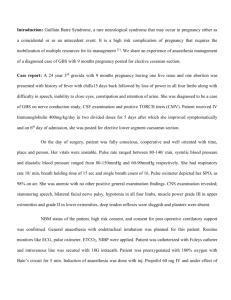
CASE REPORT: OBESE HYPERTENSIVE LADY DEVELOPING
advertisement
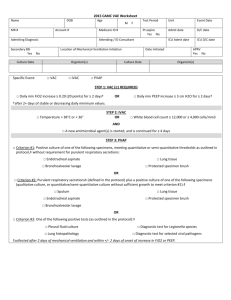
CASE REPORT: OBESE HYPERTENSIVE LADY DEVELOPING PULMONARY EDEMA POST DELIVERY, UNDER GENERAL ANESTHESIA This is the case of a 36 yr old G2A1 female, a known case of chronic hypertension superimposed with PIH, morbid obesity, who presented @ 33 POG with PPROM with failed induction for emergency LSCS. On presentation, pt’s BMI was 48 kg/m2, HR 82/min, BP 160/90 mm of Hg, RR 22/min, Pedal edema present, airway was adequate with MPCL II and a difficult venous access. Spinal anesthesia was planned as the technique of choice but failed, so general anesthesia had to be given. Patient was induced with RSII. Pt continued to have high BP intra-op, ranging from 150-180 systolic and 90-110 diastolic. Opioids, NTG and B-blockers were given intra-op to bring BP under control. Inj Pitocin 5U bolus I.V. and Inj Carboprost 250mcg I.M. were given intra-op at the request of the gynaecologist. Total i.v. fluid intra-op was 1000ml of crystalloids. There was 1 episode of desaturation intra-op to 88% which was managed by increasing FiO2 to 1. At the end of the surgery , pt was reversed and extubated. Pt developed shallow breathing, started desaturating, had b/l basal crackles on ausculatation and hence was re-intubated on ot table. There was pink frothy sputum coming out of the ETT and the airway pressures very high. Pulmonary Edema was suspected and Inj Lasix 40mg stat was given. Pt improved marginally and was shifted to ICU immediately was further management. On receiving the pt in the ICU, blood gas showed ph 7.14, PaCO2 81.7, PaO2 514.1 ( after bag ventilation with 100% oxygen). Pt was put on ventilator support. Very high pressure support and high PEEP was required to deliver the adequate tidal volume. Repeated endo-tracheal suction was required. Inj Lasix 40 mg stat, Inj Morphine 3mg was given. Pt was put on Infusion MGSO4 according to Zuspe’s regimen and on mild sedation along with antibiotics. An invasive blood pressure line was here taken because of the inaccuracies in non-invasive BP monitoring, owing to the very thick arm circumference. Pt remained stable with BP under control and minimal endo-tracheal secretions. Hence after overnight mechanical ventilation on P-SIMV mode and weaning off on CPAP/PS mode and a satisfactory blood gas report, the pt was extubated the next morning. Post-extubation, the pt remained tachypnoeic (RR – 32-40/min), most probably because of diaphragmatic splinting, because of large abdominal mass and lower abdominal surgery. After 5-6 hrs, post-extubation, pt had sudden respiratory distress wid RR – 50/min, desaturation, b/l basal crepts and loss of consciousness. Pt was immediately taken on Bains Circuit and intubated. Copious pink frothy secretions were being expressed from the ETT. ABG at this time were ph 7.06, PaO2 120, PaCO2 124. ECG was showing st segment depression in ant-lat leads. Pt was hyper-ventilated and upon return of spontaneous respiration, put on PSIMV mode Rate 25/min, PS 30, PEEP 10, FiO2 1. Inj Lasix 40mg and Inj Morphine 3 mg was given. Cardiologist’s opinion was sought, who on echocardiography gave a probable diagnosis of LV Diastolic Dysfunction with good contractility. Cardiac markers were done which were negative for Ac Coronary Event. Pt was mechanically ventilated for one day and a half and gradually pressures reduced. Presently was weaned off to CPAP mode and was tolerating well at supports of 12-14. Here, Tab Enalapril 2.5mg was added to the prescription to suppress the rennin-angiotensin-aldosterone system. On post-op day 3, pt was extubated after giving a T-Piece trial, which pt tolerated well. Pt was put on non-invasive ventilation at settings PS 14, PEEP 6, FiO2 0.4. Pt remained stable. NIV was given intermittently for 24 hrs before pt was completely taken off ventilator support. Pt was closely observed for one more day before being discharged to the ward, which was an uneventful stay.