ttp leaflet - TTP Network
advertisement
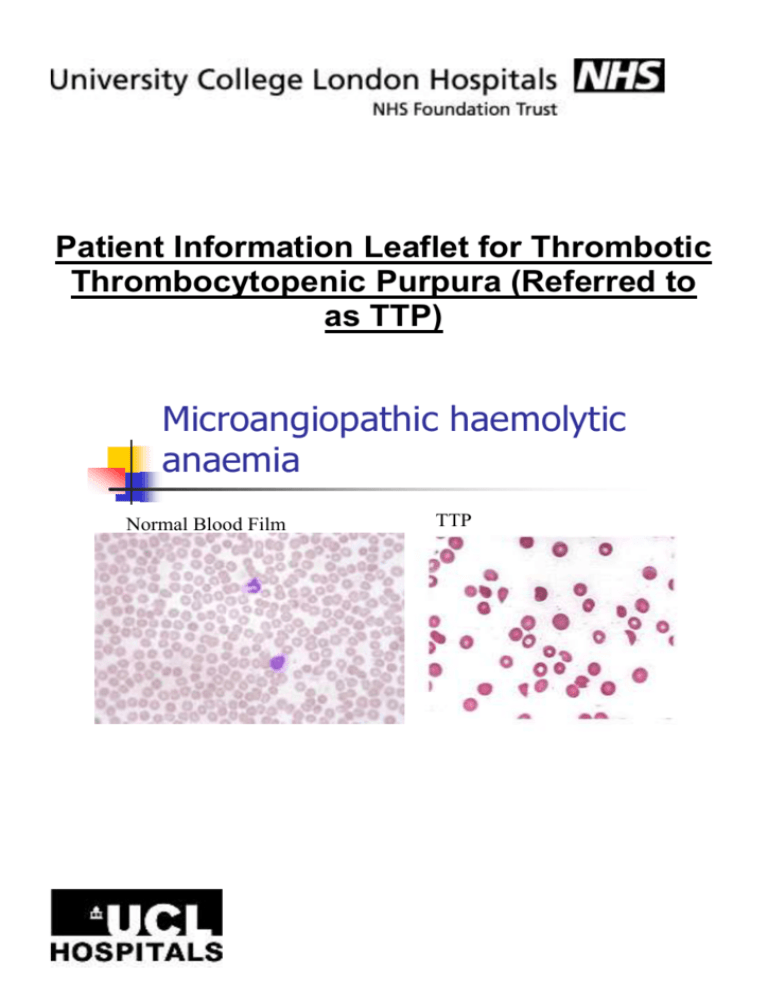
Patient Information Leaflet for Thrombotic Thrombocytopenic Purpura (Referred to as TTP) Microangiopathic haemolytic anaemia Normal Blood Film TTP What is TTP? You have been diagnosed with a condition known as TTP. It is a rare disorder of the blood coagulation system and is considered a true medical emergency. TTP is usually acquired (idiopathic or immune) and there is often no obvious cause. In some cases we can find a reason for why you have developed TTP. Rarely, we find you have congenital (familial) TTP, also known as Upshaw-Shulman syndrome. TTP affects 4-6 people per million, affecting women more than men with a peak incidence in your forties. TTP causes extensive clots (microscopic thromboses) to form in small blood vessels throughout the body (thrombotic microangiopathy). TTP is one of the microangiopathic haemolytic anaemias, and is characterised by the presence in the plasma of large von Willebrand Factor (vWF) strings. vWF is a large protein involved in blood clotting. Most cases of TTP arise from lack of an enzyme known as ADAMTS 13, which is responsible for breaking down large strings of vWF into smaller units, which then reduces the small blood vessel clots. Often the ADAMTS 13 stops working because your body makes antibodies to it. We can measure the ADAMTS 13 level when you first come into hospital, to confirm the diagnosis of TTP. We then monitor this level after you have had treatment and in the outpatients’ setting. How is TTP treated? Plasma exchange (Referred to as PEX) The plasma is the fluid part of your blood that holds all your blood cells, antibodies, nutrients, clotting factors and chemicals required for your body to function. It is a yellow colour. The PEX will remove the antibodies and replace ADAMTS 13. The procedure takes approximately 3-5 hours. Apheresis machine (Additional information leaflet: Patient Guide to Plasma Exchange at University College Hospital) Medications 1: Steroids: Intravenously / Orally. 2: A drug to protect the lining of your tummy when you are receiving the steroids: PPI e.g. Ranitidine 3: Folic Acid: to help you make red blood cells. 4: Aspirin and low molecular weight heparin when platelets >50 5: Rituximab: see leaflet Rituximab in TTP We may use other treatments during your admission, but we will explain what they are, how they work and why we need to use them. What can I expect when I am in hospital? During your hospital stay you will be treated on one of our specialist wards or the intensive care unit. PEX takes up a lot of the day as well as other treatments, such as Rituximab or blood transfusions, because your haemoglobin level may become too low. This will settle and become normal with treatment. You may also require other investigations as part of our understanding to gather as much information relating to which organs are affected and monitor them. This will include daily blood tests. The treatment will reduce once you are getting better, but sometimes, if the platelet count drops, we need to increase treatment once again. This is not unusual. If you feel unwell or there is a change in how you are feeling during your stay, please tell the nursing or medical staff looking after you. Discharge Home Each patient’s response to treatment is different, which means that the length of in-patient hospital admission varies widely. When your platelet count is over 150 and you no longer require PEX, then discharge back home is imminent. We will, however, need to monitor you closely during this time as sometimes TTP can relapse and you may need further treatment. (Additional information leaflet: Going Home after TTP) Contact Names / Numbers for the TTP Team TTP Lead Consultant: Dr Marie Scully TTP Consultant: Dr John-Paul Westwood Clinical Nurse Specialist: Siobhan Mc Guckin: 07908 175363 Out of Hours/ Urgent Medical Advice number: 07852 220900 Approved By: Dr Marie Scully, Dr JP Westwood and Siobhan Mc Guckin