other social concepts. 46 One study found that in some Aboriginal cultures people were not referred to as having a disability – disabilities were only discussed in relation to the tasks that they prevented a person from doing. Disability was not seen as affecting a person’s place in the community kinship system or, necessarily, all of their roles and responsibilities. 47 Having some understanding of the specific cultural concepts related to disability, illness and care might influence the language that professionals use when relating to families, including discussion about what role services might play. Family-centred practice with Aboriginal families requires professionals to have some understanding of a family’s kinship network, and often to engage at the community level, recognising the culturally specific role of extended families, Elders, grandparents and other relatives with responsibilities for culture and care: Caring is a shared responsibility. If your duty is to care for a child and you can’t because of other responsibilities – for example, a duty to country, a duty to Elders – then you ask members of the family to care for the child. So, if a professional is working with a family, they should not assume that a mother is the only primary carer for a child. Because of the dynamics in the family, if she’s given permission for her sister or her aunty to look after that child, then the child is in their care – they can make the decisions while the mother or father are not there. – Jody Saxton-Barney, Victorian Aboriginal Disability Network Professionals also need to understand the importance of cultural safety to children and young people’s wellbeing.48 Supporting cultural safety might include ensuring children (for example, those at special school or living in care) have ongoing opportunities for connection with culture and community and other children from their background. It might be especially important to support the cultural needs of children and young people whose specific medical needs or disability affect their access to knowledge, culture, community or country, or who require specific supports to enable them to receive knowledge (such as communication aides), travel to country, or participate in community festivals and other events. Cultural safety is also something that concerns families when receiving services or considering approaching a service for assistance.49 For services, creating the space for people to feel culturally safe means making Aboriginal families feel welcome. For professionals, it includes: showing cultural respect (including learning the specific appropriate ways to address and show respect to Elders and others within a particular community) being willing to learn and challenge their own assumptions and values being committed to ensuring their practice is culturally responsive engaging in regular reflection on how power works in their relationships with Aboriginal families. Reflective practice and feedback from families are crucial to achieving family-centred practice, and can also support the building of culturally respectful practice. There are many tools available for this purpose. VACCA, for example, describes how its cultural competence framework can be measured in relation to government standards for community organisations, 50 and offers a cultural competence continuum51 that can help professionals reflect on the extent of their own and their agency’s cultural competence. When services and professionals are culturally sensitive, responsive, reflective and respectful, this creates space for Aboriginal families – including prospective clients – to feel culturally safe and to ‘be themselves’.52 This makes it more likely that they will be open with service providers, giving professionals a fuller picture of their needs, and making it more likely that work will achieve its intended outcomes: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 21 Workers need to have an understanding of kinship, and of cultural safety. But even if they don’t understand the family’s kinship and history, an understanding of cultural safety will allow them to actually work with people, and learn as they go. – Jody Saxton-Barney, Victorian Aboriginal Disability Network Working with culturally and linguistically diverse families Partnership is also vital to culturally responsive practice with CALD families, and to building relevant professional and organisational capacity. 53 The most important partnerships will always be with the families that the professional is working with. Other important strategies for building cultural responsiveness include secondary consultation, referral and co-case management with staff in specialist services (including migrant resource centres and others with cross-cultural expertise and networks). Where available, these organisations also provide a key service option for CALD families: People are more likely to access supports in the company of others of a similar cultural background. Further, people with a disability from CALD backgrounds usually identify more readily with people from similar cultural backgrounds than they do with people with a similar disability. 54 Culturally responsive practices with CALD families include: communicating through accredited interpreters when a family requests one or when effective communication is not possible without one, and using language services skilfully (including receiving training on working with interpreters) offering information to people about their service options in an appropriate language and format because lack of information is a key barrier for CALD families (consultation might be needed to determine what information, language and format is most appropriate, as many refugees and other migrants have experienced disrupted education and have low literacy in their first language) working in partnership with ethno-specific and multicultural agencies to increase knowledge, skills and capacity to reach and work with CALD families and communities learning about specific aspects of a family’s culture, including their cultural beliefs and practices in relation to disability, family and who is responsible for caring for people with a disability, which influences whether the professional might suggest respite or other forms of support, and who in a family the professional should communicate with learning about diverse understandings of human development, raising children and the knowledge and skills appropriate to children of differing ages; for example, knowing that in some communities all children are routinely hand-fed until age five might influence the selection of milestones for assessing a child’s development, or the design, delivery and review of services and supports shaping services and supports to address relevant aspects of cultural difference – for example: a community’s religious practices might influence the timing of service delivery; attitudes to gender might influence the allocation of staff to a particular family; and attitudes to leisure might influence activities. As with Aboriginal families, culturally responsive practice with CALD families requires organisational capacity and commitment – the tools, policies, systems and training – to support good practice. This includes assessment tools that ask about families’ language, cultural and religious needs. Professional development is also important, for example, in working with language services and around specific issues relevant to working with disability in the organisation’s catchment. The National Medical and Health Research Council’s (NMHRC’s) Cultural competency in health document describes the need for action on cultural competency at multiple levels: in family–worker interactions, in professions (within pre-service education or professional standards), in organisations and in the service system as a whole.55 Learning to support cultural responsiveness Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 22 Culturally responsive practice with CALD families requires that professionals learn about families’ culture and context. The latter can vary for many reasons, not least their migration experience. For example, extended family plays a richly supportive role in many cultures but is unavailable to many refugees and other migrants: Normally in families [from my culture], extended family lives together. Not here. We have no family here. – Betty, member of a support group for families from a North Asian community The differences in (or lack of) services in the various countries of origin can also make it difficult for migrants to know what support is available, and where they might find it: In [my country] we don’t have these kinds of services at all so people are often not aware that the services exist. Unless they have a friend who says, ‘You can go there, you can go here’, they don’t get services. They need some kind of handbook. It is particularly hard when you don’t speak the language. – Julia, member of a support group for families from a North Asian community When learning about the culture of a family from a different background from their own, it is important that professionals remember that all cultures (including the dominant Anglo Celtic culture) are complex and evolving, and every individual and family have their own relationship to cultural norms, as this case manager (also from a CALD background) describes: Based on my personal and professional experience, I have come across situations where it is very difficult to involve family members in some cultures because of loss of face. They are very afraid of seeking help from other agencies because they are afraid that other people might become aware of their problems. But there are also subcultures within the same cultures. So that sensitivity and understanding, and insight into that particular cultural situation are critical. It can be a challenging area for anyone. Each family is different; each individual is different. Some cultural beliefs and practices can have negative impacts. This applies as much to mainstream beliefs and practices as to those of minority communities. Some are positive and protective. When attempting to understand how a cultural practice impacts on children, young people or families, professionals should be wary of the subtle power of stereotypes. Many cultural beliefs and practices are complex and sometimes not well understood by professionals. Secondary consultation can be invaluable, but the most relevant source of information about a family’s culture will be family members themselves. Pull out Box - Personal Perspectives: a family support group Consultations for these guides included group interviews with parents in support groups for several CALD communities. Members of a group from one South-East Asian community discussed how a professional’s interpersonal qualities and skills could make a big difference. ‘If on the first day you have a good worker who knows the right questions to ask and is friendly and warm, it can open up the person,’ one parent said. ‘If there is no friendliness there, then it blocks everything. If someone understands me I feel released. If they listen with no understanding it makes me heavy. The interpreter needs to be good too. If the interpreter shows arrogance we can’t open up.’ A number of parents talked about the impact of beliefs about and attitudes to disability in their community. ‘Traditionally, we believe that a child has a disability because the family did something wrong in a previous life, which is why we feel shame,’ said one. Another related an experience in her place of worship of her daughter being laughed at by children she wanted to play with. ‘I felt so much pain. I felt very angry. They were just kids, but maybe in their family their parents didn’t teach them that some people are different. After this, I didn’t want to take her out for a few weeks.’ Skilled, open, respectful questioning can ‘open your heart,’ one parent said. Another said that she had not told friends or colleagues about her daughter with a disability until the daughter was seven. ‘I kept it inside and I felt very heavy. I didn’t know how to talk, how to start to talk, how to open the story. After the first time of telling my story I felt released. It became easier each time. When I can’t talk, I feel like a block is in my heart.’ The group also discussed the importance of professionals recognising that not all children or families in their community are the same. ‘They have to listen to us,’ one said. ‘Because not all of us want to follow the same care.’ It was also important that professionals recognise parents’ lack of knowledge of the system. ‘When the case manager comes to talk with the families, they should explain to the parents more clearly about the funding and Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 23 how it can be used,’ one parent said. ‘Usually they don’t explain things unless I ask questions. The problem is, [my community] don’t know the right questions to ask.’ Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 24 3 Family-centred practice model A model for everyday practice A practice model can help professionals to better understand and implement family-centred practice by breaking down key concepts. These guides use a model developed by American researchers Carl Dunst and Carol Trivette,56 and also draw strongly on the work of Australian researcher Tim Moore and others 57. The model divides family-centred practice into three key elements (see Figure 1) – practices that build relationships, practices that support choice and participation, and technical quality – and associated aspects. Figure 1: The three elements of family-centred practice Adapted from Dunst and Trivette, 2007 The following chapters explore each of these in turn, discussing key practice issues drawn from the experiences of families, young people and professionals. They include practice examples, tips and ideas. Many more practice tips are contained in the sector-specific guides, alongside good practice scenarios colour-coded to the practice model elements for easy reference. Element 1: Practices that build relationships These are professionals’ values, behaviours and skills that help build positive relationships, especially with children, young people and families. The model breaks these elements into two aspects: the professional’s beliefs, values and attitudes; and the professional’s interpersonal behaviours and skills. A number of relationships are important to family-centred practice with children, young people and families. These include relationships between: children and young people and their families children, young people, families and the professionals and agencies that work with them professionals and their colleagues and supervisors organisations within and beyond each sector organisations and government. Tim Moore and others58 point to commonalities in positive, effective relationships between managers and staff, and between professionals and families.59 Therefore, organisations that support staff to work in family- Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 25 centred ways also create a culture of mutual respect and collaboration for staff and service users. Moore also suggests a ‘cascade’ effect, whereby the relationships between organisations and government influence those between organisations, which influence those within organisations and so on. Consultations for these guides particularly highlighted the need to improve relationships (including communication, coordination and integration) between the professionals and organisations involved in supporting children, young people and families. Element 2: Practices that support choice and participation Victorian policy imperatives in relation to family and individual choice strongly underpin this element of family-centred practice. The literature suggests that this is the most effective element of family-centred practice for improving outcomes for children and young people.60 Research also shows that while many professionals understand the importance of active listening, empathy and sensitivity, fewer excel in practices that help children, young people and families make meaningful choices or take action on their on behalf.61 The first aspect of this element is about empowering children, young people and families to make informed choices about services, set goals, explore which resources might help meet them and take action to get them. The second aspect is about ensuring children, young people and families have options that meet their needs. It requires professionals and organisations to think creatively to help shape support and services to people’s needs and preferences, and to recognise and respond when these change. Element 3: Technical quality Families rely on professionals to have the knowledge and skills required to deliver high-quality services and supports. Within family-centred practice, technical quality is about professionals applying their knowledge and skills – their expertise – in ways that impact positively on families, children and young people. Professionals and services need to see the knowledge, skills and behaviours required for good familycentred practice as critical areas of expertise in themselves. Professionals acquire and build expertise through their pre-service education (including vocational courses in disability services, teaching, social work, physiotherapy, speech pathology, occupational therapy and psychology), on-the-job experience, supervision, reflective practice, networking, secondary consultation, reading and professional development. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 26 4 Practices that build relationships: values, attitudes and beliefs Key messages Research shows that positive relationships between children, young people and families and their service providers are critical, and that these should be open, mutually respectful, trusting and collaborative, based on shared decision making and partnership. These relationships are deeply affected by the professional’s own values and judgements, including about those they work with. Professionals should understand how their values affect their interactions, challenge any negative ‘stories’ that can arise about those they work with, and practise engaging with people on their own terms. Professionals can build trust and engagement by respecting families’ choices and values (including when they differ from the professionals’), addressing discrimination, and working to transform traditional ‘power over’ dynamics of professionals and clients to relationships of collaboration and collective empowerment. Positive relationships are critical to providing services that support children, young people and families to adapt to the changes that disability bring to their lives.62 Australian and international studies have identified the characteristics of such relationships: they are open, mutually respectful, trusting and collaborative, based on shared decision making and partnership. 63 Relationships are two-way, shaped as much by the experiences, behaviours and values of children, young people and families as by those of professionals. People’s prior experiences of services are critical. If they are less than positive, or not family centred, it will take time to build trust, optimism and a sense of partnership: Validating the parents’ past journey is very important – the grief and the chaos that they’ve had to deal with. I’ve had clients say to me, ‘You’re case manager number eight’. I’d open at a blank page of my notebook to say, ‘This is our new beginning. This is where we start together.’ But first I would give them time with the book closed, to tell me what case managers one to seven did wrong. – Case manager Looking within We all bring our own values, attitudes and beliefs to every relationship and interaction we have. We rarely state them aloud, but they underpin everything we say and do. Professionals need to understand what this means for their relationships with the children, young people and families they work with. Family-centred practice asks professionals to demonstrate certain values, including that families hold significant expertise about their children’s needs and can successfully adapt to challenges in their lives. It isn’t always easy to hold onto and demonstrate these beliefs. Resources are limited, support systems complex and some families are dealing with multiple stressors, not all related to their child’s disability. Professionals need to respect families for who they are and engage with them as they are. Families highly value professionals they don’t feel judged by: A good respite worker is one I never feel judged by if I haven’t cleaned my house, or ironed my top. Sometimes they come in, and the house will be an absolute mess. They never judge what’s going on. Maybe I’ve been up all night with Emily, they don’t know. – Amy Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 27 Families can feel judged even if that’s not the professional’s intention – sometimes with serious consequences. The response Cathy (see box) first encountered on seeking services for her family stopped her doing so again for years. Other families have felt judged by professionals when they were unable to live up to their unrealistic expectations: One therapist gave me this wonderful sensory program I was supposed to do with Melanie every two hours. When I tried to explain to her that that was really hard, she had no concept. I felt a real sense of judgement, that I was a bad mother because I wasn’t willing to give something a try. I did try for about two weeks, but it didn’t make a difference, and it just about killed me. – Kate Many professionals strive not to be judgemental. Yet everyone makes judgements sometimes – it’s part of being human. What matters most is what happens next: how aware professionals are of their values and judgements, how they challenge them, and how this affects their interactions. It can help if professionals: become more aware of their own assumptions and values, and how these affect their interactions reflect on situations that make them uncomfortable, and seek support to deal with them better through reading, supervision or reflective practice with colleagues challenge any negative ‘stories’ that can arise about children, young people and families in a sometimes deficit-focused system value the knowledge and experience of children, young people and families, however expressed practise engaging with people on their own terms. This does not mean that professionals should not act on concerns about a child or young person’s safety – this is a critical responsibility (see page 54). Nor does it mean they cannot respectfully challenge parents or caregivers if they have strong concerns about the impact of their choices. A critical factor in parents and caregivers feeling accepted is that professionals accept and value their son or daughter with a disability (see Cathy’s story, page 29), and perhaps even offer additional insights about them: We come from a strengths base and seeing people’s gifts. One man said to me, ‘It’s so amazing to meet people who value my son in ways that we do – who care for him, but who also see how amazing he is in other ways that we don’t because we’re so full up with the day to day’. – Service coordinator The importance of values Every person’s deepest values are shaped by a multitude of factors, including their culture, ethnicity, race, ability, health status, history, socioeconomic status, location, language, beliefs, education, lifestyle, personality, life experiences, politics, family make-up, gender, sexual orientation and spirituality. Most of the time our values are invisible to us. They are what we grew up with; they shape our daily lives. Often we take them for granted. Sometimes we also take for granted that our values and ways of doing things are ‘normal’. But everyone has their own values and ways of doing things. Being sensitive to a family’s values means finding out how things work in that family, from big-picture questions around their support needs, to many aspects of how parents and caregivers want their child to be cared for. Even when families desperately need assistance, it can sometimes be too stressful to deal with professionals who don’t respect their values and needs: Most people find it really hard having strangers in their home. One family reduced the support they were getting from another organisation because it was too hard … [Their staff] had the skills, but culturally or values-wise they weren’t on the same page, and that was really stressful. Sometimes, in the moment, it’s easier not having another person around. The family might know that in the long term they’ll be exhausted, but today, it’s just too hard. – Service coordinator Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 28 Professionals should be especially careful to ensure they understand and respond to the values of people from minority communities, such as Aboriginal, CALD and same-sex parented families, and others whose life experience might be very different from their own. Responding meaningfully to the values of families can sometimes challenge not only the professional’s own values but also those inherent in the systems and processes they work with: Working with Aboriginal clients is interesting because they have different values. I wrote a plan recently for an Aboriginal client. All they wanted was things outside the guidelines. You could see that they just had different cultural values. The Aboriginal community really values their mob hanging out and spending time together. – Facilitator Tools such as general guidelines are important, of course. But flexibility is also key to family-centred practice (see chapter 7). This includes ensuring that processes and practices are culturally informed. Pull out Box - Personal perspective: Cathy, Richard, Cameron, Angela and Natasha Several families reported having felt judged for seeking support for their child or family, sometimes with profound consequences. Cathy and Richard’s middle child, Angela, has an intellectual disability and issues with mobility, hearing and sight. Their oldest, Cameron, was recently diagnosed with Asperger’s syndrome. When the family first sought services for Angela, says Cathy, ‘the message was, “Yes, you’re entitled to support, but no, we can’t provide it because your needs aren’t as high as other families”. I was extremely angry and hurt by that. You’ve got your own huge emotional struggles, and that just compounded it enormously for me. I pulled my head back in and didn’t ask for anything for a few years.’ Eventually a professional encouraged them to try again, and the family gained case management and other supports. Angela’s after-school program has been a particularly positive experience. ‘The coordinator is lovely,’ Cathy says. ‘She said, “I hope you don’t mind me saying this, but I just love Angela”. It was really beautiful. I said, “I don’t mind. I think I prefer it”. She gave me little insights into Angela [too]. I could see she had a really good, intuitive understanding of her as a little human being, and that was precious to me.’ As with the family’s initial experiences, the message from Cameron’s high school has been, ‘You’re asking too much,’ Cathy says. However, this time, she’s had great support to advocate for her son’s needs from Cameron’s speech therapist. The family’s case manager has also helped by liaising with the year level coordinator, ‘providing strategies, and visiting Cameron, to see how he learns and to help him, in conjunction with strategies the speech therapist has given us’. Discrimination, safety and trust Many families need to feel some level of trust to openly express their needs and values to professionals. In work with Aboriginal and CALD families, the concepts of cultural respect and safety 64 are critical. If families do not feel culturally safe, they are less likely to be open with mainstream service providers about aspects of their lives they perceive as highlighting their differences from the Anglo Celtic mainstream.65 According to a recent VicHealth report, the discrimination experienced by Aboriginal and CALD communities (including from services) is rarely blatant. More often it takes the form of discomfort, underpinned by a belief in ‘the insurmountability of cultural differences’, which sees some groups not as ‘inferior’ but different in ways that threaten social cohesion.66 Professionals need to challenge such attitudes within themselves and when they are expressed by others. When they do so, and are open, responsive and non-judgemental about the many ways that families differ, this counters people’s negative experiences and helps to build a sense of safety and trust between them and their service providers. Same-sex parents and lesbian, gay, bisexual, transgender and intersex (LGBTI) individuals are also less likely to develop open, trusting relationships with health and other service providers who judge or discriminate against them, or assume they are heterosexual. In one Australian study more than a quarter of same-sex parents reported negative experiences of their children’s health care related to their own sexual orientation.67 Some researchers draw a direct parallel between ‘cultural competence’ and the behaviours, knowledge and skills needed to offer appropriate services to LGBTI people. 68 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 29 Evidence shows that family-centred approaches are critical in supporting parents with an intellectual disability69 but that attitudes among service providers are too often characterised by disrespect, stereotypes and the presumption that they are incompetent parents. This can transfer into systems and processes, even in specialist disability services. One Australian study found that although parental IQ is a poor predictor of parenting competence,70 the classification ‘intellectual disability’ was frequently used in assessments ‘to imply a range of parenting deficits, including reduced capacity to learn appropriate parenting behaviours’. 71 As with other parents and caregivers, those with an intellectual (or any other) disability require services and supports that meet their needs and preferences and enable them to make meaningful choices for themselves and their children. Discriminatory attitudes towards parents with an intellectual disability are obstacles to family-centred practice, preventing professionals from ‘observing the family’s strengths, from putting helpful supports in place, and from working towards promoting family connections’. 72 Sharing power Perhaps the most important value that family-centred practice requires practitioners to hold is that children, young people and families can (and should be able to) make their own choices, direct their own supports and obtain the assistance they need to live the life they choose. Whoever the professional is working with, enacting this requires insight into the power dynamics in the relationship and a commitment to partnership and sharing power. Family-centred practice researchers refer to the need to transform ‘power over’ dynamics that characterise medical model approaches to ‘power with’ relationships of collaboration, information and resource sharing.73 This shift is happening in many sectors, with changes in approaches to funding, assessment, planning, delivery and review of services and supports. Even simple service delivery changes can support the process, such as arranging appointments to fit working parents’ schedules. Professionals should be mindful of the power and authority they continue to hold by virtue of their status, expertise and access to information: Even though we don’t see ourselves as powerful figures – it doesn’t matter how much we aim at a partnership – we are going in with expert knowledge and are being paid as professionals. That does create an uneven relationship no matter what. It’s about how you exercise that, whether you see it as power or influence. – ECI service manager Many professionals have the power to impact on a family’s access to resources, whether directly or indirectly (for example, by recognising a need and offering referral). Individualised funding is changing this to an extent. Nevertheless, professionals need to be aware of their power to recognise and respond to families’ needs (or not – see Amy’s story, page 31), including how they respond to people’s expressions of need: I said my son had all these needs and they said it is impossible to get funding for all these needs. I feel like a beggar asking for things. It is embarrassing to beg. – Fatima, member of a support group for families from a Middle Eastern community Professionals also need to be conscious that some people find it more difficult than others (for various reasons, cultural or otherwise) to ‘speak freely’ to people in authority. Winnie (a member of a support group for parents of a North Asian community) had a positive experience of planning for her child’s needs through student support group (SSG) meetings at primary school. But at high school she found the meetings far too brief, and that the school had already set her child’s goals and written her individual learning plan: They just say, ‘Are you happy with this?’ They say I can change it but I don’t feel comfortable. [In my culture] people are often very reserved. The relationship between the parent and teacher needs to be good before you feel that you can comment. [In my culture] we need a good relationship before we can speak freely. Perhaps I need to not be so gentle … not so polite. The power dynamics in a professional’s relationship with a child, young person or family are also affected by broader power structures and family stressors, including lack of access to information, education, financial resources and support networks.74 Families on low incomes are likely to have less choice about which services they use. Those without informal supports can find it particularly difficult to access some services, Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 30 for example, if transport is difficult, or they cannot get childcare for the siblings of their child with a disability. Prior experiences can also have a profound effect. Many Aboriginal families have negative experiences of mainstream services and most have at least one member of the Stolen Generations in their close family. Some refugees or other migrants might have had very negative experiences of authority in their countries of origin or on their journey to Australia, and might perceive government-funded services as more authoritarian than they intend to be. Ultimately, professionals need to move beyond ‘power with’ dynamics, and work towards what some researchers describe as ‘power through’ relationships, which promote ‘collective empowerment, a process through which … all participants (professionals and families) increase their capacity and mastery over the resources needed to achieve mutually desired outcomes’, and which can also result in benefits for the wider community.75 In this process, says Tim Moore: … power is no longer simply about controlling events and processes, but it is also about building the capacity of communities. All participants gain in competence, abilities, resource acquisition, and capabilities without taking power from others. This results in increased satisfaction by all participants, parents and practitioners alike.76 Pull out Box - Personal perspective: Amy, Colin, Emily, Anthony and Lisa Amy and Colin’s middle child, Emily, has complex medical needs and neurological issues, and their youngest, Lisa, has a learning delay. The family most appreciate services that recognise the whole family’s needs and don’t judge or make them ‘beg for help’. ‘For them to [recognise] and justify a need makes such a difference,’ Amy says. This isn’t just about what support the family receives. It’s also about how professionals respond to their needs. ‘A good case manager would say, “Right, you’re having trouble getting Emily ready in the morning, do you think it would be useful having someone help?”,’ Amy says. ‘Rather than me saying, “She’s so heavy in the morning, do you think it would be possible to have someone do an hour shift?” and they say, “Well, I don’t know, we’ll see what would be possible”. It’s all in the way it’s delivered because the outcome probably isn’t any different.’ Good workers follow the family’s lead, Amy says, and then ‘they just blend in and get on with it, and help us all. Our good respite workers don’t just help with Emily. They interact well with Anthony and Lisa. Lisa begs to stay home with one of the workers. She really looks forward to those times.’ Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 31 5 Practices that build relationships: interpersonal behaviours and skills Key messages Interpersonal qualities and skills that support positive relationships include: listening well; being tuned into non-verbal signals; engaging respectfully with children and young people; communicating well across language, educational and other barriers; connecting families with other families; and skilful gathering of information, including by asking the right questions and empowering people to ‘tell their story’ if they wish. Professionals need to be emotionally responsive to families, as appropriate to their role. This includes expressing themselves with care, being sensitive to the stressors in people’s lives, affirming the importance of family in children and young people’s lives, building trust and referring appropriately. A critical issue is communicating medical and development issues to convey accurate information and a sense of hope. Strong interpersonal skills are needed to support people to make informed choices by offering them information, addressing their concerns, helping them to make sense of technical or conflicting information, and to weigh the risks and benefits of different options. Professionals should not dismiss people’s online research, but rather offer high-quality information, ask people about their online researches, and offer to read and discuss any information they find that raises concerns for them. A key challenge is when resources are inadequate to meet people’s expressed needs. Professionals should recognise people’s needs (even if they cannot all be met by specialist services), ensure they understand them fully and work with families to find other ways to meet them if necessary, for example, through a combination of informal, universal and specialist supports. Regular communication is critical, including about the level of services available through specific funding, or remaining to the family in a given period. Families need to be kept informed of their child’s experiences, progress and any issues that arise, especially if the family is not present when the professional is with the child or young person. With adolescents and young adults, this must be balanced with the young person’s right to privacy, except where a duty of care issue arises. Professionals must also inform families about any changes that might affect services. Professionals need strong interpersonal skills and behaviours to work well with children, young people and families. Such skills are critical to building positive relationships, and are complemented by the personal strengths that tend to characterise professionals in this field, including empathy, warmth and sensitivity. One behaviour essential to family-centred practice is being available to families and young people. This can be as simple as providing contact details (especially if the family is usually not present when the professional sees their child) or having an ‘open door’ policy, which Melissa (see p.31) appreciated at her daughter’s kindergarten and now does at her mainstream school. Other key behaviours and skills include good communication, emotional responsiveness, supporting informed decision making, drawing out families’ knowledge, communicating sensitive information appropriately, responding appropriately when resources are inadequate, engaging directly with children and young people and keeping people in the loop. Communication Listening Skilled listening builds trust and is essential to enabling service providers to gather the information they need to plan effective supports with families. Many professionals are good listeners, and yet consultations for these guides revealed that too often families and young people still do not feel heard. Some families Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 32 described professionals as sometimes too solution focused, and as less than sensitive to where they were on their emotional journey: It’s about being quick to listen, and slow to give advice until you really know the family and understand … The most positive interactions have been where people acknowledge the challenges but speak to me in an empowering way – acknowledge and hear what I’m saying, and try to work with me. Sometimes people cut you off, don’t want to listen. It’s also about understanding where I am on the journey. At times I’ve been ready to hear things, and at times I need to talk. The people I connect with seem to understand those phases a little better. – Kate Professionals need to hear what a person says on that person’s terms, not as it relates to the professional’s own life, role or ideas for ‘fixing the problem’. Yet the reality is that from time to time most professionals get distracted and stop listening well, for reasons ranging from tiredness to discomfort with some aspect of the situation. Reflective practice might help professionals gain insight into when and why their listening skills falter (see chapter 10). Tim Moore also refers to ‘mindful practice’, where professionals cultivate greater selfawareness and management of their own emotional responses in their interactions with families. 77 Non-verbal communication Professionals also need to be sensitive to what is not being said, which some Aboriginal people call ‘deep listening’.78 For special education school principal Sue, her ability to do this was strengthened by having had a daughter with a disability (Nicky had atypical Rett syndrome and passed away at 19): Sometimes it’s about hearing what isn’t said. We have a beautiful garden with a bench, and one mum with a severely autistic daughter sat down beside me and said, ‘Didn’t get much sleep last night’. I said, ‘Don’t you just wish they could sleep, even an hour at a time would make such a difference’. She just burst into tears and said, ‘Most people think that I mean I got up a few times in the night’. But of course her daughter hadn’t been to bed at all. For that mum, a bad night was on a whole other level. If you haven’t had that experience, you can empathise, you can sympathise, but you can’t know what it’s like. Sue also says that: With the best will in the world, we often end up telling families what they should be doing. And families end up agreeing with us, to protect themselves. Families become very adept at ‘managing’ professionals. To avoid this it’s important that professionals tune into non-verbal cues, such as hesitation, pauses, tone and body language. Non-verbal communication is largely unconscious but very significant in conveying underlying emotions or attitudes. Remember also that non-verbal communication is not universal but has a diversity of cultural meanings. Professionals need to find out what cues to be aware of when working with families whose cultural background is different from their own. Professionals need to tune into non-verbal cues and to be aware of what they themselves are signalling. Research demonstrates that families often know when a professional’s attitude is not consistent with their words, for example, when they express care they do not feel. 79 In such cases non-verbal cues are almost certainly the give-away: We work with families often in their most vulnerable time. We can unwittingly have a huge influence by even a roll of the eyes. So we have to be very careful. – ECI service manager Professionals should be especially conscious of how their non-verbal communication conveys respect (or otherwise). What this requires depends on cultural context. For example, grandparents and Elders in Aboriginal communities have particular authority and should be treated with deference. Showing respect is also about knowing what is appropriate to ask during interactions with children, young people and families: There was one person who came as a replacement once, who started asking me questions about my disability, like what disability did I have and how did I acquire it. I didn’t really think it was appropriate to have to explain my medical history to someone who is just there to help me with my housework. – Caitlin Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 33 Communicating directly and respectfully with children and young people Non-verbal communication is particularly important in engaging children and young people. Asking them what they think shows respect for their opinion, but moving to their level, using appropriate communication methods and giving them time to respond, shows the depth of a professional’s commitment to inclusion, and helps to build a relationship with young people and their family: You often win the heart of a parent if you can engage with their child. I don’t go there consciously thinking that, it’s just something I do naturally. I’ll be on a home visit, sitting on the floor with kids crawling all over me. Sometimes I’ll do a visit with a young worker who doesn’t have children or young siblings or nieces or nephews. They will sit at the dining room table automatically. If the carer is grandma, she’ll put coffee on the dining room table, so your cue is to sit there, but most of the time I’ll just sit on the floor with my back against the couch. I’ll always do it in front of young practitioners. On subsequent visits with them I’ll find that they’ll do it too. – ECI professional In consultations for these guides, many parents and caregivers spoke of how much they appreciated professionals who engaged directly and respectfully with their son or daughter with a disability: One of the assistants was the most wonderful lady. She was not only really bubbly and friendly to me, but she acknowledged Jamie, and talked to him. At that point nobody really talked to Jamie or acknowledged him whenever I took him anywhere. The fact I can remember it 14 years down the track – it made a huge impact. It was the sense of acceptance it gave to me that was really significant. – Kate And of course, children and young people also appreciate such efforts: I like it when people aren’t patronising, and respect and talk to me like any other person. As a young person, sometimes your needs aren’t listened to as much, and parents can dictate what happens. I appreciate my opinions being heard and having as much say in the services I receive as possible. – Caitlin Pull out Box - Personal perspective: Melissa, Roland, Michelle, Stefan and Tad Melissa and Roland tried out a number of educational environments for their daughter, Michelle, who has Down syndrome. Her first (mainstream) kindergarten ‘was not family centred,’ Melissa says. ‘The door opens at 9 o’clock, they lock the door, [then] you wait till your child comes out.’ The ‘open door’ at Michelle’s second kindergarten was much better, and Melissa felt ‘included in everything that happened’. The disability service that ran it also ran a weekend playgroup, where Roland took Michelle and her two brothers, and a siblings program that Michelle’s brothers still enjoy. Michelle’s first school was safe for her in that she couldn’t ‘abscond’ but gave no classroom support, Melissa says. ‘To bring the teacher new strategies to help Michelle was a burden to her rather than a challenge …There was a table up the back where Michelle could go if she didn’t want to do work’ – a strategy the teacher persisted with despite Melissa’s protests. It contributed, Melissa says, to Michelle developing ‘a lot of behaviour issues’ by year’s end. The school’s psychologist was also reluctant to accept Melissa’s advice about her daughter (see page 71), which led to an incorrect assessment of Michelle’s IQ that made her eligible only for a special development school (SDS), if the family shifted her from mainstream education. Melissa found the SDS similar to Michelle’s first kindergarten in that children were ‘dropped at the gate’. Her concern that the SDS couldn’t meet Michelle’s learning needs was also justified. The family had to move all three children to Michelle’s current (mainstream) school, but it’s been the right choice. The school is inclusive, willing to support Michelle and her brothers, and both the teachers and leadership are responsive if Melissa raises concerns. Communicating across language, educational and other barriers Professionals should speak in plain language appropriate to people’s educational level (without patronising them) and avoid jargon and technical terms. However, they also need to help people gain the knowledge they need to navigate the service system, including how to decode acronyms and technical language: I asked my case manager, ‘In terms of money, where does it come from?’ She said, ‘Oh, you don’t need to worry about that’ – but I was asking. She said, ‘I’m trying to get you another ISP [individual service Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 34 package] for next year’. I didn’t even know I already had one! So I’m trying to use the right terminology to get that information. I still don’t feel like I have enough control. – Cathy People with limited English should be asked if they would prefer to communicate through a qualified interpreter (see chapter 9). It isn’t always practical to provide face-to-face interpreting in every encounter (for example, during every respite or attendant care session), but service providers should offer an interpreter during assessment, planning and review sessions, and first visits by support workers. Telephone interpreting is also a crucial support in emergencies or if information is needed (by either party) quickly. Using a professional interpreter enables both parties to communicate much more complex information, with greater accuracy, and makes it more likely that service users will feel confident to ask questions. Critically, using an interpreter enables professionals to get an accurate understanding of the situation, needs and choices of the person they are working with, making it more likely that supports will meet their needs. Professionals must always use professional interpreters, never family or friends. This helps ensure that: interpreting is accurate and of high quality family members are not put under undue pressure or in inappropriate situations, and can concentrate on providing support for each other and information about their own and their child’s needs important principles of confidentiality and impartiality are not breached. These all contribute to service quality and also help protect the professional’s organisation from legal risk. Professionals need to reassure people about the rules of confidentiality for professional interpreters, and let them know that they can ask for a different interpreter if they don’t feel comfortable with the one provided. It is good practice to record the name of a family’s preferred interpreter and ask for that person when booking interpreting services for that family. Professionals should offer detailed, plain language information about their service (and the service system generally) to people who have no or limited experience of receiving services in Victoria (for example, because they are migrants or have been disenfranchised). Many CALD families’ expectations are based on the service systems in their countries of origin. Professionals should ask whether it would be useful to explain how their service, profession or therapeutic modality works, including its rationale and benefits. Gathering information Asking the right questions, whether open-ended or specific, helps professionals to elicit meaningful information. ‘What would you like to work on?’ can be daunting, especially early in a family’s journey. Service providers can get parents and caregivers talking in different ways, for example, by asking about an area of family life (‘How are you all sleeping?’ or ‘Are any routines changing?’), or respectfully observing their behaviour or mood. Some people find it easier to start with what hasn’t been working for them. We support families. We might have spent an hour with them, and then we’ll meet the case manager they have had for months, and I’ll think, ‘How can you not know x and y about the family?’ It’s about asking the right kind of questions. – Association for Children with a Disability family support worker Sometimes it is appropriate for a professional (depending on their role and relationship with the family) to move beyond questions that contribute to their understanding of a family’s situation and needs, and to ask challenging questions,80 especially if they are concerned about family members’ choices or feel there is additional information that the child, young person or family might benefit from. Professionals should be very aware of how their own values and attitudes play out in such interactions. Many professionals experience a tension between collecting the information designed to facilitate quality service delivery (such as that listed in intake forms or assessment templates) and hearing the fullness and complexity of a family’s story and needs. The latter can take much longer but can also build trust, and potentially vastly improve the quality, relevance and appropriateness of services: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 35 A lot more comes out of that hour with the family than the ‘tick a box’. You need to do that, but you can often leave it until last, I think. – Intake worker Some families need the space to tell their whole story, especially early on. Being asked the right questions can be very validating, especially if they address issues not previously recognised: It is good when they ask questions about the child but also about the family, when the questions openly address the issues a family might be facing. When a worker asks about the issues for the family it can open up your heart. – Lilly, member of a support group for families from a South-East Asian community Others do not want to have to tell their stories or explain information repeatedly, in which case service providers can assist by sharing information (with permission). Professionals also need to seek out tools and methodologies (see chapter 9) – for example, for assessment, planning or review – that help them draw out the rich knowledge that children, young people and families have of: each other’s strengths, skills and needs; the family’s and each member’s dreams and goals; and how things work in their family, including how family members work around each other’s needs. Supporting informed choice Informed decision making requires families and young people to consider both their own needs and preferences and the relevant information, for which they often rely on professionals. Many people have limited information about supports and services, especially those who have limited English or have recently arrived, have low literacy or are otherwise marginalised. Natasha, a member of a support group for families from a Middle Eastern community says: We got some help but no one explained the basic things to me. Six years later I found out I was eligible for some Centrelink payments for all of those six years. No one ever told me. Amina, another member of the group says: Workers don’t tell you the basic things because they think you already know. But we don’t know. When I gave birth to my son, no one told me I was able to get a disabled parking permit. For five years we didn’t know about this. We got many fines. Professionals should offer Aboriginal and CALD families service options targeted to their cultural community, if any are available (this might sometimes require secondary consultation or other research). It is also important always to offer them full information about mainstream services and supports. Offering information Some professionals see family-centred practice as simply ‘doing what families want’, and are unsure if they can offer input. If it is clear that a family or young person is unaware of information or ideas that might assist them, it is appropriate to ask if, when and how they would like to hear about it. Depending on the context, information might well be the family’s most urgent need: I gave a presentation about self-care to a group for people still on the waiting list. It became evident very quickly that unless those parents had information, and a few services sorted out, they weren’t going to take any time to look after themselves. I was the same. One of my kids had a brain tumour when they were little. I didn’t care about having a massage [but] I sure as hell wanted to know how I got to the doctors, and about hospital waiting lists. – ECI professional Professionals need to offer information to people in a way that empowers them to make their own decisions freely and in their own time. Any suggestions professionals offer should arise from a deep understanding of the family’s needs, priorities and concerns, and be presented as possibilities and options. It can be helpful to do the following: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 36 Check what information the family and young person think they might want, and when. Information overload is common. If people don’t have a lot of information, it might be helpful to describe the kinds of things you could tell them, and ask which would be helpful. Ask families and young people about what they might already know. This helps the professional to: avoid patronising them; address any misconceptions or misinformation they might have; engage with any beliefs and values they might express; and use language they can relate to. Check if the explanation is clear enough, and whether people want additional information. Use plain language, avoid unnecessary jargon, and help people decode the terms and acronyms they need to navigate the system. It is also valuable to collect good-quality, plain language information resources on important or common topics. Professionals might find these online, or develop them with input from service users. Many families (not only from CALD communities) would also benefit from a plain language explanation of the professional’s own service and role, and how it fits into the service system. Other useful information and supports to aid decision making include: accessible information about disabilities, developmental delays, health issues and the effectiveness of different approaches, including current research (research summaries perhaps) up-to-date information about services, supports, referral pathways, intake criteria, funding and policies assistance to make sense of conflicting information assistance with weighing up the risks and benefits of different options and approaches. Sometimes families are looking for an in-depth discussion of a professional’s perspectives on an issue: [One mother] said she’d been given quite solid information from the early intervention service and case manager about the options. But when she wanted to explore it in more depth, she got the message, ‘It’s your decision, don’t ask us to decide for you’. She said, ‘I wasn’t asking you to decide for me, I was asking for nuances, and perspectives on schools’ performance’. – Service manager Meeting people’s learning needs and supporting online research Professionals should ask people how they prefer to receive information and tailor the information they offer (as much as possible) to people’s individual learning needs. Some people prefer written resources such as information sheets, brochures and research papers. Sometimes these are available in languages other than English. Professionals might sometimes be able to have resources translated, or offer to go through them with an interpreter present. Many people appreciate the opportunity to receive information via verbal explanations, diagrams, role-plays, audio or video resources, discussion or problem solving. Many people appreciate online information and are likely to explore for themselves the wealth of information available on the internet. There are a lot of good-quality, up-to-date resources online, but there is also a great deal of information that is not evidence based, and even misleading. Professionals should not be dismissive of people’s online research. New information is always being published online, some of it high quality. Families will sometimes find credible information that professionals have not yet come across themselves. Rather than dismissing information families find, it is helpful to: check in with people regularly about what information they are encountering online if appropriate, offer to read online information that raises concerns for people and discuss it with them find and offer suggestions of appropriate, good-quality and accessible websites and downloadable resources (such as information sheets), evidence-based research papers and other online resources (including support groups, moderated and otherwise). Connecting families with other families Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 37 One of the most effective ways to help families become more informed is by connecting them with others who share their experiences: You always rely on other parents because they’re at the coalface of what’s happening right now, whereas the services aren’t always up to date. I’ve been lucky. Very early on I met someone with a similar son. I basically copied what she did in terms of early intervention and applications, and hoped. And it has worked out well for us. – Daniela For people who are geographically isolated – or can only tap into community late at night when all other tasks are done – online communities can be helpful. It is important, however, to check in regularly with families who use these sources of support, as Daniela cautions: I do access an online support group [but] it’s very confronting. There are a lot of parents who are off the edge, with their frustration with schools in particular. When my son was three I got onto that website and read the stories in horror every day. So that probably wasn’t the best choice initially. It can also be very valuable for professionals to share what they have learned from other families (while respecting confidentiality). Several families reported appreciating professionals giving them information about what might be ahead for them, and what choices might be possible in the future: Years ago a speech therapist told us to book into [a private special school]. At that stage it’s years in advance, you have no idea whether that’s an appropriate school, or a good fit for your child. But she said that unless we had her name down we’d be unlikely to have a chance of getting her in. And she was right – bless her for telling us that. It was quite confronting at that stage to think maybe Louise wouldn’t be going to mainstream secondary school. The therapist could have just ignored the issue, and not confronted me with it. But she did, and she did the right thing. And because of that experience I’ve often asked professionals questions about the future. – Jan Emotional responsiveness Consultations for these guides and the literature highlight some of the stressors that can affect families, including social isolation, financial pressures, the inaccessibility of services and facilities, discriminatory community attitudes, juggling multiple service providers, inadequate or poor-quality services, exhaustion from care-giving with inadequate support, particular stressors related to their child’s disability, 81 fears for their child’s health and concerns about how best to support their development. When families express the strong emotions that arise as a result of such stressors, professionals need to listen. Sometimes they might also need to refer the family to other supports and services. Being sensitive to people’s emotional needs also requires that professionals express themselves with care: Workers need to be sensitive to all the emotions and processes parents are going through, particularly around decision making. You have children and imagine they’ll grow up and look after themselves, and then you have a child with a disability. I never imagined I would have to make these choices. There’s no guidebook that tells me the right or wrong thing to do. So rather than saying, ‘You should be doing respite’, for example, you might ask, ‘Have you thought about respite?’ or ‘What might be the benefits of respite for Casey?’ and ‘What might be the benefits for you?’ – Donna It also sometimes requires professionals to listen to families’ frustrations (for example, about the lack of respect or family centredness of some professionals) with compassion, and to respond appropriately: For a very long time families have talked with our organisation about the sadness and frustration they feel when the knowledge they have about our child and what works for their family is not recognised by professionals. Most families have many workers constantly coming in and out of their lives. If they are not treated respectfully by them, over time the disempowerment they feel can be soul-destroying. – Elizabeth McGarry, Association for Children with a Disability Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 38 The emotional journeys that families experience are diverse and far from linear, and their lives can be stressful and chaotic, depending on their child’s condition and the supports available. The impacts can require patience, empathy and understanding from the professionals working with them: I thought, when I was a professional, that the grieving process was circular. But I found out with Nicky that it’s a zig-zag. Teachers can get very frustrated. You can have a great SSG, you’ll make plans, but two days later the parents come in and say something different. That’s the grieving process, it’s not as irrational as it would appear. Some days families will be able to talk about it, some days they won’t. I found it could creep up and hit me on the back of the head for no apparent reason. There’s a whole lot of deep understanding that most people don’t have – but it impacts enormously on how we interact with families. – Sue, principal of a special school and mother of Nicky Pull out Box - Personal perspective: Daniela, Joe, Ben and Allegra When Daniela and Joe’s son, Ben, was diagnosed with autism spectrum disorder, it answered some questions. ‘You’ve got this feeling,’ Daniela says. ‘Like “something’s wrong, I’m not coping. I don’t really like going to the zoo with my kid, and I’m not sure why. But I don’t think I’ll bother when everyone else is going today.” You become very limited socially.’ Yet the news was initially devastating, partly because of Daniela’s experience of her brother’s autism, and because of the paediatrician’s predictions about Ben’s future. ‘He made out Ben would end up in a sheltered workshop – this is at age three. I thought, Maybe he will, but he’s going to have the opportunity to do better if possible.’ Ben’s diagnosis pushed Daniela ‘right out of [her] comfort zone,’ she says. ‘I had to force myself to take some risks … [and to] become his advocate. If you don’t do it, no one else will.’ Daniela threw herself into engaging with early intervention and understanding the ‘maze’ of services. She found other parents a great source of information and inspiration. Good communication from Ben’s kindergarten was critical, especially before he could talk. ‘Without it I would have been flying blind to his behaviour, how he was developing socially. Communication lets me set up and plan the year – what needs to be done communication-wise and support-wise. Autism can be quite isolating, until you know what you’re dealing with. You can feel like you don’t fit in. Communication [also] made our family feel really welcome.’ In the past year Ben has coped admirably with a five-week trip to visit relatives in Europe, and recently finished a great first prep term at his local school. Affirming the importance of family Family-centred practice is about professionals recognising the centrality of families in the lives, care and identity of children and young people. It can help to affirm the family’s significance, verbally and in other ways, to the child or young person, and to their family and community: [The school] knew about what the family did and what Casey liked to do at home. Casey adored watching her brother play basketball – they knew about that and talked with Casey about it at school. They knew that my mother, her grandmother, was also very important to Casey. Sometimes my husband would drop Casey off to school, and they included him – he wasn’t just Casey’s dad who no one knew. And they would ask questions about the family, and they put together family books, including [Casey’s brother] Ben. – Donna Michelle did a huge poster for school about her grandparents. It’s right up in the classroom with the other kids’ posters. There’s two other kids with ethnic backgrounds, and they were saying, ‘When you go to your yaya’s house, does she make you eat this and that?’ The kids accept that as part of who Michelle is. – Melissa This can be very important during times of transition, especially those involving a change in the family’s role or a shift in who cares for a child or young person, for example, a family’s first experience of in-home or residential respite, a young person’s move to independent or supported accommodation, or when a family relinquishes care of their child, a painful process for everyone involved, as this case manager says: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 39 I worked with a young man who requires full support, who can’t move by himself. The family came to us for long-term accommodation. The father didn’t have any acceptance of his son. The mum provided care. We looked for respite, but it’s difficult to find the level of care he requires. [In the end] we found alternative accommodation. He was happy to move there, and the family was very happy. The key was family inclusiveness, even though the young man knew he was not going back. We included his mum in visiting the accommodation with him, which showed that she was still caring for him. Communicating about medical and developmental issues For many professionals a key part of being emotionally responsive is supporting families to balance optimism and realism about their child’s development.82This is particularly critical at diagnosis and early in a family’s journey, as both Alison (see page 14) and Daniela (see page 39) describe. The negative messages that some parents and caregivers receive from service providers are no doubt well intentioned; however, many prefer professionals with a strengths-based approach. In consultations for these guides, families said they want both accurate information and a sense of hope. It might be helpful for professionals to: use words that have less certainty and finality (such as ‘probably’ and ‘likely’) consider the range of possibilities for the child or young person, and not base speculation on a ‘worst case’ or textbook scenario describe the range of possibilities and the factors that might influence a child or young person’s outcomes and discuss how these might apply in this family’s situation provide opportunities for the family to ask questions later (at a return appointment or by phone). Building trust Trust is built over time. It requires professionals to listen to and value what people say, and to provide information and supports that meet their needs. For many people, it also requires some personal connection (while bearing appropriate boundaries in mind). As in any long-term relationship, there are likely to be occasions when communication falters, or when professionals make mistakes. Sometimes this does irreparable harm to the relationship, but a sincere apology can go a long way: I find that really empowering these days, to be able to stand up and admit when you’re wrong, no matter how big or small the mistake is. That’s really empowering and gratifying, and it builds trust for people to know that when you mess up you’re going to take responsibility. – Disability support worker One critical issue for parents and caregivers is that their children are safe and well supported when in the care of service providers. This requires that professionals keep families informed (see below), and respond appropriately when they raise concerns. When resources don’t meet people’s needs One of the challenges of family-centred practice is the tension that can arise from asking people what they want and then not having the resources to meet the needs they express. Some researchers have found that this can be an obstacle to practice change.83 Families’ experiences of this include professionals avoiding families (not answering their calls) or telling them there are others with more urgent needs (see Cathy’s story, page 29). Ingrid (see page 41) received an even balder response: At one stage we wanted help to pay for Ella’s childcare. I felt it was vital to her development to interact with typically developing children … In front of a room full of other people I had a worker tell me I was being greedy ... in the end we actually got the funding because [the other service] decided we needed it. Families and young people understand that resources are limited and that guidelines and priorities for funding are necessary. However, they have the right to seek the best possible services and supports for their Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 40 children or themselves. They should never be made to feel guilty for doing so or that they need to be in ‘crisis’ to receive assistance. Appropriate responses to this issue are partly about acknowledging people’s needs: One case manager was particularly good. She didn’t get us more [funding] than the others, but she would identify what would work for us then see if she could get it. If she couldn’t, well so be it. They don’t have endless amounts of money. What you can have and what you need are probably very different things. Most families understand that. But some [case managers] would come in and almost ‘contain’ what you could say you needed. – Amy Appropriate responses are also about how professionals use their communication skills to gain a deeper understanding from families about a given need and its context. Such explorations might reveal that the need can be met within the available resources or guidelines. When that is not the case, professionals need to work collaboratively with families to help them find other ways to meet the need, whether through informal supports, different sources of funding or referral to another disability-specific or universal service. Professionals also need to ensure children, young people and families are offered all the financial and other support they are entitled to, and that they are informed about grievance and complaint mechanisms. It’s also important to ensure people have an accurate understanding of the level and nature of support that a given service can provide or a funding package can support. For a variety of reasons it sometimes becomes clear that a service is not able to meet a child, young person or family’s needs. In this case, professionals have an obligation to find other options and to offer support to help the family transition out of their service (see Ingrid’s story below). Pull out Box - Personal perspective: Ingrid, Dan, Justin, Ella, Rose and Luka Ingrid and Dan have had very mixed experiences with supports for their daughter Ella (who has Down syndrome), even within one service. Like many parents, Ingrid appreciated being connected with other parents. ‘It was amazing. I have the closest friends in the world from that initial support group,’ she says. The social worker who ran the group was a great support to the family. ‘We had a big drama with Centrelink, nothing to do with Ella. They approved Austudy then took it away. We’d already moved [to a house with higher rent]. I rang up, hysterical, saying, “What am I going to do? I’ve got no money to pay the rent”. Straight away [the social worker] organised help to cover some of Ella’s childcare, she talked me through it, we got onto Centrelink and appealed.’ Ingrid feels that this social worker’s life experience helped her to have a different level of empathy and responsiveness to her concerns. “If you want to move on, let’s look at other options”.’ Ingrid was, however, frustrated with the level of support provided by other workers, and with the relevance of the supports the family was offered. ‘How does a new parent know what they need, regardless of whether their child has a disability? [Service providers] can’t wait for us to say, “We need this” … In the end I said, “I’m not getting what I want here”, and it was the social worker who said, Ongoing communication Information about service levels and provision Ongoing communication with families and young people is a core responsibility of professionals and is part of the response to the issue of limited resources. Where support hours are limited (whether due to the service’s own funding or the level of a family or individual’s funding package), service providers must clearly explain the level and duration of support available at the outset, and keep families informed regularly about how much support remains to them in a given period. This is essential to organisations’ accountability to service users and empowers families and young people to manage their supports (for example, saving respite hours Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 41 to cover special occasions or school holidays), or to seek other options if service levels are unlikely to meet their needs or risk creating other issues: The funding [for a school-based speech therapist] would only have covered a few appointments, so it wasn’t worth doing because it would be more stress for my child to have to start with a new therapist and then change. – Jan Other issues that professionals should communicate about regularly include: how changes in circumstances (such as the child or young person’s age, development stage or medical needs, or family income or employment status) might affect the services available to them relevant changes in the professional’s own role or availability (including when they will be on leave and who will provide support during that time), their organisation and sector, or in the services that the professional might be coordinating on the family’s behalf new potential sources of support, including funding packages, services and programs what the professional is learning or observing about the child or young person and their family, including their growing capacity to meet their own needs. This helps build self-efficacy (see page Error! Bookmark not defined.) and calls for reflection rather than praise. Observation – without positive or negative judgement – is more likely to open up space for fruitful discussion. 84 Keeping families in the picture Parents and caregivers rely on professionals to keep them informed about what happens for their son or daughter when they are not present, especially (but not only) if the child or young person is non-verbal. This includes, for example, telling parents and caregivers about children and young people’s experiences, progress and any issues that arise at kindergarten, school, in therapy or during in-home or residential respite. Tools for doing so include: communication books; written, email, message-text or verbal reports; regular meetings and informal ‘check-ins’ (at drop-off, pick-up or other times); service reviews; special family events; an ‘open door’ policy; and invitations for family members to be present during appointments. Professionals must also respond openly and respectfully when family members raise fears or concerns. As discussed, families must feel able to trust the professionals caring for their children. During consultations for these guides, some families described some of their service providers as not being very forthcoming with information, and feeling unwelcome to access facilities when their children were there. Sometimes service providers might find it challenging to be upfront with families, but it is important that they be kept informed, for example, if their child has had difficulties with another student at school, hasn’t eaten while in a service’s care, or has had disturbed sleep during respite. This is about trust, but it also gives a family forewarning of an issue that, if it continues, might mean the child or young person will need additional support, such as more assistance around social skills or attendant care overnight. Respecting young people’s privacy Sometimes professionals must balance families’ need to be informed with a young person’s right to privacy and confidentiality, especially in late adolescence and early adulthood. Eventually many young people will need the skills and confidence to direct their own supports and to form adult relationships, including with their support workers. They need support to develop those skills, including from professionals. When they reach 18, most (unless they are under a guardianship order) are legally entitled to make their own decisions, and to have information about themselves kept confidential, including from family members, if they wish. Respecting young people’s privacy also helps professionals build trust and positive relationships. Most young people have the freedom to explore their identity, make mistakes, have relationships and do ‘teenage’ things. Just because a young person needs assistance from a support worker to go out, for example, does not mean they should not have the same freedom as their peers. There are also times when most young people want to talk to someone who is not their parent or caregiver: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 42 It’s good to be able to talk to a carer about anything, within reason. If I’ve had an issue with depression, and for some reason I can’t talk to my family, I talk to my carer. Some of them are good at understanding that they have to keep that private between us, and some not so good. If you’re going to put your trust in someone and tell them something private, they need to keep it private unless it’s an extreme matter, in which case they need to tell my mum. – Anthea What information is confidential and private and what may be shared with family members depends very much on the young person’s age and capacity. The context, including the professional’s role and relationship with the child or young person and family, is also important. Professionals need to be clear about their legal and ethical responsibilities and seek support from their manager if an issue they are unsure about arises. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 43 6 Practices that support choice and participation: decision making and action Key messages Research shows that the family-centred practices that make most difference to children, young people and families are those that support them to make decisions and take action for themselves. Professionals must collaborate with children, young people and families to determine their goals for services and supports. They often need to explain what they can offer before a family can name their needs but should be aware of their power to shape expectations, especially early on. Family goals might include the child’s inclusion in a family activity, which can be ‘broken down’ into a series of short-term goals. Professionals can support people’s self-efficacy (‘the belief in one’s capabilities to organise and execute the courses of action required to manage prospective situations’ 85) by encouraging them to work towards small achievable goals, putting them in touch with other families, being emotionally responsive, and helping people reflect on their experiences of taking action. Professionals need to understand that families have a different capacity to act at different times, explain the rationale for families’ active involvement, and tailor their support for action to families’ needs and capacity. Most importantly, people are more likely to make decisions and take action if services respond positively when they do so; if not, they are less likely to take action in future. Children (even infants) and young people can have input into decision making; professionals need to support this, and draw on families’ knowledge of their children to learn about them and their preferences, and to include them in discussion. Great sensitivity is needed if the choices of a child or young person conflict with the preferences of their family. Depending on role, a professional might be able to assist directly, or refer young people and families to specialist services to help resolve conflict. If professionals are concerned about people’s choices, they need to consider a range of questions, including: their role and responsibility in the situation; the level of risk or possible harm to the child or young person; whether they have offered adequate information to ensure the family’s choice is informed; whether the family’s thinking might change with other support; whether they are simply feeling challenged by values different from their own; and whether their own opinion is sufficiently informed. Self-determination, inclusion and choice This aspect of family-centred practice arises from a commitment to self-determination and the dignity of choice: the idea that people with a disability are entitled to make decisions for themselves and their families, and to live the life they choose. The principle of self-determination underpins self-directed support, increasingly the basis for all Victorian disability services. This first aspect of supporting choice in the family-centred practice model (see page 25) means supporting people to make decisions and take action on their own and their children’s behalf. The second (see chapter 7) is about ensuring the choices available to people are meaningful and can meet their needs. Inclusion is vital because many people want the choice of accessing mainstream services. Indeed, disabilityspecific services will only ever be part of the picture for any child, young person or family, complementing the role of informal supports (family and community), universal and other specialist services. Yet there are barriers to inclusion in many areas. A big part of supporting decision making and action is partnering with children, young people and families to help break down barriers, wherever they might be. 86 Everyone has the right to self-determination, but family-centred practice also requires that professionals recognise and address the factors that affect some people’s power to make choices in their lives. These include homelessness, unemployment, educational disadvantage, poverty, isolation, lack of access to Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 44 essential services, chronic and mental illness, family violence and discrimination – including discrimination based on gender, ability, race, religion, sexual orientation, family structure or circumstances. Family-centred practice therefore requires an understanding of the social determinants of health, defined by the World Health Organization as ‘the conditions in which people are born, grow, live, work and age, including the health system [which] are shaped by the distribution of money, power and resources … [and] which are mostly responsible for health inequities’. 87 Self-determination has a particular meaning to Aboriginal families and communities, as recognised in the Victorian Children, Youth and Families Act 2005 and the Bringing them home report into the Stolen Generations. As VACCA says, these key documents discuss self-determination as: … the principle grounding a right for Indigenous people to exercise control over matters directly affecting their children, families and communities. The Indigenous perspective on self-determination provides for the development of control over these areas of social life through processes which may involve some form of autonomy or self-government.88 This understanding of self-determination informs the principle that Aboriginal people should always be offered the choice of receiving supports from ACCOs, and points to the role of partnership between mainstream and Aboriginal organisations and communities in building the capacity of all to provide culturally competent, appropriate, high-quality services and supports to Aboriginal children, young people and families.89 Supporting choice There are many choices to be made during families’ engagements with services. Depending on the context, this might relate to choosing: which program or activity they will participate in; which professional they will work with; what supports will be offered, when and where (for example, at home or in other settings); and what role there might be for family members. Family- and person-centred approaches ask professionals to ensure, as far as possible, that these decisions are in the hands of those most affected by their outcomes. Ask and offer Professionals need to ask what support is wanted and explain what they can offer. If they propose an approach or action without first clarifying what is wanted, they might end up doing things that are irrelevant or a low priority for the person or family. On the other hand, most people find it hard to articulate their needs without knowing the possibilities. Some families expressed frustration with professionals who felt they were being family centred by not offering supports unless they were requested: [The service] ran an art therapy group and I wanted Ella to be part of it. I waited for them to say, ‘Here’s the art therapy group, Ella’s going to be part of it, that’s the next step’. But I heard nothing. We had a meeting and I said, ‘What’s happening with the art therapy? It’s brilliant – speech, therapy, everything in one class.’ They said, ‘Oh no, we can’t offer it to you, you need to tell us it’s what you want’. They can’t tell us what they offer? You run this group but you aren’t going to tell me because you’re waiting for me to tell you that my child needs art therapy, and then you’ll say, ‘Oh, we have a group’? – Ingrid Families also find it very validating when professionals recognise their support needs without them ‘having to beg’, as Amy says (see page 31). Once a relationship is established, people might appreciate professionals who offer further supports out of a deep understanding of them and their context: I work with a family who always has a massive pile of washing – it doesn’t get folded, they don‘t have time, they just pull clothes from it. If the parents are there, the kids can have mum and dad time, so I’ll offer a hand with something like that, that’s not connected with the children. It’s about building a good rapport, taking initiative. – Disability support worker Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 45 Case management have been quite proactive. As our family got bigger, they identified we would need more support and changed us from one package to another. They initiated that; I didn’t have to. It’s about thinking ahead, and keeping on track with us as a family, what family changes are. – Paula Professionals should prioritise discussion of the family’s desired goals early on, but it might first be helpful for professionals to outline their general role, approach and programs (including entry criteria, if applicable) and the potential benefits of their approach or modality, perhaps giving some concrete examples of supports that others have found helpful. In so doing, however, professionals should bear in mind their power to shape people’s expectations, especially early in their journey or when they enter a new service or sector. Collaborative goal setting Two critical issues in decision making relate to who sets the goals for supports and services, and what information informs those goals. In some settings goals were once more likely to have been informed by normative assessments;90 a child with a given diagnosis was expected to reach a certain milestone or learning outcome (perhaps related to motor skills, language or social skills) and the ‘intervention’ would be designed to help achieve this. In recent years assessment practices have become more functionally based,91 which suggests it’s more effective to start with what the child or young person and their family wants. People might express their desired outcome as the child or young person gains or strengthens an ability – to sit up or move unaided, to be independent in toileting, to socialise with peers or to concentrate on an activity. Children, young people and families need to know that their goals and needs matter most, regardless of what they think the expectations of the service or organisation might be: I always tell teachers to ask families what is the most useful thing they can be doing with the student. Sometimes they are surprised about the answers. I remember sitting in SSGs myself as a parent, hearing how the school had been working with my daughter on her writing her name. I said, ‘Why are you doing that?’ and the teacher said, ‘Well, most parents want it’. Well, she might have been getting some useful fine motor skills from that, but with her disability, she just wasn’t likely to need to write her name that often, it just wasn’t the highest priority. Given that some children learn slowly, we’d better make sure that we’re teaching them skills that are useful to them and their families. As we always say, there’s no point in teaching a student to tie their shoelaces when the family has decided that velcro and slip-on shoes are a perfectly acceptable solution for them. – Sue, principal of a special education school Sometimes the family’s priority is for the child or young person to be able to take part in an activity that is important to the whole family. Through discussion this can be translated into actions that make sense to everyone, and so are more likely to be supported by activities outside the professional setting: I worked with a young boy who had a traumatic brain injury ... The family said, ‘We want him to be riding his bike at the summer holidays, that’s really important’. Rather than saying, ‘But we need to get him out of bed first’, the team helped the family break down those goals. They needed a fair bit of facilitation, but by the end the family was saying, ‘Well, he needs to sit on the bike, so let’s work on sitting’. He did end up riding a bike in the school holidays. It was a modified bike, and mostly he was on the back of mum or dad’s bike. It wasn’t quite what the family had originally intended. But rather than telling them that straightaway – because they were overwhelmed and didn’t see how it would all fit together – over time the family came to see how it would develop, and what the next step could be. – ECI professional Some people might hesitate to name certain issues or hopes because they fear they are trivial or unrealistic, because their child’s diagnosis was delivered without giving much cause for hope (see below), or because experience has taught them that it’s unlikely their needs will be met. Supporting people to plan, implement and review approaches that help achieve short-term, realistic goals will support progress towards outcomes that might at first seem unattainable, as in this example from an ECI professional: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 46 I work with a family whose little boy has a neurological disease. One doctor said to the mother, ‘Kids with this condition don’t do very well, so don’t expect very much from your child’. This poor mum, she was very young, and she was so down. When I met her initially and we set some goals, she said to me, ‘What’s the point? I’ve been told he’ll never do anything anyway.’ It took a couple of visits to hash out what she would like help with. I completed her review the other week. Every goal on it was ticked off. At the beginning I asked, ‘How do you think your son is going, what’s been happening in the last six months?’ Mum said, ‘Nothing. He’s not doing anything, nothing has changed.’ I said, ‘Well, let’s have a look. In gross motor skills, you said you’d like him to sit by himself.’ ‘Oh,’ she said, ‘he’s doing that’. And so on. She was like a different person. She said, ‘Look at what my child can do’. It was the reviewing of the plans, being able to pull out even tiny, short-term achievable things. Choice in the context of limited resources Family-centred practice means that choices – as far as possible – are in the hands of those most affected by them. Yet these will always be limited by the availability of resources. What does being family centred mean in this context? Some families recounted experiences where they felt their ability to even express needs was ‘constrained’ by professionals focused on what was likely to be funded (see Amy’s story on page 31). If someone expresses a need that seems to go beyond the professional’s role, the available resources, or relevant guidelines or criteria, professionals should not make ‘no’ their first or final answer. Depending on their role, this might be an opportunity to explore what the request means to the person or family, what difficulty it might help resolve and what benefit it might have for the person with a disability. These explorations might well reveal that the request does fit the role, guidelines or service criteria. For example, an issue that at first seems unrelated to the needs of the child with a disability might turn out to be very relevant when looked at in terms of the needs of the whole family: We wanted to get the car windows tinted because Jack hates bright light. He gets very upset when light is in his eyes in the car. He eventually recovers. However, it triggers Abel to scream, shout and kick. This becomes dangerous and distressing for all. Professionals have to look at situations in the context of the whole family. – Cass If a need still cannot be met with the available resources, families and young people appreciate professionals who make the effort to explore other options, whether by referring them to another disability service or working with them to find other ways (for example, through other sources of funding, informal supports and universal services) to meet the need: When I started I fought like blazes to get everything possible for every family. I still advocate for families, often. But there are only so many resources for the region, so part of our job is to say ‘no’ sometimes. I’ve never heard a not good reason for someone wanting more resources than their package size. You’ve got to acknowledge the concern, or the difficult situation people are in. You give a wider context on why [the answer is no] and suggest, ‘Let’s try other things’, say making an application to the Lions Club or Rotary Club. You do as much as you can do to find options, to get the job done. – Facilitator This is also an issue of communication with families (see page 41). Children and young people’s role in decision making Professionals need to draw on both family- and person-centred approaches in relation to issues of choice, and self-determination for young children, older children, adolescents and young adults with a disability and their families. Why and how professionals balance the two approaches (especially if they come into tension) goes to the heart of what family-centred practice offers in working with adolescents and young people in particular, and is explored in some depth in chapter 2, ‘Foundations’. As discussed, most children, as they mature, have an increasing interest in (and right to) autonomy in relation to their everyday life and future. Most (unless under guardianship order) will be entitled to make Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 47 choices for themselves at age 18. Like all young people, those with a disability need support to develop the skills and confidence they need to make good choices and advocate for themselves, which includes practice in communicating their preferences: I’m trying to encourage Michael to have a say, to help him understand that when he’s with a carer he’s not actually being ‘cared for’. The carer is there to support him to do what he needs to do, not the other way around. It’s not something being done to him, and if he isn’t comfortable he needs to say so. All children are told what to do by adults, but as he becomes a young man, Michael has to realise he has a say in these things. – Anita Supporting children and young people’s input Many parents and caregivers, like Anita, Paula (page 188) and Anthea’s mother (see below), work hard to ensure their child’s goals and ambitions inform their services and supports, and to help them develop the skills and confidence to advocate for themselves. They are often keen to ensure their child is present during discussions, and will also model to professionals what they expect from them in terms of consultation with their son or daughter. Professionals need to be responsive when this happens: Michael is 17, and on the whole I find that service providers don’t talk to him. They talk to me, and I turn to him and say, ‘What do you think about that?’ I’ve made a concerted effort as he has grown to give him more of a voice. There were some issues at school, and I said, ‘I’ll go and talk to the teacher about it’. And then I said, ‘Well, you go and talk to the teacher about it, and I’ll go with you’. We made an appointment, and the principal came in and said, ‘What are the issues, Anita?’ and I turned around and said, ‘What are the issues, Michael?’ So he told them in his own words. The principal was really good, and we worked through it all. – Anita If children and young people are not already present and included in discussions about them (such as planning sessions and SSG meetings), professionals might suggest to families that they could be. Direct communication with children and young people is also critical. If they are verbal or use communication devices, professionals should ask them about their preferences. If not, professionals should ascertain their preferences by getting to know them – their personality, strengths, likes, dislikes and unique ways of communicating – through sound, expression, eye direction, posture and gesture. When people recognise and respond to indications of their preferences, even very young children can be supported to have input. Families are skilled in understanding what their child thinks, feels and wants, and can help professionals to become more skilled in this way too. As Cathy says about her daughter Angela (page 29): She’s non-verbal, although she can make her point known very, very clearly. It’s amazing how much you learn through the art of communication with someone who’s non-verbal because it’s so much about what you look at, what you do, and the emotion that’s emitting. I would like more than anything to be able to say to Angela, ‘What would you like?’, and for her to be able to tell me. But she can’t do that. Even if it was something I had to say no to, I would love it. It fills me with conflict sometimes to be making decisions for her. But I know my child. Often parents and caregivers need to speak ‘for’ their non-verbal child. Professionals need to remember to acknowledge the great care many parents and caregivers take to distinguish between what they understand their child to be wanting or needing, and their own wishes for their child: Yes, I was Casey’s primary carer and yes, I felt like we came as a package deal. But over time I learnt that I might want one thing for Casey, but what would Casey want? Yes, family is core, but right at the centre of that is the child, who is actually the one who is the recipient of the service … Casey couldn’t speak, so she couldn’t answer questions. But even asking me, ‘What do you think Casey will need?’ rather than ‘What do you want for Casey?’ is different. – Donna Pull out Box - Personal perspective: Anthea Anthea (a young woman with a disability) appreciates the continuity that comes from employing her disability support workers herself, rather than using a service. ‘I like it if I have a rapport with them,’ she says. ‘It takes the Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 48 hassle out … [because] they get to know you, and how to do your transfers, or give you a shower, or take you to the loo. You don’t have to panic about teaching a new person how to do something every time.’ As Anthea approached adulthood, she and her mother began to ‘work more in tandem’ in managing her supports: ‘If I’m having a problem with a carer I’ll try to address it. Some are more accepting of me as their boss. But if they see me more as their friend, I’ve had to say to Mum, “Look, I’m not getting anywhere, can you help me out?”’ Anthea appreciates carers she can talk to ‘about anything, within reason’, including matters she might not want to discuss with her family. She needs to trust that the worker will respect her privacy. It’s also important that carers stay out of ‘family matters’, Anthea says. ‘One carer recently, when I used to say, “Oh Mum’s been annoying me for this reason”, she’d say, “Yeah, I’ve seen your mum do blah blah”. It’s like, I have a right to say that, and you can agree to a certain point, but don’t get your back up, don’t get too involved. It’s butting in, cos it’s not your family, it’s mine. And you need to respect that just cos you work with us, and you work within my house, we still deserve privacy’. When family-centred and person-centred practices come into tension Often the wishes and needs of a child or young person and family members will be in accord and professionals will find it fairly straightforward to combine family- and person-centred practices in their approach. However, most young people, sooner or later, will make a choice, take an action or express a preference that conflicts with the preferences of their family of origin. The main difference for those with a disability is their level of reliance on their families’ continued support. Another difference, of course, is that (depending on their ability) young people might also rely on service providers to enact many of their choices. It is important to respond respectfully to families’ views about how much say children and young people should have at different ages, perhaps depending on ability. These views are often the expression of deeply held values, perhaps connected to a family’s religion or culture. And yet, as they mature, young people do have the right to a say in decisions that affect them, even when their views conflict with those of their parents and caregivers. As Caitlin (page 19) says, ‘After all, it’s my life’. Caitlin also says that professionals should be mindful of everyone’s needs, and how each decision impacts on everyone involved. Professionals must address such issues with great sensitivity. Even with the best of intentions it is easy to say or convey something unintended, potentially undermining the family’s trust in the professional, organisation or sector: I said to [a young woman I was working with], ‘Is that what you think, or what your mum thinks?’ I said it in front of her family. It was a really damaging thing to say, and a big learning for me. The family was really, really hurt. I apologised, but they withdrew from the organisation, although other people [within the agency] have remained connected with them and built bridges. I had made a mistake, but they weren’t prepared to give us a second chance. So that young woman has no services now. – Service coordinator The reality of the service system is that the lives of many parents and caregivers will remain focused on their son or daughter with a disability long after they reach adulthood, and sometimes for the rest of their lives. These are deep, complex, usually reciprocal caring relationships (especially as caregivers themselves age), which professionals must acknowledge and support. Sometimes that will involve respectfully assisting parents and caregivers to see new possibilities and options for their son or daughter, especially as they grow to adulthood. Sometimes it will also be about showing them there are other people who care about their son or daughter’s best interests. One professional tells this story: We worked with a young woman who wanted her partner to move in with her. Her mother was very concerned. She wasn’t saying, ‘No, it’s not going to happen’, but she was concerned. The mother and the daughter were refusing to speak to each other. We were in a very difficult situation because we were wanting to support the young woman and her partner, and we had potentially the capacity to do so. But we also recognised that the mother–daughter relationship was very significant, and we really wanted to try and maintain it. And although she couldn’t see it at the time, we recognised that the relationship was also important to this young woman. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 49 [Our staff member] did an enormous amount of work with the couple themselves to ensure that both individuals were wanting this, and that one wasn’t perhaps coercing the other. She also did a lot of work with the mother about her concerns. There was a lot of exploring of what the concerns were, debunking some of the myths [around sexuality and people with a disability], a bit of education for everybody involved, and taking the mother’s concerns to the daughter – from an independent perspective, rather than within the mother–daughter relationship. It didn’t happen overnight, but the eventual outcome has been that the couple are now together, and the mother is much more comfortable. In many cases it won’t be appropriate for the professional to play this kind of mediation role: if this is not wanted by either party; if the professional does not have the necessary skills, or appropriate role or relationship; or if there is an actual or perceived conflict of interest. What role a professional might play in helping resolve conflict should be determined case by case, through discussion in supervision and with the family and the young person themselves. Secondary consultation can also be very useful. There are many services that can assist in various capacities (depending on the situation and wishes of those involved), including family counsellors, mediators and advocates. A coordinator of one youth advocacy service says it is most often a parent, social worker or other adult who makes the first call: We will say, ‘Thanks for identifying that’, but then it’s our job to develop the communication with the young person, to find out what they want. We do have contact with parents after that first call because they are often concerned and want to know how it’s all going. But we remind them we are not their advocates. We maintain privacy, and respect that young people don’t necessarily want their parents to know everything about them. This becomes very important. We have lots of cases where we have parents ringing up saying, ‘Johnny’s dad doesn’t want him to do this, can you please advocate for him to have his rights respected’. Then we talk to the dad, and the dad says, ‘Johnny’s mum blah blah blah’. That’s quite common, that we’re dealing with parents in conflict. We can’t side with any of the parents. That’s not going to help. We need to work out what the young person wants, and try to get to the bottom of it. – George Taleporos, Youth Disability Advocacy Service coordinator Supporting action This aspect of family-centred practice goes beyond issues of choice. It is also about children, young people and families taking action: to investigate options, research for themselves, act on their choices, meet their own needs, advocate for themselves and obtain the supports and services they require. Recent wide-ranging research indicates that the main way that family-centred practice contributes to improved outcomes for children, young people and families is by strengthening their self-efficacy.92 Selfefficacy is defined as ‘the belief in one’s capabilities to organise and execute the courses of action required to manage prospective situations’,93 which affects how a person thinks, behaves and feels. 94 As this ECI professional says: It’s not one of the tangible goals that we write on a plan, but one of our key goals is to get a family from that point of being overwhelmed – ‘I don’t know what to do’ – to coming to you and saying, ‘What do you think about this?’ I like it when a family has done research on a standing frame, a chair or whatever, and says, ‘What do you think about this?’ rather than, ‘Oh, what should I do?’ For me, that’s the transition from them being overwhelmed, and you needing to help them to get there, to them being empowered, where they say, ‘How can we, as a family, use you for what we want?’ People with a strong sense of self-efficacy regard challenging problems as tasks to be accomplished. They tend to develop a deeper interest in and commitment to the activities they take part in, and they recover quickly from disappointments. People with a weaker sense of self-efficacy tend to avoid challenging tasks, believe that difficult situations are beyond their capabilities, tend to focus on the negative, and quickly lose confidence in the face of setbacks.95 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 50 Albert Bandura, the psychologist and researcher who first described self-efficacy, lists four factors that affect people’s sense of self-efficacy that are useful pointers for family-centred practice: ‘Mastery’ experiences: performing a task successfully strengthens people’s sense of self-efficacy. Therefore, encouraging families to do work towards an achievable goal strengthens their confidence to do more. Social modelling: seeing that other people like themselves have completed a task successfully is a powerful motivator. Peer support is helpful for many families, as are stories (for example, in the services’ communication materials) about what other families have achieved. In the same way, examples of good practice (such as those in this guide) are a way to support professionals to improve their own practice. Social modelling is also an important way that parents and caregivers show their children the importance of taking an active role in meeting their own needs and advocating for themselves. Psychological responses: everyone has their own set of emotional responses to life’s challenges. Stress and anxiety, for example, can affect a person’s self-efficacy in a difficult situation, but the key factor is how people interpret their emotional responses. Most people can learn how to manage their stress and so improve their sense of self-efficacy.96 Social persuasion: Bandura says that people can be verbally encouraged to believe they have the skills and capabilities to succeed; however, encouragement alone is not enough to strengthen self-efficacy, especially in the face of challenges. Indeed, he says it’s easier to (unintentionally) undermine people’s self-belief, with the consequence of undermining self-efficacy. Reflection, not praise Some researchers suggest that objective reflection, rather than positive encouragement or ‘praise’, might be a more effective way to help support stronger self-efficacy.97 However well intentioned, praise can feel like a judgement from ‘on high’. Praise is also less likely to create space for the person to discuss their ambivalences or difficulties, or reflect on how they might do things differently next time. Simply acknowledging the efforts of a parent or caregiver, for example, gives them the space to talk about what the effort has cost, any doubts they might have about the value of that particular effort, or any ambivalence about similar future efforts. Tailoring support for action Most parents and carers of children and young people with a disability feel they are their children’s best advocates – and that they have had to be. Many take on this role with gusto (see Daniela’s story, page 39), others less so. Most professionals have experiences of working with people who want them to make the decisions, implement the therapy (or educational strategy, case plan and so on) and ‘just fix it’. This doesn’t mean these families care or know less about what will work for their child and family, nor does it mean they have less potential to take a more active role. It does mean they are less likely to articulate their knowledge, and might require far more support and encouragement to become informed, set goals, and make decisions and act on them, for instance by partnering with professionals to implement supports (say in relation to early intervention) in ‘natural environments’ such as the family’s home. Like most people, parents and caregivers of children or young people with a disability will have varying capacity to act at different times. Most parents and caregivers also juggle paid work, the needs of siblings and other issues. Many find their capacity to take an active role increases as they journey through the system and adapt to the changes brought about by their child’s disability: In the beginning I felt that the case manager was coming in and managing me. I wasn’t capable of doing anything else. I’m a much different person this many years on. The case manager still manages our case, but I feel that I can advocate for our family much better than I could back then. I have a good understanding of the system. – Amy Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 51 When professionals are struggling to engage a family in making decisions or becoming involved in an activity to support their child’s development, it might be helpful to consider whether: the supports or activities in question have been designed collaboratively in relation to the family’s goals and priorities, daily life and long-term capacity the professional is offering sufficient support for the parent or caregiver to take an active role, for example, by offering the chance for them to practise doing a task with the child or young person when the professional is present, to build confidence, give reassurance and adjust technique the professional can work with other services involved in the child or young person’s situation (for example, in relation to their therapeutic activities in the home) to tailor their supports to family capacity, therefore developing an integrated support plan the rationale for the family’s participation has been clearly communicated the family is unable to engage due to unavoidable circumstances, or if they might be able to do so with more or different support; for example, parents and caregivers might be eligible for more financial assistance or help with other responsibilities, allowing them more time for their family, or some might benefit from referrals to meet other needs, including their own, those of their child with a disability or other siblings it would be helpful to invite (with the parents or caregivers’ permission) other family members or people in their informal network into the process. Social support for families is a key factor in children and young people’s long-term outcomes,98 and creative planning processes, for example, can help some families to identify that there are many more informal supports available to them than they realised: I feel privileged to be part of a Circle of Support for a young boy who was previously in our service … At the first meeting there were 25 people [all] considering how they could have a role in supporting this family and child. A number of their friends had wanted to help but didn’t really know quite what to do. Having the Circle of Support validated their role. – Service manager ‘Releasing’ people’s capacity to take action British health researcher Jennie Popay says many professionals assume people do not engage because they lack skills and capacity. She suggests most people will act on issues that matter to them if they believe action is likely to be effective. But if their experience is that their views or experiences were ignored in the past, or that ultimate control of resources lies with professionals, then they will be reluctant to engage again. She suggests that rather than trying to ‘build’ people’s capacity to engage, professionals should ‘release’ their inbuilt capacity by addressing issues that lead to reluctance, 99 for example, by ensuring decisions are in the hands of service users and that their knowledge and preferences do meaningfully inform planning and other processes. Professionals need to tell families that it’s important to be involved to ensure supports and services are tailored to them, and to address any other needs that might prevent their engagement. This includes making sure they receive a positive, respectful response when they do engage. In the end, a family or young person’s level of involvement is up to them. Of course, some parents, caregivers and young people with a disability go beyond advocacy for themselves and become powerful advocates for others and for broader positive change. Professionals can encourage service users to get more involved in their organisation, let them know about advisory groups or consultations that will give them an opportunity to contribute to service system development, or put them in touch with community-based advocacy groups and associations. Many of these provide both support and advocacy for families, and an opportunity for families to become involved in broader change: The Association for Children with a Disability provides support and information, individual advocacy, community education and public policy responses to improve the availability and delivery of disabilityrelated services. ACD helps families build confidence to navigate complex support systems and provides Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 52 tools to successfully mediate with service providers to achieve better outcomes for their children. – Elizabeth McGarry, Chief Executive Officer, Association for Children with a Disability When families are dissatisfied with the service’s approach Sometimes the approaches services take don’t at the outset meet families’ expectations, especially in terms of one-on-one therapeutic activities. All services benefit from feedback, reflection and improvement, but sometimes families feel very dissatisfied with services that require them, as a fundamental part of their approach, to take an active role. When this happens, this ECI service manager says: We try to meet them halfway, if that’s what we need to do for a short period to engage the family. If it means having a small win. So if they want one-on-one physio for a while, we could start that process, but we would always be working towards giving the power back to the parent. There are definitely families that want more of a passive role. It’s about keeping that conversation going. The issue is, a child can come in for an hour’s session, but that’s just two per cent of the child’s time for the week. What’s really going to be effective is if we spend the time teaching the parent activities that they can incorporate into their daily routine – that will have a far greater effect than the one hour of dedicated time with a therapist. There are families where we have to start that way, especially if they’ve been transitioned from other services like hospital-based therapy services, or they have been seeing private therapists. So there is a transition between the two models. Sometimes, people will remain dissatisfied with the level or type of support a particular organisation or service provider offers. Professionals need to do everything they can to address such concerns. They need to ensure: families receive all the supports they are entitled to within and outside the service families’ and other service users’ suggestions and feedback are sought and acted on families and young people are informed about complaints and grievance procedures, and supported to use them if necessary. In the end, if the family is still unhappy, the professional should offer to help them find alternative sources of support and offer assistance to transition out of their service (see Ingrid’s story, page 41). Pull out Box - Personal perspective: Winnie Anecdotally there is a perception among service providers that CALD families are less likely to engage actively or to advocate for their child with a disability. If this is so, reasons might include families’ perceptions of their role or the role of services, or inadequate skills in cultural competence among professionals. As Jennie Popay says (see above), people’s experiences when they do take action can also have a major impact. Consultations for these guides included group interviews with several support groups for CALD communities. Winnie, a member of a group for parents from a North Asian community, was a strong advocate for her son at secondary school, having had ‘regular meetings and an individual plan’ when he was in primary school. However, she says secondary school staff ‘don’t meet with me unless I request it. I went to a meeting and told [the school] strategies for what to do with my son, but they didn’t do any of them. I gave them the contact details of Autism Victoria and the number of an autism school who will do outreach and will give some advice to mainstream schools, but the school never spoke with them.’ Winnie’s son’s five hours of classroom support per week haven’t helped him. The aide ‘sits near him’, she says. ‘My son doesn’t like it. He won’t ask her for help. When she tries to help he ignores her. He tells me he is annoyed by this lady … “She follows me all the time,” he says. The teacher’s aide says that if she is sitting in the classroom, he sits on the other side of the room. I said to the school, “Maybe you could use the funding to help him in another way?” They didn’t … [Also], my son is 20 minutes late for every class. When the bell rings, everyone goes to their locker. It is very crowded. My son doesn’t like this. He waits until everyone has gone to class before he will go to his locker. I asked the integration aide to come up with a strategy for this, but she hasn’t.’ Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 53 If you are concerned about people’s choices Some situations require professionals to act (whether or not they are mandated) in the best interests of the child. Professionals should consider making a report to Child Protection where a child or young person is in need of protection and has or is likely to suffer significant harm due to emotional abuse or neglect and the parents have not or are unlikely to protect the child. A referral to Child FIRST may be the best way of connecting families to the services they need when they are experiencing difficulties that make them more vulnerable and impacts on the child’s safety, stability and development.100 See the Child, Youth and Families website for more information about making a report to Child Protection or a referral to Child FIRST.101 In some situations professionals will be working with families whose choices strongly concern them but which might not warrant a report to Child Protection or referral to Child FIRST. In such cases professionals should consider (with support from their supervisor) their role and responsibility to the child or young person and family and whether: the family’s decision or action poses a high level of risk and possible harm to the child or young person – to be decided on a case-by-case basis with the professional consulting their supervisor and with social workers or others in their team, and with Child FIRST (they are not obliged to make a referral) they have gathered enough information from the child, young person and family, as well as from other services, to have a sufficiently informed opinion the professional is simply feeling challenged by values and choices that are different from those they might make themselves in the same situation the course of action the professional wishes to suggest is sufficiently informed by the family’s priorities, and able to be implemented in a way that fits into family life the professional has provided enough appropriate, accessible information to the family or young person to ensure their decision is well informed the family’s thinking might change with additional support, such as a second opinion, advocacy support or counselling; for example, some families have had negative experiences of medical care for their child with a disability and might be very reluctant to consent to further treatment, even if this decision has significant consequences for their child’s long-term health and development. Professionals’ duty of care obliges them to talk to families about any practices or choices (or aspects of a child’s environment) that have the potential to cause harm.102 Sometimes a concern will arise because of inaction, for example, if parents or caregivers are not carrying out basic care procedures (such as putting on ankle-foot orthoses), resulting in risks to the child’s long-term health or development. As discussed, the appropriate response is determined by the risk and level of potential harm. If this is serious, long-term or irreversible, a report to Child Protection is warranted. The reality is that many families are dealing with multiple stressors, including homelessness, unemployment, poverty, mental ill-health, chronic illness and family violence, and will not always be able to prioritise their child’s needs. In making decisions about the best interests of the child or young person consideration must be given to the cumulative patterns of harm on a child’s safety, stability and development. For example, one ECI professional described a family in which both parents experienced mental illness: The biggest issue from my perspective at the moment is that the child is not sleeping. So they can’t make appointments, they can’t turn up to playgroup, they can’t handle anything because they’re not getting any sleep through the night … but when it comes to taking any action to deal with that, they aren’t ready to. Either it’s not as big an issue for them as it seems to me, or they’re currently not in a position to take action, probably because they haven’t slept for a long time, and there are a lot of other things going on. Professionals need to refer families to other supports and services as required and tailor their own support to the family’s needs and capacity. In many such cases (as in this family), there are multiple service providers Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 54 involved. The professional needs to ensure good communication and coordination with the other services, as well as appropriate monitoring of any factors that might develop into risks for the child or young person. Sometimes professionals will work with families who are engaged in dubious ‘treatments’ for their child’s disability. These can be very expensive, time consuming and give people false hope for a ‘cure’, for example, for Down syndrome or cerebral palsy. Often the harm is limited to the family’s finances and emotions when the ‘cure’ proves ineffective; sometimes there are associated health risks. Professionals should consider the issues listed above, in particular the level of risk or potential harm of the practice. If there seems to be little or no risk, professionals might simply ask questions about the family’s experience of the efficacy of the approach and offer information about the credible evidence for or against it, taking care not to make families feel judged for their choices. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 55 7 Practices that support choice and participation: flexible, responsive services and supports Key messages Services can tailor service delivery to family life by offering appointments to fit family routines, delivering support in the home or other accessible locations, providing flexible service hours or offering support through telephone, Skype or SMS text messaging. They can reduce the demands on families by offering support with administration, ensuring continuity of care, and sharing information (with permission) with other services. Professionals should be aware of the demands they put on families, and work with the family and their other services to formulate an integrated support plan matched to their needs and capacity. Services and supports should be tailored to a family’s needs, goals and priorities. Professionals can do this through collaborative goal setting, seeking out and reading all relevant information, and responding to the many ways in which families differ, including in its make-up, attitudes to disability and care, understanding of development and child rearing, and attitudes to gender and privacy. Professionals should integrate supports into children and young people’s natural environments. Families are generally best placed to implement many activities in the context – and at the frequency – needed for them to be effective. Other natural environments include kindergartens, childcare centres, schools and recreation facilities. Many families want their children in mainstream services; sometimes professionals need to support those services to meet children’s needs, or support families to advocate for inclusion. Parents and caregivers themselves need support, including perhaps respite or referrals for various needs. Professionals should support siblings of children with a disability, for example, by integrating them into activities, or referring them to siblings groups or family activities. Professionals can validate siblings’ roles by encouraging their participation in helping their brother or sister with a disability. Professionals need to respond to developmental changes and changes in family circumstances. Most families find transition between different settings or sectors stressful; professionals can assist by sharing information (with permission) and engaging in collaborative planning with the family and other services. Professionals need to ensure children and young people with a disability and their families can choose from options that are appropriate and relevant to their needs. This requires both flexibility and responsiveness. Flexibility is about professionals being willing and able to tailor services and supports to people’s needs and preferences. Responsiveness is about being alert and responsive when these shift. The ability of professionals to be flexible and responsive will depend to an extent on their role and their organisation’s capacity. Some professionals are quite autonomous in managing their time and deciding how to carry out their role. Some are more restricted, whether by their role or level of authority, their job description or conditions, or the pressures of time, resources or funding. The reality for most is somewhere in between. Chapter 9 and the organisational guide discuss ways that managers and organisations can support staff to be family centred, including through more family-centred policies and processes. Fitting in with family life Unless young people with a disability live independently, their lives are shaped by their family members’ various needs, schedules and priorities. Depending on context, services might be able to tailor various aspects of service delivery to fit in with family life, including those below. Family schedules and routines Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 56 Many services make efforts to schedule meeting, appointment and respite times that fit in with family routines, rather than simply advising families of when the service will be delivered. Families also appreciate flexibility in when supports are delivered: We can utilise our respite how we choose. So I could have someone here every day at school time so I can pick up the kids from school, and have Emily here. Or I can put it in a block, so Emily can stay here on a Sunday and the rest of us can go out bike riding or something. – Amy When we go out as a family, one of us invariably ends up looking after Angela while the other parent participates in the activities, then we try to swap. It would be great if we could ring and say, ‘Are you available for four hours? Meet us here.’ So there are an extra pair of hands to help Angela participate, or to just spend a bit of time with her, rather than her being in respite or being left at home. – Cathy Some families have regular routines and appreciate professionals who try to fit in with them. Some families are much less likely to have regular routines, and professionals need to stay in touch, and be flexible: I always tell workers to ring families. You could say, ‘When’s a good day? Okay, I’ll come next Tuesday, let’s put it on the calendar. Ring me if you need to change it.’ But nine times out of ten they don’t, so you ring the day before and say, ‘I’m calling in to see you tomorrow. Are you right to have a yarn and a catchup? Is there anything you need? Is there anything you’ve got in the last week that you need help with?’ Workers also need to give families that courtesy, to let them know if they can’t come themselves. – Jody Saxton-Barney, Victorian Aboriginal Disability Network Childcare needs Sometimes it will be appropriate for the professional to meet with parents or caregivers without their child. In such cases families might appreciate assistance with childcare, or the flexibility of meeting when others are caring for their child (for example, during school hours). If a family has more than one child it can be very difficult for them to access many services and supports, especially if they don’t have informal supports to care for the other children, such as grandmothers or other relatives, or financial resources to pay for childcare. Families appreciate services that cater for the needs of siblings, whether by scheduling groups and appointments to avoid school drop-off or pick-up times, providing childcare for siblings, providing support tailored to their needs (see Melissa’s story, page 34), or including them in activities: When Samuel was in early intervention, they would have stuff there for the younger kids to do, or they’d encourage them to be part of the exercise. They almost built them into the program. Most of us would be looking for opportunities for the other kids not to be there, so you could just concentrate on one. But all my kids got dragged from pillar to post, especially my oldest. So you’d be looking for services that would accommodate their needs. – Paula Transport Difficulties with getting to services can be a major barrier to some families accessing support. Services can provide support for transport (such as taxis), or offer to deliver supports in the family home or at childcare, kindergarten, school or other community settings. When meetings are required with a parent or caregiver who is in paid work, the professional might offer to meet them at a cafe near the parent’s workplace. Sometimes transport difficulties are such that it might be appropriate to offer support to parents or caregivers via telephone or even Skype such as the families of the many children and young people who travel great distances to access special education settings. It can be very difficult for some parents to attend regular face-to-face SSG meetings (including arranging childcare) within working hours. Phone or Skype meetings might be more appropriate for ‘check-ins’ than for key planning meetings. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 57 Service hours Flexibility in service hours might make it easier for families to attend a service and help engage different members of the family such as parents in full-time paid employment. Sometimes flexibility in service hours will suit staff, but it is also important that this doesn’t undermine their conditions of employment. Communication preferences The way people communicate is changing rapidly. Many people are comfortable using Skype (see above), while a lot of young people use SMS text messaging and email as common forms of communication. Using these tools has the potential to enhance service without significantly increasing service time, although it is important for services to be aware of any implications for staff working conditions: Family-centred practice is about making time for relationships. One thing that’s changed in our service in recent years is how we do that. These days there’s probably an hour and a half per week of funded family intervention. But we now have quite a few families who, in addition to our contact hours, have fairly regular SMS contact. That’s given an opportunity for some people to have better relationships because they’ve got more frequent contact. There’s a whole age group of parents for whom that’s a more natural way of relating [although] we have to be mindful of boundaries. – Service manager Pull out Box - Personal perspective: Kate, Greg, Jamie, Melanie and Callum Kate and Greg’s oldest child, Jamie, has a pervasive developmental disorder, and their younger two, Melanie and Callum, both have Asperger’s syndrome. The family has had to juggle the expectations of many service providers over the years. Kate says: ‘You might have an ECI staff member, you’ve got the kinder teacher, you’ve got the kinder aide, you’ve got the paediatrician. If you’ve got any medical issues you’ve also got all those people … You get workers who talk as if they know everything, telling me what I should be prioritising. I’m thinking, I’ve got five specialists… It’s like they can see one entrance, but not the whole house. In the early days they would leave and I’d just feel terrible about myself. I’d think, I’m not doing that, but maybe if I was, Jamie would get better. ‘They just kept giving me tasks to do or therapies to run, and failing to acknowledge that I needed to look after myself, because in the long run I still need to be able to function. I’ve felt workers push and push to implement strategy after strategy; they didn’t see that, as a mum, I have to still be doing it in 12 months, two years, five years, 10 years. Now I often say to service providers, “I just need to work on one thing per child at a time. That’s all I can do”. The ones who accept that have been good. Sometimes I feel they’re just focused on the child. Some don’t see where I’m at, and my capacity, and that’s been hard.’ Service levels Sometimes the more intensive forms of support a service offers (such as groups or appointments) will not suit a family’s needs. An alternative might be to offer the family less intensive – but still proactive – support, while leaving the door open to more intensive engagement if the need arises: [One mother I work with] has four children, two with autism. Their days are so busy with so many different things that [the group-based supports offered] didn’t work for her. We talked about the different options, and in the end worked out that the best thing was for me to ring her once or twice a term. That’s what she needed from our service, just to talk through any issues, and if anything was coming up that we could help her with, then we would. She would basically use us as a sounding board. – ECI professional Reducing the demands on families For some families, managing their child’s services and supports (as well as their care) can amount to an almost full-time role. It can make a significant difference to families when professionals are aware of the demands placed on families by their service and the other services the family uses, and do what they can to reduce those demands. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 58 Offering support with administration Some people prefer to manage their own supports. Some do not, or don’t have the capacity. Families appreciate being offered options for assistance on this level. Professionals should take care to explain the implications of increased administrative or case management support for respite or attendant care hours, such as within a funding package. Maximising continuity of care Always seeing the same one or two professionals reduces the need for people to repeat information. More importantly, it supports the formation of positive, effective partnerships. Continuity of care is a particularly crucial issue for some: [Therapists] need to get to know your child. And the reverse – the child [needs to] get to know and trust the therapist, which is extremely important. Transition is really important for Angela. First she needs to see the place [where the therapy will be], then come back another day. Then she can walk into the room, check out the bed she has to lie on, talk to the therapist, then go away. It will take quite a while for her to be comfortable to have someone touch her. It took until last year for her to walk in quietly without having a complete meltdown, and me having to physically restrain her. It’s a really big problem when we don’t have that continuity of care. – Cathy Sharing information There are many ways in which services can improve how they collect and manage the information of those they work with (see chapter 9 and the organisational guide). Professionals should make detailed notes so that families and young people with a disability don’t have to repeat information. They could offer to fill out forms (such as funding applications) with families or young people, or transfer previously collected information onto new forms. Often it will be helpful for professionals to share information within their team or with other services (with permission). You’ve got to tell your story again and again, even with the same agency. People won’t read in a file about your situation. They cite things like privacy and confidentiality. We want that, but often it’s used as a barrier to sharing information. There’s no legal reason why they couldn’t share that information if you give your permission. – Paula Following up and paying attention to detail Lack of follow-through by busy professionals is a common complaint from families, as are basic problems such as lateness or inattention to detail. When a family relies on service providers to get through their day, a seemingly small mistake by a service provider can have significant implications: For instance, a big box of continence aids arrives, you open the box and it’s the wrong sort. You haven’t got more, you haven’t got money to go and buy any … The knock-on effect from that is you can’t take the child out. And you have to find the energy to try to get another box, and get rid of this huge box you don’t need. – Association for Children with a Disability family support worker Improving service integration Professionals need to improve both communication and coordination with the other services involved in the lives of children and young people with a disability and their families to ensure the family is at the centre of the whole range of their services and supports (see page 71 on teamwork and service integration). Tailoring services and supports Flexibility is not only about reducing the burden on families that are often already overstretched, although this is important. It is also about maximising the effectiveness of services and supports. The evidence shows that Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 59 parents and caregivers are much less likely to participate in early intervention, for example, if its design or delivery is inconsistent with their goals, priorities or routines. 103 Engaging children, young people and families in goal setting and planning can greatly enhance the effectiveness of supports, as in Donna’s experience of her daughter Casey’s special development school (see box). Professionals need to work with children, young people and families to design, implement and review supports and services. This is about everyone contributing their knowledge, expertise and resources, and working together to determine and make use of the best mix of informal, disability-specific and universal supports and services to meet people’s needs. This will mean different things in different contexts, as explored in the sector-specific guides that form part of this suite. Key elements common to many settings are explored below. Pull out Box - Personal perspective: Donna, Ben, Casey and family ‘The greatest source of support, without question’ for Casey and her family (in terms of service providers) during the 10 years of her life was her special development school. But although Casey had complex medical needs and a severe intellectual disability, she and her family also had a very positive experience of a universal service, in the form of family day care. ‘It’s funny,’ says Casey’s mother, Donna. ‘I never think of it as a support service because [Casey’s older brother] Ben also went to family day care. [But] my family day carer took on an awful lot, and the council provided her with a lot of support so she could look after Casey.’ Some of the many positives about Casey’s school were that Donna knew her daughter was safe at school and that the school partnered with Donna to maximise Casey’s participation in learning. ‘They brought expertise to the table in education, and I brought my expertise to the table in terms of being Casey’s mum,’ Donna says. ‘Our goals were for her to become more independent in small ways.’ ‘They got to know Casey as a person, and through knowing her personality, they knew when to push her and when to back off. They knew who was who in the family. They knew the right questions to ask [me], so they could talk about those things with Casey. They knew about what the family did and what Casey liked to do at home. Casey adored watching her brother play basketball – they knew about that and talked with Casey about it at school. They knew that my mother, her grandmother, was also very important to Casey.’ Taking a lead from families Professionals need to take their lead from children and young people with a disability and their families in the planning, design and implementation of services and supports. This means finding out how things are done in that family and tailoring supports accordingly. How a family does things is often an expression of their values and priorities. This can impact on many aspects of their supports and services, from their long-term goals to: … tiny things, like should Emily have her teeth brushed and face washed when she first wakes up, or once she’s in her chair and has woken up a bit? We have our own way, and I think I’d hate to be woken up with a freezing cold face washer! – Amy The easiest way to find out more from a child, young person or family about how things work best for them is to ask. However, families also appreciate professionals who make the effort to read all the available information about their family, who can observe their needs, and who record information and share it with others in their team who might be involved in delivering support. Professionals need to gather (with permission) and read all information available about the child or young person and their family, including case files, communication books and reports from other service providers. Common areas of difference Families are diverse in many ways, but there are some common issues arising from such differences that impact on design and delivery of services and supports: Who is part of the family and how are relationships defined? This might impact on who is included in planning, decision making and communication, and who takes an active role in implementing supports. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 60 Who makes which decisions, and what is the division of labour in the family and household? With this in mind, who needs to be included in decision making and implementation of services and supports? How does the family manage everyday life, including meals, transport, leisure and cultural or religious observances and celebrations? This might impact on the nature and timing of supports and when appointments should be scheduled (for example, not during times or days of religious observance). Attitudes to disability, including who is responsible for caring for people with a disability: these might impact on the way people understand disability (what it is and how it comes about), which might then influence the kinds of services and supports they are interested in, including whether they are open to respite or other support services. Attitudes to authority and self-advocacy: these might impact on how willing people are to actively ask for services or advocate for themselves, with implications for how professionals themselves interact with people and seek their views, as well as for how they might support people to advocate for themselves. Understandings of development, knowledge, abilities and social roles at different ages: these might impact, for example, on what abilities children might be expected to develop at different ages. As mentioned, when working with a family from a culture where children are routinely hand-fed until age five, it would make no sense to include this as an assessment criteria or goal for a younger child. Attitudes to gender roles, relationships and separation of the sexes in different spaces: these might impact on the gender of the support provider or the nature of the supports and services suggested. For example, many cultures require separation of the sexes after a certain age, making single-sex groups, activities and facilities much more appropriate than mixed-sex. Which matters can be discussed openly, and which are private: this might impact on when, how and in whose company professionals raise ‘sensitive’ issues with children, young people and family members. The level of comfort with people other than family being in the home or involved in personal care. Interpersonal communication style, including attitudes to touch, personal space, expressing disagreement, eye contact or pauses: these would impact on what non-verbal signals a professional should be cued into (including unwillingness to verbally express disagreement or discomfort) and how they might ensure the appropriateness of their own body language. Professionals also need to respect and respond to the cultural needs of children and young people with a disability, as they are central to their identity and sense of self. This might be especially important for those children whose medical needs or disability have restricted their access to cultural knowledge or events: Of course there is a need to provide the child with a wheelchair or speech therapy or OT, but cultural needs are just as important to a child’s wellbeing. Is the child able to attend festivals? What can be done to help them engage with other children from their cultural background when they are in a special school? – Jody Saxton-Barney, Victorian Aboriginal Disability Network Using natural learning approaches It is now common practice within ECI and allied health practice to integrate supports into children and young people’s natural environments, including their care, play, household or family activities, schooling and recreation. Strategies embedded in family activities include: ways of carrying children that build their strength; word and clapping games that support speech and social skills; climbing activities in the backyard or park that help with balance and gross motor skills; and toys or household tasks that help with fine motor skills: We are working with a young mother with two boys who have autism. One thing she told us would really make a difference was if she could enjoy playing with her sons. That’s been our focus. Last week we spoke on the phone, and I could hear her boys laughing, which I’d never heard. She herself was clearly happy. Her life had changed. That was just a very simple program of 10-minute fun activities our speech Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 61 pathologist had worked out. They were making this huge difference to her. But it needed us to affirm that having fun with her children is a good thing to focus on. – ECI service manager Some activities will be most effectively performed by professionals, perhaps due to the skills required or because children and young people respond differently to someone who isn’t their parent or caregiver: Parents know our children best, we advocate for our children, we talk to them every day. I do reading and words with Ella. But four months ago we started with a new speech therapist. She sits with this child for half an hour, and they get more done than I could do in a month. I can’t teach her on my own, I don’t have the skills. Plus, she’s my child and she knows it! Whereas if a therapist sits with her for an hour she behaves very differently – as kids do for someone who is not their parent. – Ingrid Yet as described by the ECI service manager on page 53, most professionals are likely to be with a child or young person for only an hour a week or fortnight. Parents and caregivers are children’s first and best teachers, and are generally best placed to implement many activities in the context – and at the frequency – needed for them to be effective. Professionals need to clearly explain the rationale and evidence for family involvement in therapeutic activities. If the design of supports starts with activities the child, young person or family already do or are interested in doing, or the goals they want to achieve, they are more likely to do the activity regularly, making the goal more achievable. Identifying appropriate locations and services, supporting inclusion Often the most appropriate natural learning environment is the home, but other environments might be kindergartens, childcare centres, schools, sports clubs, recreation facilities, libraries and community centres. Sometimes being in other environments can result in extremely fruitful partnerships and excellent supports for the child or young person with a disability, their family and the mainstream service provider (see Deborah’s story, page 72). In some cases, work might be needed to build and continuously support the capacity of staff in these settings. A professional’s capacity to do that will depend on factors like their role, their organisation’s policies, time, resources and the willingness and capacity of staff involved. The suggestion that staff might help facilitate natural learning should be discussed with the child or young person and the family. In school settings, while educators and integration aides are not expected to be therapists, there might be activities important to a student’s development that can be incorporated into their learning, in both mainstream and specialist settings: [We collect] information about how we can support the family in their home if there are sensory issues or issues with sleeping. We could look at doing a sensory profile with the OT; look at what the parents could do and how we could help at school. A number of children come in with very limited diets, so junior primary teachers have been growing vegies with the children, and doing a cooking program, which has encouraged some children to try different foods ... I sometimes find parents are at their wits’ end – we can develop behaviour management techniques in the classroom that parents can do at home. – Special development school teacher Sometimes strategies might be specific to the child or young person with a disability, such as using a special chair or desk. However, it is also important to promote inclusion by incorporating supports for students with disabilities into the whole environment.104 For example: a physiotherapist might develop activities that can be used in a physical education class; a speech pathologist might offer word ‘games’ that can be used in class; or a kindergarten could create a ‘quiet time area’ or sensory activities for use by all children. Many families want their children to be integrated into mainstream environments, educational and otherwise. Indeed, disability-specific services will always need to complement the support provided by informal networks and universal services. Sometimes mainstream services will need support to meet the needs of children and young people with a disability (see Deborah’s story, page 72); sometimes advocacy will be needed to bring them on board (see Alison’s and Paula’s stories, pages 144 and 188). This is about people’s right to inclusion. It is also about valuing the diverse and unique contributions that Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 62 people with a disability make to the community when their meaningful participation is supported: I bumped into [a mum from Michelle’s class] a couple of months ago and we were chatting. She said to me, ‘When Michelle started at the school, I didn’t know what was going to happen. I knew nothing about disability and I was kind of scared of her. But by the end of the year I realised she was just like any other kid.’ And I thought, Good on you Michelle, you’ve taught someone something! That shows why integration is so important. The fact that this mother could admit it, that was great. She was open and positive, and learned from the experience. That’s why we need support, so kids growing up can realise that kids with disabilities are part of the diversity of life. – Melissa Supporting parents and caregivers Families very much appreciate professionals who show an understanding of the multiple pressures on families and the needs of other family members. Many parents and caregivers find the various stressors associated with caring for a child with disability (especially with inadequate support) can put a considerable strain on their relationship, with negative consequences for their own emotional wellbeing, and for their children: For the first two years we were crying all the time. We didn’t go out. We were so isolated. My husband and I were fighting and not sleeping together. On the inside he was blaming me for the disability. We didn’t know anything about the disability or services that could help us. The first service to see people in these situations needs to give knowledge about the disability and what we can expect in the future. We had no idea. – Miriam, member of a support group from a Middle Eastern community Professionals always need to offer families information about their support options. This is especially so for families from marginalised communities. Professionals also need to help parents and caregivers understand how to navigate the service system, for example, by providing information about services and government departments and assisting in meeting requirements like filling out forms. Often families will have a letter from the hospital, or school, or Centrelink, and they’ll ask, ‘What does it mean? Why does he have to go and have grommets? Who gets this information? Why do I have to sign it? Where does this go?’ That fear factor – it’s ingrained in us, unfortunately. ‘Who needs to know all this stuff? Why?’ I try to get them to understand that … it’s the same form for everybody, [and] whilst paperwork is hard to fill out, it’s confronting, but it’s necessary to get the funds to do the work. – Jody Saxton-Barney, Victorian Aboriginal Disability Network Many families have nobody in their networks who can care for their children to give family members a break. Some families go for years giving around-the-clock care. Respite can provide welcome relief for many, and give parents time to reconnect, especially when one parent has been providing more of the day-to-day care: I have respite from the council once a fortnight, so my husband and I can spend time together. You can become quite resentful of your partner whose life doesn’t seem to have changed that much. So it was good for us to reconnect by just going to the pictures, having a night off. – Daniela Some families do not want other people to look after their children, or do not want to be away from them. Professionals should respect their choices and find other ways of giving support such as: a disability support worker to assist with care while the parent is at home; support to enable the parent or caregiver and child to take part in events or celebrations in their community; or referral to a playgroup or other community-based group to help reduce social isolation. Emotional support and appropriate referral The roles of many professionals involve a component of emotional support for parents and caregivers. Emotional responsiveness is critical to family-centred support and building trusting relationships. However, it is important that professionals recognise the limits of their role or skill set and refer appropriately to address emotional support needs when they are expressed. Say your relationship is breaking down. The case manager has been focused on getting you incontinence products or a bike. It’s an intimate thing to say, ‘My husband’s not coming home until 8 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 63 o’clock at night and now this is happening …’ You need to be able to trust that person, and that you will get a result from saying that, like a referral to a family relationships service for carers, or more respite to work through some of those issues. – Association for Children with a Disability family support worker Professionals might need to refer families to supports and services to help them deal with a range of stressors, including social or geographic isolation, poverty, homelessness, family violence, mental ill-health, drug and alcohol issues and chronic illness. Referrals might need to be supported (that is, professionals might need to do more than provide information and a phone number), and ongoing liaison might be needed with the other service provider. Supporting siblings Addressing the needs of siblings is a crucial but sometimes neglected aspect of family-centred practice. It’s important not to generalise about the experiences of siblings of children and young people with a disability. Their needs and choices vary widely, and their feelings about having a sibling with a disability can also vary a lot over time. According to the Association for Children with a Disability’s Growing together booklet,105 such experiences and feelings can include: increased compassion, understanding and maturity compared with their peers isolation, if they are not in touch with other siblings of children with a disability embarrassment arising from the negative reactions of others in the community anger and resentment, perhaps because of the impact of their sibling’s disability on their family and the increased time and resources taken by that sibling responsibilities beyond those of their peers pride, love and joy about their sibling’s achievements lack of information about their sibling’s condition and anxiety about it, including anxiety about their own future and that of their family and sibling grief and loss for the ‘sibling they didn’t have’, or if their sibling dies feelings of pressure to be perfect, to ‘make up’ for what their sibling cannot do frustration about limited opportunities to become independent of their family and caring role closeness with their sibling with a disability but sometimes difficulty with communicating or playing guilt, for example, that they are not helping enough, or that they can do things their sibling cannot do protectiveness, and a role in advocating for their sibling or supporting them to advocate for themselves. Sometimes addressing siblings’ needs involves helping parents and caregivers deal with the response of their child with a disability when a new baby arrives: When my other daughter was born we had huge issues with Ella. Ella was very violent towards her. It was a nightmare, the darkest days I have ever experienced. I went to her teacher at school and said, ‘What do I do? I need help! I am not coping.’ Together we put together social stories. The teacher sent stuff home for me to work on with her and spoke about it with Ella at school. – Ingrid Sometimes professionals can support siblings by validating their brother or sister with a disability: We were having issues at home with one of Michelle’s brothers saying, ‘Why did she have to be born?’ At that time Michelle had been trying really well (at school). I went to the school and asked if she could have an award or something in assembly, to show that she’d been achieving. I said, ‘I’m asking this for two reasons. One is for Michelle. And the other is for her brother.’ The teachers said, ‘Great idea’, and they did it. And I think it’s changed the tone a bit because Michelle’s not always just in trouble. I don’t think Stefan’s had an award, but Michelle has! – Melissa Sometimes professionals can assist by integrating siblings into activities (see Paula’s story on page 188), Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 64 referring them to siblings groups or all-inclusive family activities (see Melissa’s story on page 35) or providing care for them during respite. They can also validate siblings’ roles and support family relationships by suggesting or supporting creative ways to include them in helping their brother or sister with a disability: I was working with a family with a young son with autism and two other teenage boys. The family was struggling with the youngest brother throwing things, and his behaviour generally. The teacher and I encouraged the family to implement a lot of early intervention strategies, and I asked if the older brothers could help. The mother said that until they started doing this, the siblings had ignored their little brother. They used to go into their room, and had nothing to do with him. But after that, it was just amazing – the siblings helped this child come to a point where he is now. The principal of the school he is transitioning into rang me to say she can’t believe how much his social skills have improved. His brothers were doing little videos of what you should do when you greet people, to say hello and goodbye. The siblings got involved, and got him involved. – ECI professional Linking people into community Social inclusion and community connectedness are widely recognised as key factors in people’s emotional wellbeing.106 Strong informal networks of support are a key factor influencing improved outcomes for children, young people and families. Indeed, evidence suggests that other aspects of family-centred practice are less effective without such support. 107 However, consultations for these guides highlighted the common experience among families of increased social isolation (see Daniela’s story, page 39 and loss of social supports. When I was thinking about mainstream or special school, a friend said to me, ‘Well if you ask me, integration has never worked’, which shocked me. When I started Michelle at [a specialist integrated] kinder, another said, ‘Isn’t it good they’ve got places like that for people like her?’ We had a big circle of friends, but there was this segregation, no understanding that Michelle needs to mix with mainstream kids. I got tired of fighting. Even my in-laws don’t know how to handle her; they say, ‘She was so good today’, like they expect her to run amok. You get these attitudes everywhere – it gets tiring. – Melissa Professionals should offer people options for linking into the community. Some will gain most from linking into their local community. Many service clubs have grants programs and discretionary funds that can be used for one-off purchases for members of their community with special needs. Likewise, service clubs, places of worship and other similar organisations can often assist with transport, day trips and social support for people who are socially isolated. Neighbourhood houses often host support groups and provide low-cost classes. Aboriginal and CALD families should be offered information about mainstream groups, but many will also appreciate information about groups and other supports targeted to their cultural community, especially if mainstream groups are based on a different approach to disability and care from their own. In [the Aboriginal] community, it’s very rare that the person with a disability and their carer is separated because the carer feels a duty to care for the person with a disability and the person with a disability doesn’t want to be without the carer. Often people don’t engage with support groups because their carer is not invited, it’s for them. – Jody Saxton-Barney, Victorian Aboriginal Disability Network For some families it will be important to make links with other people facing similar issues, such as parents and caregivers whose children have similar diagnoses or who are at a similar developmental stage. Support groups, play groups and carer support services can be good options, while online groups are helpful to many (some are moderated by professionals who offer support and referral, but others are not). Professionals should also offer support to children, young people and families to engage in groups, especially if they don’t have a history of community participation. For example, people might appreciate meeting the coach or another person from the local sporting club or the convenor of a support group before attending a session. Professionals can provide ongoing support by asking how it went, encouraging the family or young person to reflect on how the experience did or did not meet their needs, and (in the latter case) what other kinds of groups or supports might work better for them. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 65 Many people speak positively about their experiences of groups, and many experience them as a lifeline. But groups are not for everyone. If someone says they are ‘not a group person’, professionals should respect that choice, while leaving open the possibility that they might change their mind later on. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 66 Tailoring supports to people’s capacity Professionals must tailor services and support to the capacities of children and young people with a disability and their families. Doing this well is a fundamental skill. We had a fantastic young speechie, a real gem. She had come up with this whole program of 20 minutes a day that mum could do at home after her daughter got home from school. She laid it all out, and the mum said ‘yes, yes’. Then the speechie left, and I said, ‘Right, let’s talk about what we’ll really do’. The mum burst into tears, and talked about how impossible it would be, however nice it sounded. We ended up arranging for the speechie to write down for mum exactly what she was doing with her daughter while at school, so that when she could, mum could also support that at home. But the rest of the time, I encouraged her to just enjoy being with her child. – Sue, principal of a special education school A critical issue for many families is that although the expectations of one professional might be reasonable in isolation, in combination with everyday pressures and the expectations of all their other service providers, they can become unmanageable: You visit therapists or doctors and they say, ‘You need to do this five times a day, you need to do this three times a day, you need to do this two times a day, or your child will not reach their potential’. That pressure is extraordinary. And you’re saying, ‘That’s all well and good, but in the meantime I’m also caring for another child, trying to get to appointments, trying to manage a house, do the shopping, feed every three hours. It’s just not a realistic goal. As a parent sometimes you need to say, ‘That’s just impossible, please suggest something achievable’. – Cass Tailoring supports includes checking in regularly to see if an approach is still manageable and identifying any additional support needs that may have arisen. Responding to change Professionals need to recognise and respond to a variety of changes that affect children and young people with disabilities and their families, including developmental change. Human development is a complex and variable process, and change is usually incremental. Sometimes parents and caregivers recognise it easily. Sometimes a professional might be the first to observe it. There should then be discussion about any impact the change might have on the goals and design of services and supports. Whether the child or young person has increased capacity should also be discussed. If they are able, they should have a say in any planning or implementation issues that arise. Professionals also need to be responsive to the many other changes that affect people’s lives. Families might manage their time and resources differently (and perhaps need more or different support) when a baby arrives or other challenges arise: the death of a grandparent; changes in housing or employment; parental separation; or illness (including hospitalisation) of a parent, caregiver, other family member or the child or young person with a disability themselves: Very early on when Emily was spending a lot of time in hospital, I was trying to juggle the other two kids, and my job and my husband’s job. We had a good amount of respite, but when she was being cared for in the hospital we would lose it all. I found that so hard. If ever I needed someone to mind her, it was then, while I went to pick Anthony up from kinder, or went home to have a shower. Emily fractured her leg while she was in there – it was broken somehow while I wasn’t around. I’m sure it was an accident, but at the end of the day I felt that she had to be monitored quite closely. – Amy Our case managers have really assisted our family through some difficult times. In our chaotic life they always seemed so organised. They have always been in tune with what was happening in our family, especially during times when we needed extra help, like when Samuel’s brothers were born. They spoke to us beforehand, and we discussed what additional help we might need. It was reassuring to have a plan in place and know that they weren’t going to say, ’There’s no more funding left’. – Paula Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 67 Some families and communities experience more change than others, for a variety of reasons, and require a higher level of flexibility and responsiveness from professionals and services to meet their needs: A worker might come in and say, ‘You can do this, and put this in place’, and it might work for a couple of weeks, and then there’s a funeral, or there’s been a family violence matter, or they all get up and go away, or the routine changes. It’s really hard for the community to understand routine for children with disabilities because they’re just part of the mob. Workers shouldn’t feel that this part of the work is a failure, they need to be flexible … [Also,] there are a lot of expectations on parents, but if they can’t do it, then they can’t. Workers have got to be pretty flexible to say, ‘We’ll just give it a go, just keep going until you get what you need’ – that the child gets after-school care, or a wheelchair, or the family gets a caption TV, or a fire alarm they can see. – Jody Saxton-Barney, Victorian Aboriginal Disability Network Transitions, especially between different settings or sectors, can also be periods when families require higher levels of support from professionals. These can be especially stressful times, and people sometimes struggle to find their feet and define their needs in the context of practices and funding models that might differ greatly from those they have encountered before. Shifts between practitioners, service providers and funding packages can also have an impact. Professionals can support families during transitions by: offering to share information with other services (with permission), including medical and other personal information, effective (and ineffective) approaches to working with the child or young person and information about the needs and preferences of the child or young person and family offering to engage in collaborative planning with new services or advocating for the child or young person’s needs with the new service (see Paula’s story, page 188) engaging in processes to support transition (such as transition statements for early childhood educators) offering newly engaged children, young people and families information about how their service works (including its family-centred approach, especially if it differs from those they have encountered before) and how it fits into the wider support system offering support for families transitioning into and out of the service. Professionals should also consider their own and their service’s responsiveness to change, and in particular their processes for reviewing the services offered to children, young people and families, to ensure they stay in touch with both developmental and environmental changes. They need to ask: how often reviews occur, at what points, and who can initiate them what questions are asked in review processes, and of whom how children, young people and families can communicate to the professional or service when their needs change at other times. During transitions between sectors, organisations or service types, families might be confused or find it difficult to define their needs in the context of differing practices and funding models. It is vital to discuss with families how changes for their child or family might impact on the supports they have. Pull out box - Personal perspective: Anita, Peter, Michael, Ryan and Claire ‘When Michael was young,’ says his mother, Anita, ‘like for any other child, I made the decisions. As he got older, I started to realise he should have a say. I still manage overall, but he has choices within that. For instance, when he’s doing reading and numeracy tasks with a carer, Michael chooses what to read, or what game to play.’ When her son was a young teen, Anita realised that other boys his age were often out in the community. Michael’s regular carer then ‘went down the street every Saturday morning for two years with him, supporting and growing his skills in finding his way, safely crossing roads, and using money. It’s given Michael a real measure of independence, a real self-esteem boost. He says to me now, “I’m going down the street to get a DVD”. It’s great, because like any young adult he has that freedom.’‘Michael’s got ambitions,’ Anita says. ‘He wants to drive a silver Mazda, to live in London, he wants a girlfriend, and to work in a video shop. He is just like any other teenager! As much as anything, he wants independence. He doesn’t want me to go with him because I’m his mother.’ Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 68 8 Technical quality Key messages Professionals need the expertise to deliver high-quality services and supports to benefit children and young people with a disability and their families. Research shows that a significant barrier to family-centred practice is when professionals are trained in models where the service provider is seen as the expert. As evidence grows of the efficacy of family-centred practice, the skills it requires are likely to be more highly valued, and to be emphasised in pre-service and continuing professional education and professional standards. Professionals need to find or develop family-centred tools and methodologies in intake, assessment, planning, design, implementation, monitoring and evaluation of services and support, which will enable them to draw upon the rich knowledge that children, young people and families have of each other. Most families have multiple service providers, and would benefit from increased service integration, from professionals sharing information (with permission) to coordination, collaborative planning, integrated support and highly developed partnerships. At a minimum, it includes professionals developing referral and secondary consultation relationships with other key services. Self-care is important for occupational health and safety and professionals’ capacity to work well with children, young people and families. It includes clinical supervision, debriefing after difficult or critical incidents, regular debriefing and check-ins with a supervisor, peer support, breaks and holidays, and professional development. One important aspect is the maintenance of appropriate personal–professional boundaries with families; these vary by culture and context but are best set by organisations and should be clearly communicated to staff and families. Children and young people with a disability and their families rely on professionals to have the knowledge, experience and skills – the expertise – required to deliver high-quality services and supports. Professionals gain and maintain expertise through their pre-service training, experience, supervision, networking, secondary consultation, reading and ongoing professional development. Within family-centred practice, technical quality is about how service providers apply their expertise for the benefit of (and in partnership with) those they are working with. This guide touches on some of the areas of technical expertise that are most applicable across all sectors, and most relevant to family-centred approaches. The sector-specific guides drill down into other areas of expertise pertinent to each setting. Family-centred practice is, of course, only one element of high-quality service delivery. Current thinking in best practice more broadly can be accessed through professional journals, training and further education. Many professionals also hold leadership positions, and their approach to management can influence staff members’ capacity to work in family-centred ways (see chapter 9 and the organisational guide). Professionals need a wide range of technical knowledge other than that specific to their discipline or training. This includes knowledge of: various conditions and disabilities; colleagues’ modalities; the services, processes and procedures of their and related services; funding and the policy environment; and the impact of privacy laws, including on sharing information between family members and services. Family-centred practices as core professional skills Professionals need to understand family-centred practice as an approach rather than an end in itself: Sometimes staff get mixed up between family-centred practice as a vehicle to get to the outcome, or family-centred practice as the intervention. So they start to say, ‘You don’t need my expertise’. The Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 69 answer to that is, ‘Yes we do, but we also need you to be able to work in this way’. It’s about not throwing the baby out with the bathwater. – Service manager As discussed, family-centred practice requires a shift in power and authority from the professional to the family. Various researchers have identified challenges that family-centred practice poses for professionals, especially those working outside a family systems model, which considers the parent–child relationship as part of the ‘intervention’.108 Some researchers have found that a significant barrier to family-centred practice in some sectors is that many professionals were ‘trained in models, such as the medical model, in which the service provider was seen as the expert’. 109 One Australian study focused on professional issues for physiotherapists, finding that ‘moving towards a family-centred focus creates significant challenges for more traditionally trained physiotherapists in the way they gain and utilise information from patients and family members’.110 Some professionals’ pre-service training might not have emphasised (or addressed) familycentred approaches to core skills and competencies, or seen family-centred practice as a skill in itself. As evidence grows of the efficacy of family-centred practice in various settings, this is likely to change. Indeed, changing approaches in ECI led to the development, in 2009, of a set of professional competencies that put family-centred approaches squarely at the centre of practice. 111 Meanwhile, many services continue to provide comprehensive orientations to the approach for new staff. Consultations for these guides also highlighted some innovative approaches to practice change, including mentoring and reflective partnerships (see the organisational guide). Using family-centred tools and methodologies Professionals need to find, develop and use appropriate tools to draw upon the knowledge of children, young people and families in intake, assessment, planning, design, implementation, monitoring and evaluation of services and support. For example, research indicates that most parents and carers have a very good understanding of their child’s development and disability. One study found that parents asked to estimate areas in which their child was developmentally delayed were 80 per cent correct when their responses were compared with the Bayley motor scale. Furthermore, it found that parents were correct 91 per cent of the time in estimating if their child was on target in their development. 112 Many tools and methodologies are available to professionals in each sector and professional setting, each with their own strengths and weaknesses. Whatever is used should go beyond the ‘tick a box’ approach and allow the professional to develop a ‘rich, strengths-based account of the child [or young person] incorporating their and their family’s perspectives’. 113 Consultations for these guides revealed many examples of excellent practice, but also that this is not every family’s experience: The paperwork is ridiculous … [it asks] the same questions every time, not getting to the next layer … You know my child’s diagnosis, how old she is, who’s in the family, what medication she’s on, is she toilet trained, can she feed herself. But does that tell you how Casey lives her life? And does that tell you what’s important to Casey and us, for Casey to be the best and happiest she can be? – Donna Professionals also need to draw on parents and caregivers’ knowledge of their child in relation to how to conduct assessments; not doing so can have significant consequences: I kept saying, ‘Warn me when you do [the IQ test] because I need to explain to her what’s going to happen that day so she’s in the right frame of mind’. Michelle is one of these kids that likes to muck around, likes to get reactions out of people and make people laugh. She’s just a kid! There came the day, I got this phone call at 11 o’clock: ‘We’re doing the test today’. And I said, ‘Well good luck because she hasn’t been prepared, she’s got no idea what she’s doing’. And sure enough that’s what happened. She got into the room, and kept doing the wrong thing, trying to get a reaction. She’s never seen this lady. So she kept marking everything wrong and came back with an assessment of IQ48, which meant if I put her in a special school, it would have to be a special development school. I knew she didn’t belong in an SDS, but the psychologist refused to change it. You can ask them to re-do it, but they only do it every two years because they feel that the child gets too familiar with the questions. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 70 So I went and had a different one done through a private psychologist and she came back with a much higher score … Michelle’s self-esteem had a real battering that year. She spent lots of time playing games on the computer, her behaviour was really bad and her self-esteem was so low. – Melissa It is important that the methodologies used, and the language within them, engage professionals in thinking about meaningful aspects of practice, including how their practice might be improved: We began using the language of ‘family life at the centre’ of intervention. We kept the term ‘intervention’ in there, and immediately staff were more engaged. The discussions then became about family life and intervention, and what would an assessment look like if family life – or the family – were at the centre of it. So you can still do fairly formal assessment, with questions that you ask families before, during and after like, ‘How would we see the best in your child?’, ‘Is this bringing out what your child can do?’, ‘Was that a good assessment of your child?’. There are other questions – ‘Are we not doing it right, what could we do differently?’, which can be quite challenging. – Service manager Working towards service integration Many families have more than one service provider, whether from the same agency or different ones. Consultations for these guides highlighted many families’ experiences of reduced service quality, service gaps and contradictory information arising from a lack of service integration, including contradictory advice and unrealistic expectations from individual professionals: Therapists often say that it’s really what you do at home that matters, so there is usually ‘homework’ to do with your child between therapy sessions. This means that sometimes there is speech therapy, physiotherapy and occupational therapy homework to do. The therapists are not necessarily aware of everything else that you are dealing with at home – medications, bed-wetting, other appointments, let alone the needs of the rest of the family. And if you’re seeing them privately, then the speech therapist doesn’t know what the physio has said – the only person who knows it all is the parent. It is usually the mother who has to process it all somehow. Sometimes you can do it well, and sometimes you just have a nervous breakdown. – Anita Professionals can significantly assist families by sharing information with each other, with the family’s permission (see Jan’s story on page 72). Consultations highlighted many examples of where efforts to improve communication and coordination significantly improved service quality and effectiveness. When I’ve sat down with the team – the caseworker, the parent, the other workers – that’s where I’ve seen a little bit more progression with the child. I’ve seen strengths that we’ve been able to work on because we’re following up information that’s not out of date. Swapping ideas with each other and the client. – Disability support worker Improving service integration requires both skills and good processes. Children, young people, families and professionals all benefit when: everyone involved understands each other’s roles, skills, area of expertise and practice approaches everyone knows and is focused on the needs and priorities of the child, young person and family everyone (including the family) is kept up to date (email, communication books, case conferencing and regular telephone contact can all be helpful) there are processes to resolve any problems. In some cases, coordination moves to the level of significant collaboration, especially when specialist disability or early childhood intervention services provide support to mainstream organisations to enhance service provision: Ruth goes a couple of days a week to a special school and a couple of days a week to a Jewish school. The coordination is brilliant. Meetings, emails, phone calls. When Ruth first started at Jewish school she was a mess. She ran riot and the school had a hard time with her. Then the teacher from Ruth’s special Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 71 school came to the Jewish school and talked with the teacher about the issues and devised some strategies. I tell you what, they did this and they had a different child. The Jewish school will do anything. They really want Ruth. – Deborah Sometimes such partnerships develop even further, towards a high degree of service integration: A lot of parents want that choice of their child attending a mainstream educational setting, but you get a lot of resistance from schools who don’t feel that they can do it. We set up a classroom in a mainstream school. We put our staff into it, and our kids, and they would go there three days a week. A lot of those kids have now learned the skills for being in mainstream school – this is what you do when the bell goes, this is where you put your bag – and have now jumped off, into the mainstream setting, some at that school, some elsewhere. – Service manager Most professionals are at times called to work in collaboration with others who come from a very different perspective or discipline, including those that are less person or family centred. This can be challenging for everyone, yet whatever support family-centred professionals can offer to improve communication, coordination and integration with other services will be beneficial to children, young people and families. My challenge is to work with other agencies that don’t see family-centred practice as being central to their work. Many agencies we work with work in isolation with the client, and don’t see the importance of working with the whole family. Trying to educate them is a real challenge, whether that is through a forum, or partnership and liaison, or case conferencing. Involving everyone and discussing the issues, delegating roles and responsibilities – time spent is the key. – Case manager Referring and using secondary consultation Professionals need to know how to refer appropriately to meet a variety of needs, including for new or different disability supports, or for information on diagnosis or medical treatment, including a second opinion. Practitioners also need to know how to identify signs and risks of mental ill-health, suicide, drug and alcohol abuse, sexual abuse and family violence, and how to refer in response to these and other needs, such as for diagnosis, counselling, family therapy, parenting programs or carers support, or for income, housing or legal support. This requires an up-to-date knowledge of the service sector and/or ready access to a good database of services and resources. If a professional cannot meet a particular need, they need to offer alternatives without making people feel ‘fobbed off’. It can be helpful if the professional can: be specific about the need they cannot meet and why discuss what services might meet the need, including the type of service, location and hours find and provide any information they have promised promptly (lack of follow-through by busy workers is a common complaint from families). Professionals should also discuss with the family whether the other agency is family centred, their expectations of support from the agency, and how they might engage with it. If it’s possible for the professional to offer support, for example, with referral, ongoing liaison, coordination or information sharing, discuss all these possibilities with the family, if necessary seeking their formal permission. Professionals should establish ongoing relationships within services they refer to, contact for secondary consultation or collaborate with for co-case management, planning or project work. This might include Child FIRST services, multicultural and Aboriginal organisations or those with expertise in LGBTI issues. Pull out Box - Personal perspective: Jan, Sean, Lachlan and Louise Jan and Sean really appreciate it when the professionals in their daughter Louise’s life work as a team, even if they’re from different agencies. ‘No one has really designed this team other than us,’ Jan says. ‘But if they can communicate with each other, that’s good. So the paediatrician’s reports go to the psychologist and the GP and the speech therapist. That way they’re all up to date with each other about what’s going on.’ Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 72 Jan also values the capacity of professionals to think about the family’s future and ‘whether they are coping’, and to know the role of other services well enough to refer appropriately: ‘Our speech therapist, for example, sent us to the psychologist for the IQ tests and behavioural support, and also referred us to a paediatric neurologist. It’s being able to look at other needs, and know what other service providers would do.’ ‘The best workers we’ve ever had are those who can see the needs of the whole family,’ Jan says. ‘[Who] can very much support the mother and father, and talk about issues that would be on their minds, and have empathy with the child, and the sibling. So the speech therapist, for example, has helped with Louise’s speech and social skills but also talked to us as parents about how to handle behavioural issues.’ Another example is the psychologist, who has helped Louise (who has an intellectual disability) work through her feelings about changing schools and supported the whole family to work through the issue together. Self-care and maintaining appropriate boundaries Self-care is a skill that many human service professionals pay too little attention to. Self-care practices are important for professionals’ occupational health and safety (including their mental health), as well as their capacity to work well with children and young people with a disability and their families. Useful self-care practices include: clinical supervision; debriefing after difficult or critical incidents; regular debriefing and check-ins with a supervisor; peer support; breaks and holidays; and professional development. There needs to be strong organisational support to enable staff to take care of themselves, including appropriate agency policies, time and resources for debriefing and supervision (which might include external clinical supervision), strong management skills and a culture in which self-care is seen as an important contributor to occupational health and safety and service quality. One important aspect of self-care is the establishment and maintenance of appropriate ‘boundaries’ between professionals and the children, young people and families they work with. This can be confusing for everyone involved, given that care and empathy are key to building trusting, open and collaborative relationships. Many professionals work in people’s homes and engage with intimate facets of their daily life: Sometimes I find it challenging to find my place with professional and personal boundaries. You want to give as much as you can personally, without pulling down all your boundaries. Sometimes you’re working so closely in family-centred care, it can be difficult when the family has an issue you’ve encountered in your personal life. Through debriefing I’ve discovered that it’s important not to let too much of yourself out. Maintaining my own personal and professional boundaries has helped me avoid burning out, and from getting too emotionally involved. – Disability support worker A caring professional can be an emotional lifeline in tough times, but they are not a friend or part of the family. Appropriate personal–professional boundaries are best set by organisations, and should be clearly communicated to staff and service users. Where those boundaries lie might vary between organisations and communities. For example, the reality for many rural and cultural communities is that people often know or know of each other: We have a lot of small communities in the area we work, and I often have staff who live in those communities. It’s for them to work out that boundary, and maintain confidentiality, but I have an expectation, as their manager, that they will often find that tricky. – Disability service manager In Aboriginal organisations people are likely to be connected through diverse lines of kinship, and different boundaries might apply. Personal–professional boundaries will also be influenced by cultural values around caring roles: Sometimes community sees a support worker’s role as blended. You become a friend; everything becomes intertwined. You get invited to community events, parties. So the boundaries need to be very strong, and written down. There need to be guidelines for families to know that the worker works from nine to five, and this is the emergency contact person after five o’clock. – Jody Saxton-Barney, Victorian Aboriginal Disability Network Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 73 Whatever boundaries suit a particular organisation and context, if they appear to be shifting in an inappropriate direction in a particular professional–family relationship, the issue needs to be thoughtfully addressed in supervision. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 74 9 Family-centred organisations Key messages Action on family-centred practice requires change at the level of the individual professional, within the professions that feed into the sector, within organisations, and within the service system as a whole. At every level this should be informed by consultation with and participation by people with a disability and families. Organisations can support staff through professional development and orientation programs, in supervision, through reflective practice and other team-based learning approaches and through use of written materials (such as these guides). However agencies manage resource allocation and staffing, family-centred practice requires that staff have adequate time for meaningful partnerships with families, and with other services. Recruitment also offers the opportunity for building capacity in family-centred approaches. There is a link between how organisations are operated and the quality of partnerships between family and staff using their services; this should reflect values like flexibility, openness, teamwork, respect, good communication and creation of a participatory, creative, collaborative and supportive culture. Agencies need to ensure their systems, policies and procedures are family centred, including staffing, record keeping, information sharing and complaints handling. The approaches of reception, finance, communications and other staff should also be family centred, as should the physical environment. Organisations should find ways for families to direct their own supports, and for their views to inform organisational and program development, and positive change at a broader level. Families can have input into organisations in many ways, but these will only be effective if supported across the organisation. Services can increase service integration by encouraging staff to ask families how they want their services to work together, and working more collaboratively with their other service providers. Organisations can come together to strengthen relationships, share learning, deepen knowledge of each other’s services and approaches, build each other’s capacity, and work towards more uniform, streamlined and coordinated approaches to service provision. Many Victorian professionals are committed to family-centred approaches in their work with children and young people with a disability and their families. Yet how effective any individual professional can be in increasing the family centredness of their practice will always be limited without support from their organisation and beyond. Making the services and supports that children, young people and families receive more family centred requires managers and organisations to act on multiple levels: to nurture good practice among staff; to make the organisation and its policies and procedures more family centred; to ensure agencies work together to form an integrated service system from the perspective of families; and to contribute to thinking within the relevant professions. At every level, action to strengthen family-centred practice should be informed by self-reflection, evidence and the diverse views of children, young people and families themselves. As mentioned (and discussed in chapter 10), evidence indicates that participation by and feedback from families is the touchstone for maintaining and improving practice.114 Organisations need to find meaningful ways for families to direct their own supports, and for families’ views and needs to inform organisational and program development, as well as positive change at a broader level. Many agencies are finding innovative ways to support change towards greater family centredness on all these levels, as is explored in some detail in the organisational guide in this suite. That guide’s key messages are summarised below. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 75 The barriers to change Researchers in ECI and allied health have identified a number of barriers to increased family-centred practice115 including: lack of time, human and financial resources116 lack of support from the organisation to use family-centred approaches117 professionals’ lack of understanding and valuing of family-centred practices118 professionals’ lack of skills around collaboration and partnership with families 119,120 professionals’ unwillingness to reconcile with families’ views that differ from their own 121 pre-service training based on service models in which the professional is seen as expert 122 lack of information resources available to give families that account for social, cultural and language considerations and differing learning needs 123 under-utilisation of families as a resource for sharing information, support and knowledge 124 parents and caregivers’ expectations (perhaps based on advice from referring medical practitioners) that support will be delivered exclusively by therapists in therapeutic settings, rather than being integrated into their child’s natural environment and daily routines 125 lack of skills in working cross-culturally, including deficit-based views of CALD families, cross-cultural misunderstandings related to the meanings of disability, and differing views about the goals for people with a disability and the role of caregivers.126 Within early childhood education, a 2010 review of the literature cited challenges for practice, including: prior practices, attitudes and beliefs, especially among professionals who are ‘not used to considering families as equal partners in young children’s learning and development’ that pre-service training needs to build knowledge of the research and theory of family involvement in children’s education and include practical skills training for collaborating with families. 127 In a project to support increasing family centredness in children’s services in NSW, Gowrie Children’s Services identified barriers including: for staff: lack of training, inadequate staff support, a youthful workforce, staff turnover and attitudes for organisations: lack of time, lack of commitment from service operators, difficulties creating a familyfriendly environment and lack of childcare places.128 Within schools, research highlights the role of leadership as facilitating of (or restricting) family-centred practice, and the need for increased skills among both teachers and school leaders in working with parents (the basics of family-centred practice), and understanding parents’ roles in their children’s education.129 A framework for action As with the family-centred practice model (see page 25), it is useful to have a framework for thinking about how to support action on family-centred practice beyond what individual professionals can do. This guide uses one adapted from the NMHRC’s dimensions of cultural competency. 130 The framework comprises four interrelated dimensions for action, informed by service-user participation at every level. Individual – Knowledge, attitudes and behaviours defining family-centred practice are maximised and made more effective if they are within a supportive organisation and wider service system. Individual professionals feel supported to work with children, young people and families to develop relevant, appropriate and sustainable services and supports (see Figure 2). Profession – Family-centred practice is an important component in education and professional development. Relevant sectors and professions develop standards and quality frameworks that incorporate family-centred practice to guide professionals’ working lives. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 76 Organisation – A culture is created when the skills and resources required for family-centred practice are in place and are integral to core business. Families’ views and needs inform development and planning and the design, implementation and review of programs. Service system – Policies and procedures for family-centred practice are effective when in place across all sectors and the whole service system, and mechanisms and sufficient resources for fostering and monitoring family-centred practice are present at all other levels. Figure 2: Four interactive dimensions for action on family-centred practice Adapted from NMHRC model Supporting staff to be family centred Professional development and orientation Organisations need to consider which aspects of family-centred practice can best be supported through professional development, considering both staff experience and prior training. One study found that professionals who had been in the workforce for more than 15 years had most difficulty embedding familycentred principles into their practice.131 Many professionals need support to better understand the relationship between family-centred practice and their technical expertise. This might be a particularly valuable focus in orientation programs for new staff, given the current lack of focus on family-centred approaches and related skills in many pre-service courses. Feedback from service users should inform priorities for professional development. Organisations should also consider how service users might directly inform or participate in professional development. Supervision Managers need to support family-centred practice through supervision. Especially in the context of reorienting practice, supervision can be a useful forum for keeping staff focused on the basics and helping them better understand how to use their specialist skills working collaboratively with families: Family-centred practice is about understanding what is making the difference for that family. For some, that might be about respite, or being able to pay the bills and the rent. You have to keep having the conversations with workers about that: look at the feedback that the family is giving – this is what is Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 77 important to them right now. It is about understanding that there are many ways we can make a difference that are much broader than just providing discipline-specific support. – Team leader Family-centred practice requires support from managers if staff are to be flexible in their delivery of services and supports to families, without going outside their role, service parameters or working conditions. It’s important to ensure families don’t feel ‘caught’ between staff wanting to respond in one way to an expressed need and their supervisor who has a different view. Deeper engagement with families may mean that staff need to deal with a greater range of issues for families. Support for building their skills, resources and knowledge to do so may come from supervision or colleagues. Many staff are also likely to value support within supervision regarding maintaining appropriate personal–professional boundaries. This, along with debriefing as needed about difficult or critical incidents (sometimes requiring external supervision), can assist with staff self-care and prevent burnout. Reflective practice, team-based approaches and using written materials Some organisations maintain and improve family-centred practice using team-based learning. This might be as simple as regular team meeting agenda items focused on ‘what I am doing that is family centred’, reflective practice or practice development sessions, ‘shadowing’ experienced colleagues, or video-assisted reflection in which a professional reviews a video recording of their interaction with a family, whether alone or with their supervisor or team. A 2005 joint Canadian–British study132 investigated the impacts of a set of family-centred service fact sheets on professionals, students and families, confirming that such tools most effectively contributed to practice change when they provided support for new knowledge through interactive and interpersonal strategies, including problem-based learning, interactive workshops and educational outreach visits (for students). 133 Organisations might consider using the guides in this suite to support professional development, reflective practice, team discussion and practice-based learning. Wilson and Dunst’s Family-centred practices checklist134 was developed for use primarily in supervision (although it might also be used to support team discussion) focusing on relational and participatory practices. Managers might consider expanding the tool to cover relevant technical skills and knowledge in line with staff key performance indicators. Whole-of-organisation approaches A number of researchers make a link between the way organisations operate and the quality of partnerships between staff and families using their services: If program personnel truly believe in collaboration and working with families, their behaviours as administrators, individuals, and team members, and the manner in which their programs are organised and operated, will send a message that reflects these basic principles. This belief will be translated in the characteristics of the personnel who are hired and in the support and respect that administrators give their staff, all of which affect the individual relationship established with each family. 135 Managers and governance bodies wanting to strengthen family-centred approaches in their organisation must ensure the core values of family-centred practice inform their agency’s values, including its mission or values statements. More broadly, they need to lead the creation of an organisational culture that: values, supports, resources and monitors family-centred practice; is open to new ideas and learning; and supports the meaningful participation of families at every level, from directing their own supports to having input into organisational planning, programs, evaluation, communications and project work. The organisational guide contains more discussion about the role of leadership. Service development Managers need to consider family-centred practice in resource allocation, although it will always be one of many competing demands on existing resources. Family-centred approaches can sometimes require staff to know more, consult more, reflect more and do things differently. This might have implications for the amount Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 78 of time staff need to spend with families, what they do when they are with them, or even who they work with within the family (for example, respite workers providing care for siblings). There are many approaches to structuring organisations and allocating resources to ensure there are the resources, skills, knowledge and capacity in place to provide high-quality services and encourage an integrated approach to their delivery. However an agency resolves these questions, family-centred practice requires that staff have the time and capacity for meaningful partnerships with children and young people with a disability and their families in planning, delivering and reviewing supports and services. Staff also need the time and capacity to build collaborative partnerships with other professionals and organisations. Other key resources include: a good-quality database of services and resources; professional development; journals and other practice resources; and family-informed tools and methodologies. Training and support for current staff are critical to improving practice, but recruitment also offers opportunities to build capacity in family-centred approaches and skills, as discussed in the organisational guide. Organisations wishing to build capacity in cultural responsiveness should also consider employing staff from diverse cultural backgrounds, especially from communities in their catchment. Appropriately qualified and trained bilingual staff can add to an organisation’s capacity to offer linguistically and culturally relevant services and support. Management practices As mentioned, Tim Moore and others point to commonalities in positive, effective relationships between managers and staff, as well as between professionals and families, and suggest that one influences the other.136 Relevant values and behaviours that underpin family-centred practice include flexibility, openness, teamwork, respect, good communication and creation of a participatory, creative, collaborative and supportive culture. Working conditions should also be family friendly; flexible working hours that accommodate staff family responsibilities can add to agency capacity to meet service users’ needs. 137 One manager in the Victorian sector has taken a systematic approach to deepening family-centred practice within her organisation. A working group of interested staff has driven the project over a 12-month period, which incorporates a formal ‘buddy system’. Three-monthly report-back sessions are held in small groups or with the larger team, depending on staff preferences. The consultative, ‘bottom-up’ and evidence-based aspects of this approach have been key to its success: It was really owned and driven by people on the team. I’ve seen the development of some fantastic tools. There’s a lot of conversation and debate, and I have definitely seen some shifts in thinking and practice. It’s a big journey, and it takes time. But it’s because it’s come from within the group that we’re going to get better traction, better take-up. – Service manager Systems, policies and procedures Families can sometimes experience frustration with organisational systems, policies and procedures that seem less than family centred. The organisational guide lists some of the many positive approaches that Victorian services are taking to improve systems, policies and procedures including: rostering and hand-over systems that facilitate continuity of care; transparent record keeping and tools for information sharing; strengths-focused assessment templates; organisational partnerships that facilitate collaboration and integrated support; and clear policies and procedures around responding to suggestions, concerns and complaints raised by service users. As discussed earlier, for the most part, families experience a service primarily through their relationships with one or more of the professionals from that service. However, the skills and approaches of other staff (reception, administration, finance, policy, communications and fundraising) will also affect their experience of service provision, as will other aspects of organisational practice. Research evidence supports the value of creating a family-centred culture across an organisation. 138 Positive approaches among Victorian services include: waitlist management and offering of alternative supports: an ‘open door’; a welcoming and Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 79 accessible physical environment; regular family events; and regular, high-quality communication with service users. Family participation in organisations Research confirms the value of service-user participation in helping services become more responsive to the needs of service users and the community.139 There are many ways that both families and people with a disability can participate in organisations beyond directing their own supports. Offering multiple ways to get involved increases the likelihood that more service users (and more diverse service users) will do so; the organisational guide discusses a wide range of options for family participation. Service-user participation is only effective if well understood and supported at all levels of the organisation. The following issues relating to effective participation are adapted from evidence-based summary guidelines in a key Australian resource guide to improving services through consumer participation:140 Meaningful participation by families means that organisations must be prepared to change. The capacity of an organisation to increase family participation might need developing, which could require both training and structural change. Information sharing is crucial at all levels of participation, from service users to board members. Participation means providing many ways for families to ‘speak’ to organisations and organisations listening actively to what families say. Increased family participation might mean that conflicts emerge. When organisations recognise and manage these well, it can lead to better quality service in the medium to long term. Increasing family participation is about relationships and the skills and behaviours that help build them. Partnership with families is based on dialogue and trust. Trust is built through openness and consistency. Multiple strategies are essential for engaging diverse families and dealing with diverse issues. Families need to be engaged early, even in the process of deciding how best to engage them better. Organisations should take care not to promise what cannot be delivered, and be clear about their capacity to inform family involvement and respond to family concerns. A family-centred service system A number of studies identify the importance of providing coordinated and comprehensive care, 141,142 including coordination of service providers from different disciplines and different locations. 143 As soon as you manage to get one form of help, everything else falls off underneath it. It’s not one individual’s fault. It’s the system. Nobody talks to each other. They all have their own teams, and nobody seems to understand what the others do, or the decisions they make, or the impact they have. – Kate As discussed, professionals need to do what they can to improve communication and coordination with other services providing support to a child or young person with a disability and their family. However, many aspects of improving service coordination lie in the hands of organisations. Many of the developments that enhance service integration and family centredness occur at the level of policy and funding, rather than within or between organisations. Managers and governance bodies need to contribute to these as appropriate, for example, by contributing to sector consultations and supporting their service users to contribute to community consultation processes. There are many ways that professionals and services can (and do) work to increase service integration from the family’s point of view. Systems, policies and procedures within an agency can encourage staff to ask families what services they are using, and how they want their service providers to work together. Communication and coordination with a family’s other service providers (with the family’s permission and Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 80 participation) can be formalised. Secondary consultation or partnerships in supported referral build relationships between services and provide integrated support to a family. Organisations can come together to strengthen relationships, share learning, deepen knowledge of each other’s services and approaches, build each other’s capacity, and work towards more uniform, streamlined and coordinated approaches to service provision – refer to the organisational guide for more discussion. The VicHealth partnership continuum 144 defines four levels of partnership based on increasing degrees of commitment, and on willingness to change and share ‘turf’: networking, coordinating, cooperating and collaborating. Most partnerships within the service system for children and young people with a disability and their families – like partnerships in human services generally – are at the networking and sometimes coordinating end of the spectrum. In many contexts this is appropriate. In others families will very much benefit from work by managers and governance bodies to establish or move partnerships further along the spectrum. As discussed in chapter 2, partnerships are particularly important to increasing capacity in cultural responsiveness. Creating more family-centred professions As mentioned in chapter 8, a number of studies have identified that a significant barrier to family-centred practice in some sectors is that many professionals were ‘trained in models, such as the medical model, in which the service provider was seen as the expert’. 145 One Australian study, focused on professional issues for physiotherapists, found that ‘moving towards a family-centred focus creates significant challenges for more traditionally trained physiotherapists in the way they gain and utilise information from patients and family members’.146 Therefore, some professionals’ pre-service training might not have emphasised (or perhaps even addressed) family-centred approaches to core skills and competencies. As evidence grows of the efficacy of family-centred practice in various settings, this is likely to change. Indeed, changes in approach to practice in ECI led to the development, in 2009, of a set of competencies for professionals in that sector that place family-centred approaches squarely at the centre of practice. 147 Managers need to contribute themselves, and support their staff to contribute, to development in thinking around family-centred practice within their profession and sector. Family-centred organisations as learning organisations Managers and governance bodies need to find ways of conceptualising, planning and supporting learning around family-centred approaches at an organisational level. The notion of the ‘learning organisation’ is one idea that recognises the importance of both individual and collective learning. 148 It regards learning as ‘valuable, continuous, and most effective when shared [and sees] every experience [as] an opportunity to learn’.149 Other characteristics of learning organisations are that they: foster dialogue, making it safe for people to share openly and take risks; value learning approaches based on continuous improvement, such as reflective practice or action research; question predetermined beliefs and assumptions; continuously interact with their environment; and have a systems focus, looking at the whole organisation and the relationships within it.150 In many ways the idea of learning organisations connects strongly with the notions, values and behaviours that underpin family-centred practice. Some conceptualisations of a learning organisation see it as led by management while others regard it as necessarily more collaborative and democratic. The support of the organisation’s leadership will always be crucial to making any change sustainable. However, in the context of family-centred practice, more collaborative approaches seem appropriate, especially when collaboration is extended beyond the staff to encompass meaningful participation by families and people with a disability. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 81 10 Maintaining and improving practice Key messages Research shows it can be challenging to implement and maintain commitment to all aspects of familycentred practice, and that there is a tendency towards ‘professional drift’ back to more traditional approaches. Professionals and services need to engage in reflective practice and seek regular feedback from service users to maintain and improve family-centred practice. Professionals should both seek feedback from children and young people with a disability and their families during the course of their work, and ensure they have the opportunity to give regular anonymous feedback. Many tools have been developed for this purpose, focused on the relational and participatory aspects of family-centred practice. Services could adapt these to their context and expand them to cover technical areas in line with staff key performance indicators. There is strong evidence of the effectiveness of reflective practice for improving practice and achieving maximal outcomes for children, young people and families. Professionals can undertake this on their own, with peers, in supervision and in their teams. Reflective practice has been linked to action research and the need for critical reflection, where practitioners question their assumptions and how their values inform practice. It is therefore strongly linked to some of the basic elements of family-centred practice. Family-centred practice has informed work in some sectors for 20 years or more, and many professionals and agencies regard it as fundamental to their approach. As a philosophy it has driven significant change within many organisations, including the development of key worker and family coordinator roles, and multidisciplinary and transdisciplinary approaches. However, evidence shows it can be challenging to both implement family-centred approaches and maintain commitment to all aspects of the approach. Research has shown that many organisations and practitioners begin with a willingness to be family centred, but find it difficult to maintain all aspects of the approach over time; a phenomenon known as ‘professional drift’. 151 Other research suggests that a mismatch can arise between the degree to which professionals think they are working in family-centred ways and the experiences of children, young people and families. For example, a Canadian study of 309 early childhood services found that professionals felt they were doing well at communicating with parents, treating them as experts, considering family strengths, and providing a positive view of the future and how parents could help. 152 However, parents and caregivers in the study felt that professionals fell short in a number of key ways important for family-centred practice: in providing information in a variety of ways: in involving families in decision making; in assisting families to make decisions or receive equal services; in considering families’ practical constraints; and in making families feel comfortable asking questions or raising concerns. A later American study also showed that professionals rated the service they provided as more family centred than families did.153 In this case, the most significant factor for both groups was experience – how long the professional had been in practice and how long the family had been in the service system. While Australian evidence on the consistency between professionals’ reported practice and families’ experiences is lacking, seeking feedback from families ‘walks the talk’ of family-centred practice, and as such is valuable in its own right. As Treloar notes: Vigilance is needed to ensure that services remain responsive to families’ needs. At the heart is the need to listen to all that families say and to meet their expressed needs as far as possible. This requires consistent and ongoing evaluation of professional practice. In this, too, it is essential that families be seen as partners.154 Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 82 Professionals and services therefore need to both engage in reflective practice and seek regular feedback from service users to maintain and improve family-centred practice. Monitoring and seeking feedback Professionals should seek feedback from children and young people with a disability and their families during the course of their work and ensure they have the opportunity to give regular anonymous feedback without fearing it will affect the ongoing support provided to them. In more than two decades of research into family-centred practice, many tools have been created to measure the family centredness of various aspects of services and supports. Professionals and agencies might look at how these could be used to inform existing service user feedback tools or adapted to their organisation and context. For example, Dunst and Wilson’s Family-centred practices checklist155 is a tool for use primarily in supervision, focusing on implementation of relational and participatory practices. Services might want to give thought to expanding the tool to cover relevant technical skills and knowledge, in line with staff key performance indicators. Carl Dunst has also produced sample tools for use with families that professionals could use to develop a set of questions for children, young people and services during review periods or at other times (see the organisational guide).156 Organisations might also adapt them as a tool (or set of tools) for seeking regular feedback from children, young people and families. The organisational guide includes further discussion of issues related to seeking feedback from children, young people and families, including the design of tools, implementation of surveys or focus groups, analysis of findings, using findings to inform practice change and dissemination of results to service users. Reflective practice During consultations for these guides professionals often highlighted the need for reflection to ensure adherence to family-centred approaches: Family-centred practice is about taking a lead from the family, developing a rapport, going back to constantly review that family support plan, to ensure that you haven’t gone off on your own little tangent – that you don’t think you’ve walked in as the family’s hero. That can happen too. When you do develop the rapport, if every time you go in, the family says ‘You’re fantastic’, it can be very easy to get distracted from the game plan. – ECI professional Consultations were seen by many participants as an all-too-rare opportunity to stop, share ideas and reflect on their practice. Some managers described using innovative approaches to support family-centred practice in their teams and organisations, but many reflected on the difficulty of finding time to do so: There aren’t enough opportunities for staff to feed back how they are working in a family-centred way, and to share that with each other. That’s something we could introduce to team meetings, even if it’s just 10 minutes answering the question, ‘What are you doing that demonstrates a family-centred approach?’ People can learn so much from each other just by hearing those stories. – Service manager There is strong evidence that professionals who regularly reflect on what they do, why they do it and how this new knowledge can be used to improve their practice, achieve the best outcomes for children and families.157 This suggests the need for reflective practice, and indeed its usefulness has been widely accepted in human services in recent years. Yet research reveals a lack of clarity among professionals about what reflective practice actually involves. 158 Early work in reflective practice introduced the concepts of ‘reflection in action’ (thinking on your feet, which could also be linked with Australian researcher Tim Moore’s concept of ‘mindful practice’ 159 in family-centred contexts) and ‘reflection on action’ (thinking after the event). It has been described as ‘repeated cycles of examining practice, adjusting practice and reflecting on it, before you try again’. 160 Professionals can engage in reflective practice on their own, with peers, in supervision and in team meetings. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 83 Pollard identified the following seven characteristics of reflective practice for early childhood professionals: 1. an active focus on goals, how they might be addressed and their potential consequences 2. a commitment to a continuous cycle of monitoring practice, evaluating and revisiting it 3. a focus on informed judgements about practice, based on evidence 4. open-minded, responsive and inclusive attitudes 5. the capacity to reframe one’s own practice in light of reflections and insights based on research 6. dialogue with other colleagues, in-house and with external networks 7. the capacity to mediate and adapt from externally developed frameworks, making informed judgements and defending or challenging existing practice. 161 Reflective practice has also been linked to action research162 and the need for critical reflection, where practitioners question their assumptions and how their values inform practice. Using this suite of guides A 2005 joint Canadian–British study, Family-centred Service: Moving Ideas into Practice,163 says that the barriers to family-centred practice identified in the literature suggest the need for educational materials targeted at service providers, decision-makers and students about key ideas and implementation strategies.164 The authors cite evidence that such materials are most effective in raising awareness165 and increasing knowledge166 (a necessary precursor to behaviour change),167 rather than producing change directly. They investigated the impacts of a set of family-centred service fact sheets on professionals, students and families, confirming that they contributed most effectively to practice change by providing support for new knowledge communicated through more interactive and interpersonal strategies, including problem-based learning, interactive workshops and educational outreach visits (for students).168 Professionals and services should therefore consider using these guides to support professional development, reflective practice, team discussion and practice-based learning. This guide provides a conceptual framework and discussion, along with many practice examples and family stories. The sectorspecific guides provide further concrete ideas for practice in specific settings and detailed good practice scenarios (including with Aboriginal and CALD families), with accompanying ‘practice points’ colour-coded to the elements of the family-centred practice model. The organisational guide explores reflective practice and other strategies for supporting practice change in more detail. There are also many other resources available to support reflective practice and critical reflection. Australian early childhood researcher Glenda McNaughton draws on both social theory and action research to suggest six questions that professionals might use to create positive change: How have I come to do things this way? How have I come to understand things this way? Who benefits from how I do and understand this? Who is silenced in how I do and understand this? How many other ways are there to do and understand this? Which of those ways might lead to more equitable and fair ways of doing and understanding things? Next steps There is a wealth of expertise, experience and commitment to working in family-centred ways among Victorian professionals and services. It can be hard for professionals to find the time to reflect and learn from each other and the families they work with, but the evidence shows that it is well worthwhile: Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 84 We need to invest significant time in staff, and give them permission to have the time around moving their practice, and thinking about what that means. So often they’re out, doing and doing and doing. But without the time to have that reflection, and think about what they’re doing, and share their experiences, we’re not going to get anywhere. – Service manager For those wanting to read further, the sector-specific practice guides in this suite provide many concrete tips and ideas for practice, including detailed good practice scenarios drawn from the experience of professionals, young people with a disability and their families. The organisational guide will be of interest to those wanting to explore how organisations can better support family-centred practice and bring families into every aspect of their processes and practices. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 85 Endnotes 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 King, GA, Law, M, King, SM and Rosenbaum, PL 1998, ‘Parents’ and service providers’ perceptions of the familycentredness of children’s rehabilitation services’, Physical and Occupational Therapy in Pediatrics, vol. 18, no. 1, pp. 1–20. McWilliam, RA, Snyder, P, Harbin, GL, Porter, P and Munn, D 2000, ‘Professionals’ and families’ perceptions of family-centred practices in infant-toddler services’, Early Education and Development, vol. 11, no. 4, pp. 519–538. Trivette, C (unpublished) cited by Dunst, C and Moore, T, ‘Family-centred practice’ presentations at ECIA (Victoria) Seminar, 13 August 2010, referenced in Moore, T, Family-centred practice presentation handout, viewed November 2011, <www.eciavic.org.au/events/professionaldevelopment.html>. Wilson, LL and Dunst, CJ 2005, Checklist for assessing adherence to family-centered practices, CASEtools: instruments and procedures for implementing early childhood and family support practices, vol. 1, Center for the Advanced Study of Excellence in Early Childhood and Family Support Practices, Family, Infant and Preschool Program, J. Iverson Riddle Developmental Center, Morganton, North Carolina, viewed November 2011, <http://w.fippcase.org/casetools/casetools_vol1_no1.pdf>. Hollo, A 2009, Early childhood intervention practitioner competencies, ECIA (Vic) and Department of Education and Early Childhood Development (DEECD), Melbourne. DEECD 2009, Victorian early years learning and development framework, viewed November 2011, <www.education.vic.gov.au/earlylearning/eyldf/default.htm> House of Representatives Standing Committee on Family, Community, Housing and Youth 2009, Who cares…?:report on the inquiry into better support for carers, Commonwealth of Australia, pp. 183–186; National People with Disabilities and Carer Council, 2009, p. 22; and Commonwealth Department of Families and Housing, Community Services and Indigenous Affairs 2010, Occasional Paper no. 29: Effectiveness of individual funding approaches for disability support, prepared by Social Policy Research Centre and Disability Studies and Research Centre, University of New South Wales, cited in Council of Australian Governments 2011, National disability strategy, viewed November 2011, <www.facs.gov.au/sa/disability/progserv/govtint/Pages/nds.aspx> Council of Australian Governments 2011, National Disability Strategy Disability Act 2006 (Vic). Summers, JA, Marquis, J, Mannan, H, Turnbull, AP, Fleming, K, Poston, DJ, Wang, M and Kupzck, K 2007, ‘Relationship of perceived adequacy of services, family-professional partnerships, and family quality of life in early childhood service programmes’, International Journal of Disability, Development and Education, vol. 54, no. 3, pp. 319–338. Bronfenbrenner, U and Morris, P 2007, ‘The bioecological model of human development’, in W Damon and RM Lerner (Eds), Handbook of child psychology, 6th edn, Wiley, New York, pp. 793–828. Dempsey, I, Keen, D, Pennell, D, O'Reilly, J and Neilands, J 2009, ‘Parent stress, parenting competence and family-centered support to young children with an intellectual or developmental disability’, Research in Developmental Disabilities, vol. 30, pp. 558–566. Bruder, MB and Dunst, CJ 2005, ‘Personnel preparation in recommended early intervention practices: Degree of emphasis across disciplines’, Topics for Early Childhood Special Education, vol. 25, no. 1, pp. 25–33. Dunstan, E and Griffiths, S 2008, ‘Sensory strategies: practical support to empower families’, New Zealand Journal of Occupational Therapy, vol. 55, no. 1, pp. 5–13. Department of Human Services 2007, Planning for individuals – a resource kit and implementation guide for disability service providers, State Government of Victoria, Melbourne. DEECD 2010, Victorian early years learning and development framework evidence paper – practice principle 1: Family-centred practice, viewed November 2011, <www.vcaa.vic.edu.au/earlyyears/evidence.html>. Department of Education, Employment and Workplace Relations 2008, Family school partnerships framework, viewed November 2011, <www.familyschool.org.au/pdf/framework.pdf>. Moore, T and Larkin, H 2005, ‘More than my child’s disability…’: a comprehensive literature review about familycentred practice and family experiences of early childhood intervention services, Scope Victoria Ltd. Dunst, CJ, Trivette, CM and Hamby, DW 2007, ‘Meta-analysis of family-centered help-giving practices research’, Mental Retardation and Developmental Disabilities, vol. 13, pp. 370–380. Dempsey, I, Keen, D, Pennell, D, O’Reilly, J and Neilands, J 2009, ‘Parent stress, parenting competence and family-centered support to young children with an intellectual or developmental disability’, Research in Developmental Disabilities, vol. 30, no. 3, pp. 558–566. Trivette, C, Dunst, CJ and Hamby, DW 2010, ‘Influences of family-systems intervention practices on parent–child interactions and child development’, Topics in Early Childhood Special Education, vol. 30, no. 1, pp. 3–19. DEECD 2010, Victorian early years learning and development framework evidence paper – practice principle 1: family-centred practice, viewed November 2011, <www.vcaa.vic.edu.au/earlyyears/evidence.html>. Macgregor, R 2005 and Cronin, D 2008, cited in DEECD, The importance of family partnerships – evidence, viewed November 2011, <www.education.vic.gov.au/about/directions/familiesaspartners/importance/evidence.htm>. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 86 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 Yap, K and Enoki, D 1995; Epstein, J 2005; Leadbeater, C and Wong, A 2010; Izzo, CV, Weissberg, RP, Kasprow, WJ and Fendrich, M 1999; and Henderson, A and Mapp, K 2002), all cited in DEECD, The importance of family partnerships – evidence, viewed July 2011, <www.education.vic.gov.au/about/directions/familiesaspartners/importance/evidence.htm>. Association for Children with a Disability 2011, Growing together: a parents’ guide to supporting siblings of children with a disability, ACD, Melbourne. Dodd, J, Saggers, S and Wildy, H 2009, ‘Constructing the ‘ideal’ family in family-centred practice: challenges for delivery’, Disability and Society, vol. 24, no. 2, pp. 173–183. Council of Australian Governments 2011. Council of Australian Governments 2011. United Nations Convention on the Rights of the Child, viewed November 2011, <www.unicef.org/crc/>. Sanderson, H, Acraman, C and Short, A 2005, Using person centred planning and approaches with children and their families, viewed November 2011, <helensandersonassociated.co.uk>. Australian Research Centre in Sex, Health and Society (ARCSHS) 2009, Summary of the findings of sex in Australia: the Australian study of health and relationships, La Trobe University, Melbourne. Department of Human Services 2007. Sanderson et al. 2005. Victorian Health Promotion Foundation (VicHealth), Onemda VicHealth Koori Health Unit (The University of Melbourne), McCaughey Centre: VicHealth Centre for the Promotion of Mental Health and Community Wellbeing (The University of Melbourne) and the Victorian Equal Opportunity and Human Rights Commission 2009, Building on our strengths: a framework to reduce race-based discrimination and support cultural diversity in Victoria: summary report, VicHealth. National Medical and Health Research Council 2005, Cultural competency in health: a guide for policy, partnerships and participation, viewed November 2011, <www.nhmrc.gov.au/_files_nhmrc/publications>. Victorian Aboriginal Child Care Agency (VACCA) 2008, Aboriginal cultural competence framework, Department of Human Services, Melbourne. VACCA 2008. VicHealth et al. 2009. Australian Bureau of Statistics, 2006 Census. Department of Human Services 2011, Enabling choice for Aboriginal people living with disability, viewed November 2011, <www.dhs.vic.gov.au/about-the-department/documents-and-resources/reports-publications>. Department of Human Services 2011. VicHealth et al. 2009. VACCA 2008. Department of Human Services 2011. Australian Bureau of Statistics 2006, 2004-05 National Aboriginal and Torres Strait Islander Health Survey, ABS, Canberra. Department of Human Services 2011. Stopher, K and D’Antoine, H 2009, Aboriginal people with a disability: unique approaches to unique issues, prepared for the Western Australian government, viewed November 2011, <www.disability.wa.gov.au>. VACCA 2008. VACCA 2008. VACCA 2008. Tong, C and Cross, TL 2010, Cross-cultural partnerships for child abuse prevention with Native American communities, Northwest Indian Child Welfare Institute, Portland, Oregon, cited in VACCA 2008. VACCA 2008. See both NMHRC 2005, Cultural competency in health: a guide for policy, partnerships and participation, viewed November 2011, <www.nhmrc.gov.au/_files_nhmrc/publications> and Department of Human Services 2004, Culturally and linguistically diverse strategy, State Government of Victoria, Melbourne. Department of Human Services 2011. NMHRC 2005. Dunst, CJ, Trivette, CM and Hamby, DW 1995, ‘Measuring the help-giving practices of human services program practitioners’, Human Relations, vol. 49, no. 6, pp. 815–835. Dinnebeil, L and Rule, S 1994, ‘Variables that influence collaboration between parents and service coordinators’, Journal of Early Intervention, vol. 18, pp. 349–361; Hedges and Gibbs 2005. Dinnebeil, L and Rule, S 1994, ‘Variables that influence collaboration between parents and service coordinators’, Journal of Early Intervention, vol. 18, pp. 349–361; Hedges and Gibbs 2005. Moore, T 2006, ‘Parallel processes: common features of effective parenting, human services, management and government’, in ECIA (Victoria) Annual Conference, viewed November 2011, <www.eciavic.org.au>. Dunst, CJ, Boyd, K, Trivette, CM and Hamby, DW 2002, ‘Family-oriented program models and professional helping practices’, Family Relations, vol. 51, no. 3, pp. 221–229. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 87 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 Wilson, LL and Dunst, CJ 2005, Checklist for assessing adherence to family-centered practices, CASEtools: instruments and procedures for implementing early childhood and family support practices, viewed November 2011, <http://w.fippcase.org/casetools/casetools_vol1_no1.pdf>. Dunst, CJ, Boyd, K, Trivette, CM and Hamby, DW 2002, ‘Family-oriented program models and professional helping practices’, Family Relations, vol. 51, no. 3, pp. 221–229. Moore and Larkin 2005. VACCA 2008. VACCA 2008. VicHealth et al. 2009. Mikhailovich, K, Martin, S and Lawton, S 2001, ‘Lesbian and gay parents: their experiences of children's health care in Australia’, International Journal of Sex and Gender Studies, vol. 6, pp. 181–191. McNair, R 2003, ‘Lesbian health inequalities: a cultural minority issue for health professionals’, Medical Journal of Australia, vol. 178, no. 12, pp. 643–645. Kazdin, AE, Siegel, T and Bass, D 1992, ‘Cognitive-problem solving skills training and parent management training in the treatment of antisocial behavior in children’ Journal of Consulting and Clinical Psychology, vol. 60, no. 5, pp. 733–47, cited in Wade, C, Mildon, RL and Matthews, JM 2007, ‘Service delivery to parents with an intellectual disability: family-centred or professionally centred?’, Journal of Applied Research in Intellectual Disabilities, vol. 20, pp. 87–98. Tymchuk, A., Lakin, C and Luckasson, R 1999 ‘Life at the margins: intellectual, demographic, economic, and social circumstances of adults with mild cognitive limitations in an increasingly complex society’, in A Tymchuk, C Lakin and R Luckasson (Eds), A forgotten generation: the status and challenges of adults with mild cognitive impairments in American society, Paul H Brookes, Baltimore, cited in Wade et al. 2007. McConnell, D, Llewellyn, G and Ferronato, L 2002, ‘Disability and decision-making in Australian care proceedings’, International Journal of Law, Policy and the Family, vol.16, no. 2, pp. 270–299, cited in Wade et al. 2007. Wade et al. 2007. Turnbull, AP and Turnbull, HR 2000, Families, professionals and exceptionality: collaborating for empowerment, 4th edn, Merrill/Prentice Hall, Upper Saddle River, New Jersey. Guralnick, MJ 2006, ‘Family influences on early development: integrating the science of normative development, risk and disability, and intervention’, in K McCartney and D Phillips (Eds), Handbook of Early Childhood Development, Blackwell, Oxford, pp. 44–61. Turnbull and Turnbull 2000. Moore and Larkin 2005. Moore, T 2007, The nature and role of relationships in early childhood intervention services, Second Conference of the International Society on Early Intervention, Zagreb, Croatia, June 14-16, 2007, viewed November 2011, <netsvic.org.au/emplibrary/ccch/TM_ISEIConf07_Nature_role_rships.pdf>. Department of Human Services 2010, Every child every chance: best interests case practice model summary guide, State Government of Victoria, Melbourne. McWilliam, RA, Tocci, L and Harbin, GL 1998, ‘Family-centred services: service providers’ discourse and behaviour’, Topics in Early Childhood Special Education, vol. 18, no. 4, p. 206. Moore, T 2006, Parallel processes: common features of effective parenting, human services, management and government, ECIA (Vic) Annual Conference, viewed November 2011, <www.eciavic.org.au>. Guralnick 2006. Hollo, A 2009, Early childhood intervention practitioner competencies, ECIA (Vic) and Department of Education and Early Childhood Development (DEECD). Litchfield, R and MacDougall, C 2002, ‘Professional issues for physiotherapists in family-centred and communitybased settings’, Australian Journal of Physiotherapy, vol. 48, pp. 105–112. Kohn, A 1999, Punished by rewards: the trouble with gold stars, incentive plans, A's, praise, and other bribes, Houghton Mifflin Harcourt, Boston. Bandura, A (Ed.) 1995, Self-efficacy in changing societies, Cambridge University Press, Cambridge. Hollo 2009. World Health Organization, The social determinants of health, viewed November 2011, <www.who.int/social_determinants/en/>. VACCA 2008. VACCA 2008. Hollo, A 2009 and Viscardis, L 1998, ‘The family-centred approach to providing services’, Physical & Occupational Therapy in Pediatrics, vol. 18, no. 1, pp. 41–53. Hollo 2009; Viscardis 1998. Trivette, Dunst and Hamby 2010. Bandura, A (Ed.) 1995, Self-efficacy in changing societies, Cambridge University Press, Cambridge. Bandura 1995. Bandura, A 1994, Self-efficacy, cited in Ramachandran, VS (Ed.), 1994, Encyclopedia of human behavior, vol. 4, Academic Press, New York. (Reprinted in H Friedman (Ed.) 1998, Encyclopedia of mental health, Academic Press, San Diego). Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 88 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 Bandura 1994. Kohn, A 1999, Punished by rewards: the trouble with gold stars, incentive plans, A's, praise, and other bribes, Houghton Mifflin Harcourt, Boston. Moore and Larkin 2005. Popay, J 2006, ‘Where’s the evidence? The contribution of lay knowledge to reducing health inequalities’, Glasgow Centre for Population Health Seminar, viewed November 2011, <www.gcph.co.uk/assets/0000/0353/Jennie_Popay_Summary.pdf>. Miller, R 2007, Cumulative harm: a conceptual overview, Department of Human Services, Melbourne. For guidance about making a report to Child Protection or referral to Child FIRST see the following, viewed November 2011, <www.dhs.vic.gov.au/for-individuals/child,-youth-and-family-services/child-protection>. Hollo 2009. Guralnick 2006. Hollo 2009. Association for Children with a Disability 2011. VicHealth 2005, Research summary 2 - Social inclusion as a determinant of mental health & wellbeing, viewed November 2011, </www.vichealth.vic.gov.au/Publications/Social-connection.aspx?page=2>. Moore, T and Larkin, H 2005. Schulz-Krohn, W and Cara, E 2000, ‘Occupational therapy in early intervention: applying concepts from infant mental health’, American Journal of Occupational Therapy, vol. 54, no. 5, pp. 550–554. Law, M, Teplicky, R, King, S, King, G, Kertoy, M, Moning, T, Rosenbaum, P and Burke-Gaffney, J 2005, ‘Familycentred service: moving ideas into practice’, Child: Care, Health & Development, vol. 31, no. 6, pp. 633–642, citing Lawlor, MC and Mattingly, CF 1998, ‘The complexities embedded in family-centred care’, American Journal of Occupational Therapy, vol. 52, no. 4, pp. 259–267; Bruce, B, Letourneau, N, Ritchie, J, Laroque, S, Dennis, C and Elliott, M 2002, ‘A multisite study of health professionals’ perceptions and practices of family-centred care’, Journal of Family Nursing, vol. 8, pp. 408–429. Litchfield and MacDougall 2002. Hollo 2009. Harris, SR 1994, ‘Parents and caregivers’ perceptions of their children’s development’, Developmental Medicine and Child Neurology, vol. 36, pp. 918–923. Hollo 2009. Trivette, C (unpublished), cited by Dunst, C and Moore, T, ‘Family centred practice’ presentations at ECIA (Victoria) Seminar, 13 August 2010, referenced in Moore, T, Family centred practice presentation handout, viewed November 2011, <www.eciavic.org.au/events/professionaldevelopment.html>. Minke, K and Scott, M 1995, ‘Parent–professional relationships in early intervention: a qualitative study’, Topics in Early Childhood Special Education, vol. 15, pp. 335–352; vol. 7; p. 181; Murray, CJ and Mandell, MM 2009, ‘Administrators’ understanding and use of family centred practices’, Journal of Early Intervention, vol. 32, p. 17; and Turnbull, AP and Turnbull, HR 2000, ‘Families, professionals and exceptionality: collaborating for empowerment, 4th edn, Merrill/Prentice Hall, Upper Saddle River, New Jersey. King, S, Kertoy, M, King, G, Hurley, P, Rosenbaum, P and Law, M 2000, Children with disabilities in Ontario: a profile of children’s services. Part 2: Perceptions about family-centred service delivery for children with disabilities, CanChild Centre for Childhood Disability Research, Hamilton, Ontario; Litchfield, R and MacDougall, C 2002, ‘Professional issues for physiotherapists in family-centred and community-based settings’, Australian Journal of Physiotherapy, vol. 48, pp. 105–112. King et al. 2000. Baum, AC and McMurray-Schwarz, P 2004, ‘Preservice teachers’ beliefs about family involvement: Implications for teacher education’, Early Childhood Education Journal, vol. 32, no. 1, pp. 57–61; Garshalis, J and McConnell, S 1993, ‘Comparison of family needs assessed by mothers, individual professionals, and interdisciplinary teams’, Journal of Early Intervention, vol. 17, pp. 36–49; McBride, S, Brotherson, MJ, Joanning, H, Whiddon, D and Demmitt, A 1993, ‘Implementation of family-centered services: perceptions of families and professionals’, Journal of Early Intervention, vol. 17, pp. 414–430; McWilliam, RA, Maxwell, KL and Sloper, KM 1999, ‘Beyond “involvement”: Are elementary schools ready to be family-centered?’, School Psychology Review, vol. 28, pp. 378–394. King et al. 2000; Iversen, MD, Shimmel, JP, Ciacera, SL and Prabhakar, M 2003, ‘Creating a family-centered approach to early intervention services: perceptions of parents and professionals’, Pediatric Physical Therapy, vol. 15, no. 1, pp. 23–31. Buysse, V, Wesley, P, Keyes, L and Bailey, DB 1996, ‘Assessing the comfort zone of childcare teachers in serving young children with disabilities’, Journal of Early Intervention, vol. 20, pp. 189–203; Dinnebeil, L and Rule, S 1994, ‘Variables that influence collaboration between parents and service coordinators’, Journal of Early Intervention, vol. 18, pp. 349–361; Hedges, H and Gibbs, C 2005, ‘Preparation for teacher-parent partnerships: a practical experience with a family’, Journal of Early Childhood Teacher Education, vol. 26, pp. 115–126; Judge, S 1997, ‘Parental perceptions of help-giving practices and control appraisals in early intervention programs’, Topics in Early Childhood Special Education, vol. 17, pp. 457–476; Dunst, CJ and Trivette, CM 2005, Measuring and evaluating family support program quality, Winterberry Press, Ashville, NC; Krauss, M 1997, ‘Two generations of family research in early intervention’ in MJ Guralnick (Ed.), The effectiveness of early intervention, Paul H Brookes, Baltimore, pp. 611–624. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 89 121 Minke and Scott 1995. 122 Lawlor, MC and Mattingly, CF 1998, ‘The complexities embedded in family-centred care’, American Journal of Occupational Therapy, vol. 52, no. 4, pp. 259–267; Bruce, B, Letourneau, N, Ritchie, J, Laroque, S, Dennis, C and Elliott, M 2002, ‘A multisite study of health professionals’ perceptions and practices of family-centred care’, Journal of Family Nursing, vol. 8, pp. 408–429, cited in Law, M et al. 2005, ‘Family-centred service: moving ideas into practice’, Child: Care, Health & Development: vol. 31, no. 6, pp. 633–642. 123 Moore and Larkin 2005. 124 Moore and Larkin 2005. 125 Moore and Larkin 2005. 126 Harry, B 2008, ‘Collaboration with culturally and linguistically diverse families: ideal versus reality’, Exceptional Children, vol. 74, no. 3, pp. 372–388. 127 DEECD 2010, Victorian early years learning and development framework evidence paper – practice principle 4: Family centred practice, viewed November 2011, <www.vcaa.vic.edu.au/earlyyears/evidence.html>. 128 Andrews, K 2008, The family-centred approach: supporting change in children’s services, Gowrie <www.gowriemelbourne.com.au>, Melbourne. 129 Flynn, G and Nolan, B 2008, ‘What do school principals think about current school-family relationships?’, NASSP Bulletin, vol. 92, pp. 173–190, cited in Murray, CJ and Mandell, MM 2009. 130 NMHRC 2005, Cultural competency in health: a guide for policy, partnerships and participation, viewed November 2011, <www.nhmrc.gov.au/_files_nhmrc/publications>. 131 Department of Ageing Disability and Home Care 2003, Partners for managers: managers module for the partners package, Early Childhood Intervention Coordination Program, Sydney. 132 Law, M, Teplicky, R, King, S, King, G, Kertoy, M, Moning, T, Rosenbaum, P and Burke-Gaffney, J 2005, ‘Familycentred service: moving ideas into practice’, Child: Care, Health and Development, vol. 31, no. 6, pp. 633–642. 133 Law et al. 2005. 134 Wilson, LL and Dunst, CJ 2005, Checklist for assessing adherence to family-centered practices, casetools: instruments and procedures for implementing early childhood and family support practices, vol. 1, Center for the Advanced Study of Excellence in Early Childhood and Family Support Practices, Family, Infant and Preschool Program, J. Iverson Riddle Developmental Center, Morganton, North Carolina, viewed November 2011, <http://w.fippcase.org/casetools/casetools_vol1_no1.pdf>. 135 Dinnebeil, L and Rule, S 1994, ‘Variables that influence collaboration between parents and service coordinators’, Journal of Early Intervention, vol. 18, pp. 349–361; Hedges and Gibbs 2005. 136 Moore, T 2006. 137 Litchfield and MacDougall 2002. 138 Law, M, Hanna, S, King, G, Hurley, P, King, S, Kertoy, M and Rosenbaum, P 2003, ‘Factors affecting familycentred service delivery for children with disabilities’, Child: Care, Health and Development, vol. 29, no. 5, pp. 357– 366. 139 South Australian Community Health Research Unit, Flinders University of South Australia. Department of Public Health and the Australia. Department of Health and Aged Care2000, Improving health services through consumer participation: a resource guide for organisations, Commonwealth Department of Health and Aged Care. 140 South Australian Community Health Research Unit et al. 2000. 141 Ziring, PR, Brazdziunas, D, Cooley, WC, Kastner, TA, Kummer, ME, González de Pijem, L, Quint, RD, Ruppert, ES and Sandler, AD 1999, ‘Care coordination: integrating health and related systems of care for children with special health care needs’, Pediatrics, vol. 104, pp. 978–981. 142 Lindeke, LL, Leonard, BJ, Presler, B and Garwick, A 2002, Family-centered care coordination for children with special needs across multiple settings’, Journal of Pediatric Health Care, vol. 16, no. 6, pp. 290–297. 143 Shelton, TL and Stepanek, J 1994, Family-centered care for children needing specialized health and developmental services, 3rd edn, Association for the Care of Children’s Health, Bethesda, MD. 144 Victorian Health Promotion Foundation (VicHealth), Partnerships analysis tool, viewed November 2011, <www.vichealth.vic.gov.au/Publications/VicHealth-General-Publications/Partnerships-Analysis-Tool.aspx>. 145 Law et al. 2005, citing Lawlor and Mattingly 1998 and Bruce et al. 2002. 146 Litchfield and MacDougall 2002. 147 Hollo 2009. 148 Finger, M and Brand, SB 1999, ‘The concept of the “learning organisation” applied to the transformation of the public sector’, in M Easterby-Smith, L Araujo and J Burgoyne (Eds), Organisational Learning and the Learning Organisation, Sage, London. 149 Kerka, S 1995, The learning organisation: myths and realities, ERIC Clearinghouse. 150 Senge, PM, Kleiner, A and Roberts, C, Ross, RB and Smith, BJ 1994, The fifth discipline fieldbook: strategies and tools for building a learning organisation, Double Day, New York; Kerka, S 1995; Finger, M and Brand, SB 1999; Gadamer, H-G, 1979, Truth and Method, Sheed and Ward, London; and Argyris, C and Schön, D 1978, Organisational learning: a theory of action perspective, Addison Wesley, Reading, Mass.: cited in Infed, The Learning Organisation, viewed November 2011 <www.infed.org/biblio/learning-organization.htm>. 151 Trivette, C (unpublished) cited by Dunst and Moore, ‘Family-centred practice’ presentations at ECIA (Victoria) Seminar, 13 August 2010, referenced in Moore, T, Family centred practice presentation handout, viewed November 2011, <www.eciavic.org.au/events/professionaldevelopment.html>. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 90 152 King et al. 1998. 153 McWilliam et al. 2000. 154 Treloar, R 2003, Recommended practices in family-centred early childhood intervention, Early Childhood Intervention Coordination Program, Department of Ageing, Disability and Home Care, Sydney. 155 Wilson and Dunst 2005. 156 Dunst, C 2010, Family-centred practice handout, ECIA Seminar, 13 August 2010, viewed November 2011, <www.eciavic.org.au/events/professionaldevelopment.html> 157 MacNaughton, G 2005; Sylva, K et al. 2004; Siraj‐Blatchford, I et al. (2008); and Raban, B et al. 2007, all cited in DEECD (2010), Victorian early years learning and development framework evidence paper – practice principle 8: reflective practice, viewed November 2011, <www.vcaa.vic.edu.au/earlyyears/evidence.html>. 158 Kinsella, E 2009 and Ghaye, A and Ghaye, K 1998, cited in DEECD 2010. 159 Moore, T 2007, The nature and role of relationships in early childhood intervention services, Second Conference of the International Society on Early Intervention, Zagreb, Croatia, June 14–16, 2007, viewed November 2011, <netsvic.org.au/emplibrary/ccch/TM_ISEIConf07_Nature_role_rships.pdf>. 160 Gruska, McLeod and Reynolds 2005, cited in DEECD 2010. 161 Pollard, A 2002, cited in DEECD 2010. 162 McMahon, T 1999, ‘Is reflective practice synonymous with action research?’, Educational Action Research, vol. 7, no. 1, pp. 163–169. 163 Law, M, Teplicky, R, King, S, King, G, Kertoy, M, Moning, T, Rosenbaum, P and Burke-Gaffney, J 2005, ‘Familycentred service: moving ideas into practice’, Child: Care, Health & Development, vol. 31, no. 6, pp. 633–642. 164 Law et al. 2005. 165 Grimshaw, JM, Thomas, RE, MacLennan, G, Fraser, C, Ramsay, CR, Vale, L, Whitty, P, Eccles, MP, Matowe, L, Shirran, L, Wensing, M, Dijkstra, R and Donaldson, C 2004, ‘Effectiveness and efficiency of guideline dissemination and implementation strategies’, Health Technology Assessment, vol. 8, pp. 1–72. 166 Rogers, EM 1995, Diffusion of innovations, 4th edn, The Free Press, New York, cited in Law, M et al. 2005. 167 Law et al. 2005. 168 Law et al. 2005. Family-centred, person-centred: a guide for everyday practice and organisational change – FINAL TEXT 91