polypharmacy - Sharing In Health

David LaPierre polypharmacy assignment
Mr A.C came to the family doctor's office today as a follow-up for his COPD.
He is a 75 year-old man, retired as a labourer, and living with his wife. His health is significantly affected by severe low back pain, ongoing cough, and dyspnea. He is fully independent for his ADLs and IADLs.
No memory or cognitive problems reported. His MMSE in the office was 27/30.
Past Medical History : see CGA.
His CHF, and its attending medications, had been leading to symptoms of postural hypotension, such as dizziness. Self-checks in the pharmacy while symptomatic showed readings of 85/50. He had been self-adjusting or skipping dosages until a recent change in medication by his family doctor, as discussed.
Physical Exam : Mr C appeared overweight but fit. Good colour. He was engaged throughout the interview. pulse varied from 60 to 160 and irregular during the assessment. Tachycardia was asymptomatic and transient. Blood pressure 118/72 lying, 100/70 standing. bilateral wheeze; no crackles.
JVP 2 cm ASA, no murmur, 1+ pedal edema neuro exam grossly normal normal gait; sat and stood from chair without difficulty.
Investigations (4 months ago): serum creatinine: 120 umol/L, Hgb: 116, MCV: 84, fasting glucose: 6.3
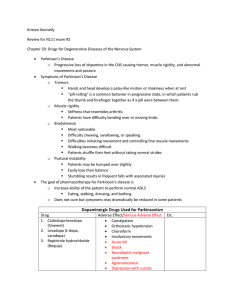
Medication Review : lisinopril (5mg BID) – His family doctor has recently halved his dose of ACE inhibitor in response to symptomatic hypotension, and this has improved his symptoms. This medication is indicated for his cardiac history and as such should be continued, but his serum creatinine should be closely monitored.
It may be advisable to trial holding his ACEi to see if his cough may be exacerbated by this drug. adverse effects : cough, hyperkalemia, renal insufficiency, angioedema, anemia, hypotension irbesartan (150 mg OD) – the combination of an ACEi and an ARB like irbesartan is increasingly contraindicated, and there does not appear to be a reason to continue with this medication, especially in light of recent postural hypotension. His family doctor should consult with the prescribing cardiologist who follows Mr. C regarding the possibility of stopping this medication. adverse effects : nausea, diarrhea, hypotension, hyperkalemia, decreased renal function furosemide (40 mg OD) – this powerful loop diuretic is prescribed for heart failure. Mr C does describe an ongoing cough, though this appears more due to his COPD than CHF, given the absence of crackles or pedal edema. Again, given the history of symptomatic hypotension, this medication should be held unless congestive symptoms re-appear. adverse effects : urinary frequency, dehydration, orthostatic hypotension, renal failure, hypokalemia, hyponatremia, gout, tinnitus.
David LaPierre polypharmacy assignment rabeprazole EC (20 mg OD) – this proton pump inhibitor is used for control of reflux, satisfactorily for
Mr C. He should consider decreasing or holding his dose, as many patient can use PPIs occasionally for symptom control without risking adverse effects. adverse effects : headache, nausea, constipation, sedation, musculoskeletal pain ezetimibe (10 mg OD): This cholesterol absorption inhibitor is prescribed after statins were stopped due to GI upset. Given Mr C's cardiac history, it is appropriate he attempt to control his cholesterol, though evidence supporting ezetimibe's impact on outcomes is scant. adverse effects : diarrhea, back pain, coughing, dizziness, fatigue, joint pain, pancreatitis, hepatitis, coagulopathy salicylic acid 3%: This is being used for Mr C's psoriasis, with good results. It should be continued adverse effects : skin irritation, rash
MS contin (30 mg OD/BID): Mr C has been taking morphine daily for over four years for his low back pain after failure of all other pain medications. It is efficacious and well-tolerated, and Mr C has reduced his dosage from QID recently. Abuse does not appear to be a concern. It should be continued. adverse effects : dependence, addiction, nausea, constipation, euphoria, sedation, dizziness, headache, anorexia, insomnia, fatigue, urinary retention tiotropium bromide (18 mcg): This anticholinergic medication is important in treating Mr C's COPD. It should be continued or even up-titrated according to symptoms. adverse effects : dry mouth, constipation, tachycardia, blurred vision, urinary retention symbicort (2 puffs BID): This combination steroid and long-acting beta2 agonist is another agent in treating Mr C's COPD. Its use as a second-line agent is balanced against known, serious risks. The poor control of Mr C's disease warrants this use. adverse effects : pneumonia, Candida, glaucoma, asthma-related death. salbutamol (2 puffs PRN, aerosolized): Mr C's COPD has recently seen him add aerosolized salbutamol to his ongoing MDI use of this short-acting bronchodilator. He requires numerous administrations during the day for symptom control. adverse effects : tremors, dizziness, anxiety, headache, insomnia, nausea
Medication omissions: If Mr C's varying heart rate is investigated to show atrial fibrillation, warfarin should be started. His hemoglobin should be re-examined, and iron should be started if ferritin is also low. Vitamin D (1000 IU) and calcium (500mg BID) should be taken to prevent osteoporosis.
David LaPierre polypharmacy assignment
Management plan: Mr C's most serious need for medication optimization is for lisinopril, irbesartan, and furosemide. The balance of hypertension and control of his CHF needs to be weighed against the significant hypotension he has experienced. The above changes should be explored, in consultation with his cardiologist.
Other steps to take include:
ECG and/or Holter monitoring to investigate potential atrial fibrillation
repeat bloodwork: CBC, glucose, creatinine, ferritin
PT or chiropractic referral to explore non-pharmacotherapeutic treatment for LBP