Falls Prevention in Residential Care
advertisement
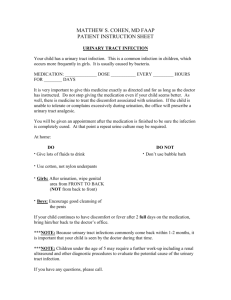
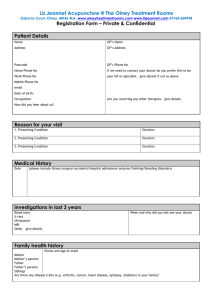
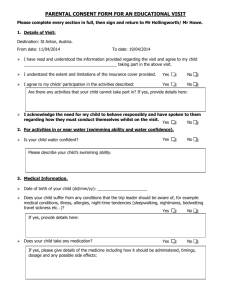
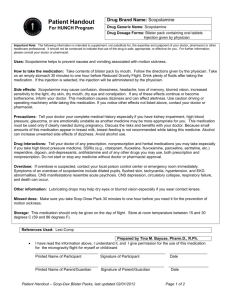
Identify potential causes of falling particularly in residential care Understand the difference between intrinsic and extrinsic risk factors. What are the implications of falling Have an action plan following a fall Heart attacks Strokes Falls 275,000 per year 130,000 per year 2,700,00 per year 500 older people a day fall in the home and require hospital treatment. Every 5 hours one older person dies as a consequence of a fall in the home 40% of Care Home admissions are as a result of a fall After a hip fracture 50% of fallers can no longer live independently 20% of older people who suffer a hip fracture as a result of a fall, die within 6 months “An unexpected event when the person 'falls' to the ground from any level, this also includes falling on the stairs and onto a piece of furniture with or without a loss of consciousness” National Institute for Clinical Excellence 2004 Physical injuries Loss of independence Psychological Social impact Carer impact Cost to services A resident falls over. What should go through your mind when thinking about why they fell? Medical Problem Syncope (Faint) Postural hypotension (B.P. Drop) Epilepsy BPPV Spinal Cord Compression Diabetes Peripheral Neuropathy (numbness of feet) Medication Medical Problem On 4 or more medicines Hypnotics Anxiolytics - diazepam;lorazepam Diuretics bendroflumethiazide; - - temezepam; zopilclone frusemide Corticosteroids –prednisolone Blood Pressure Medical Problem Medication A drop in blood pressure sufficient to cause an inadequate blood supply to the brain. A risk factor if there is more than a 20 mmHg drop in systolic pressure between lying and standing. dizziness, syncope and/or falls when: ◦ ◦ ◦ ◦ ◦ getting up quickly from lying or sitting positions standing still for any length of time getting out of a warm bath standing up after a big meal these symptoms usually ease if you lie or sit down Patient lies down for 3-4 minutes Blood pressure is recorded Patients stands – B.P. measured After one minute – measured again After 2 minutes – measured again Any history of relevant symptoms recorded Take particular care in the morning Get out of bed in stages. Avoid sudden changes in posture. Avoid sitting/standing for long periods. Raise the head of the bed Wear support stockings or tights. Medical treatments ◦ Fludrocortisone ◦ Pindolol ◦ Midodrine Blood Pressure Medical Problem Medication Urinary Tract Infection Asymptomatic Cause confusion Cause urgency Pyrexia Dipstick urine if someone falls Form from In-reach Blood Pressure Medical Problem Poor balance Medication Urinary Tract Infection Includes Maintaining a position Changing position Reaching Walking Turning Stepping up/down Chronic conditions (Stroke; Parkinsons etc) Vision (bifocals/varifocals) Alcohol Diet/ dehydration Feet Hearing Blood Pressure Medical Problem Poor balance Medication Urinary Tract Infection A trip Why do older people fall? List all the environmental risk factors you think could make an older person more likely to fall Trip Hazards Footwear Slippery Surfaces Risky Behaviour Look for the cause! Medical problem Medication Postural Hypotension UTI Balance Environmental risks Refer Doctor Doctor Do L/S B.P. Refer Doctor Dipstick – treat Keep active; exercise Remove hazards Complete when older person falls Fill in demographics Turn to back page Yes or no to risk factors Decide if action one you can do – tick when done Turn back to front and refer appropriately Send a copy to the G.P. B.&.N.E.S. G.P. All syncope Unexplained falls – 2 or more in a year Poor balance and at risk of falls Multidisciplinary team Investigations Balance Exercise Course Referral by clinician – G.P. Help the aged research http://www.helptheaged.org.uk/ Google don’t mention F word Older people don’t acknowledge the need Fear of consequences Need to concentrate on the positive I wonder why they fell?