CHAPTER 13 - Nursing Pharmacology
advertisement
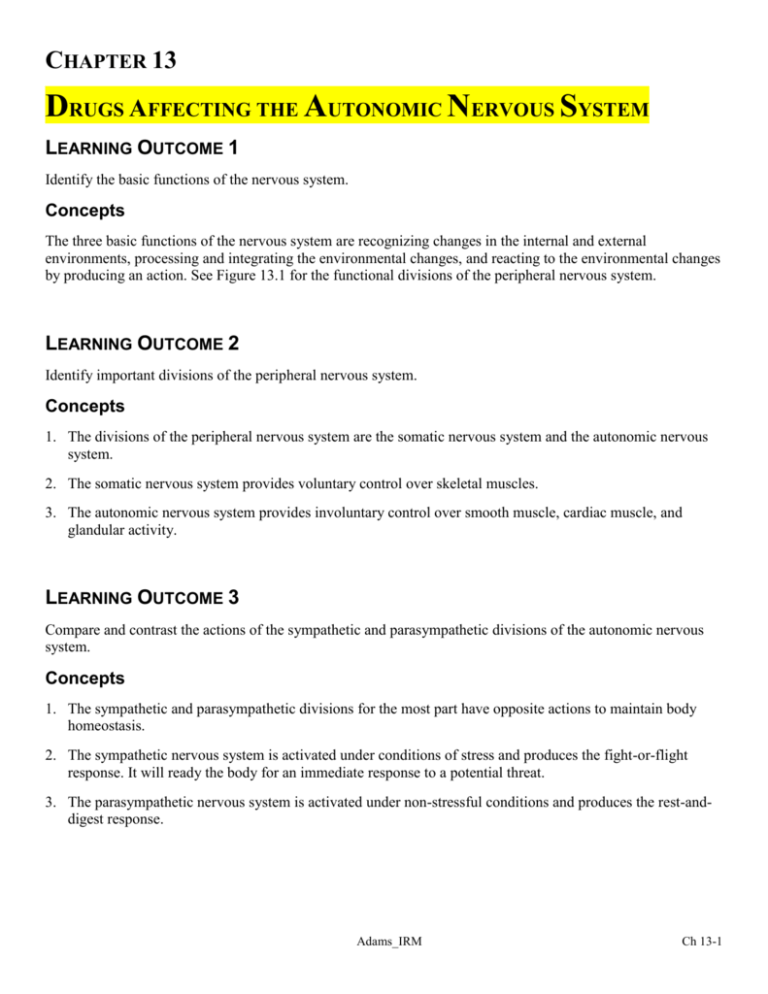
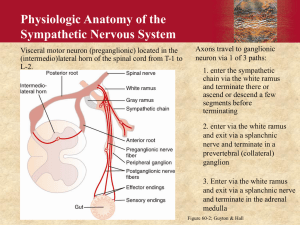
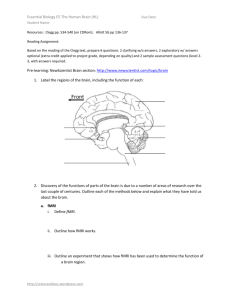
CHAPTER 13 DRUGS AFFECTING THE AUTONOMIC NERVOUS SYSTEM LEARNING OUTCOME 1 Identify the basic functions of the nervous system. Concepts The three basic functions of the nervous system are recognizing changes in the internal and external environments, processing and integrating the environmental changes, and reacting to the environmental changes by producing an action. See Figure 13.1 for the functional divisions of the peripheral nervous system. LEARNING OUTCOME 2 Identify important divisions of the peripheral nervous system. Concepts 1. The divisions of the peripheral nervous system are the somatic nervous system and the autonomic nervous system. 2. The somatic nervous system provides voluntary control over skeletal muscles. 3. The autonomic nervous system provides involuntary control over smooth muscle, cardiac muscle, and glandular activity. LEARNING OUTCOME 3 Compare and contrast the actions of the sympathetic and parasympathetic divisions of the autonomic nervous system. Concepts 1. The sympathetic and parasympathetic divisions for the most part have opposite actions to maintain body homeostasis. 2. The sympathetic nervous system is activated under conditions of stress and produces the fight-or-flight response. It will ready the body for an immediate response to a potential threat. 3. The parasympathetic nervous system is activated under non-stressful conditions and produces the rest-anddigest response. Adams_IRM Ch 13-1 LEARNING OUTCOME 4 Explain the process of synaptic transmission and the neurotransmitters important to the autonomic nervous system. Concepts 1. The synaptic transmission involves the connection of two neurons outside the CNS, in series. This connection is called the ganglionic synapse. The preganglionic neuron carries the impulse from the spinal cord to the ganglionic synapse. The postganglionic neuron carries the impulse from the ganglionic synapse to the second synapse at the target tissue. 2. The two primary neurotransmitters of the autonomic nervous system are norepinephrine (NE) and acetylcholine (Ach). In the sympathetic nervous system, norepinephrine is released at almost all postganglionic nerves and binds with adrenergic receptors, which involve the alpha- or beta-receptors on the effector organ. Acetylocholine is released by presynaptic nerves in the parasympathetic nervous system and binds with cholinergic receptors, which involve the muscarinic or nicotinic receptors. LEARNING OUTCOME 5 Compare and contrast the types of responses that occur when drugs activate alpha1-, alpha2-, beta1-, or beta2adrenergic receptors, and nicotinic or muscarinic receptors. Concepts 1. Activation of alpha1-adrenergic receptors, which are located in all sympathetic target organs except the heart, cause constriction of blood vessels and dilation of the pupils. 2. Activation of alpha2-adrenergic receptors, which are located at presynaptic adrenergic neuron terminals, inhibits the release of norepinephrine. 3. Activation of beta1-adrenergic receptors, which are located in the heart and kidneys, increase the heart rate and the force of contraction of the heart and the release of renin from the kidneys. 4. Activation of beta2-adrenergic receptors, which are located in all sympathetic target organs except the heart, inhibits smooth muscle. 5. Activation of nicotinic receptors, which are located in cell bodies of sympathetic and parasympathetic postganglionic neurons, stimulates smooth muscle and secretion of glands. 6. Activation of muscarinic receptors, which are located in parasympathetic target organs except the heart, stimulates smooth muscle and secretion from glands. Prototype Drug Ch 13-2 phenylephrine (Neo-Synephrine) Adams_IRM LEARNING OUTCOME 6 Discuss the classification and naming of autonomic drugs based on four possible actions. Concepts 1. Autonomic drugs are classified based on four possible actions that can occur in the sympathetic and parasympathetic nervous systems. 2. Drugs that stimulate the sympathetic nervous system are called adrenergic agents or sympathomimetics. 3. Drugs that inhibit the sympathetic nervous system are called adrenergic-blocking agents, adrenergic antagonists, or sympatholytics. 4. Drugs that stimulate the parasympathetic nervous system are called cholinergic agents or parasympathomimetics. 5. Drugs that inhibit the parasympathetic nervous system are called cholinergic-blocking agents, anticholinergics, parasympatholytics, or muscarinic blockers. Table 13.1 Types of Autonomic Receptors LEARNING OUTCOME 7 Describe the nurse’s role in the pharmacological management of patients receiving drugs affecting the autonomic nervous system. Concepts 1. The nurse’s role in the pharmacologic management of patients receiving any type of autonomic drug involves careful monitoring of the patient’s condition, providing education as it relates to the prescribed drug treatment, and noting adverse effects of the drug therapy. In addition, the nurse should identify the current drugs and/or herbal supplements for possible interactions or contraindications for the drug. 2. Parasympathomimetics: Monitor for adverse effects such as abdominal cramping, diarrhea, excessive salivation, difficulty breathing, and muscle cramping. Monitor liver enzymes with initiation of therapy and weekly for six weeks. Assess and monitor for appropriate self-care administration to prevent complications. Direct acting: Monitor intake and output ratio. Monitor for blurred vision. Monitor for orthostatic hypotension. Indirect acting: Monitor muscle strength and neuromuscular status, ptosis, diplopia, and chewing. Schedule medication around mealtimes. Schedule activities to avoid fatigue. Monitor for muscle weakness. 3. Anticholinergic: Monitor for signs of anticholinergic crisis. Report significant changes in heart rate, blood pressure, or the development of dysrhythmias. Provide comfort measures for dryness of mucous membranes. Minimize exposure to heat or cold or strenuous exercise. Monitor I & O. Monitor patient for abdominal distension, and auscultate for bowel sounds 4. Adrenergic Antagonist: For prostate hypertrophy, monitor urinary hesitancy/feeling of incomplete bladder emptying, interrupted urinary stream. Monitor for syncope. Monitor vital signs, level of consciousness, and mood. Monitor for dizziness, drowsiness, or light-headedness. Observe for side effects, which may include blurred vision, tinnitus, epistaxis, and edema. Monitor liver function. 5. Sympathomimetic: Closely monitor IV insertion sites for extravasation with IV administration. Monitor breathing patterns, shortness of breath, and/or audible wheezing. Observe patient’s responsiveness to light. Monitor for rhinorrhea and epistaxis. Adams_IRM Ch 13-3 Table 13.2 Adrenergic Agents (Sympathomimetics) LEARNING OUTCOME 8 For each of the drug classes listed in “Drugs at a Glance,” explain the mechanism of drug action, primary actions, and important adverse effects. Concepts 1. Adrenergic agents (sympathomimetics). The prototype drug is phenyl ephrine (Neo-Synephrine). The mechanism of action is to stimulate the sympathetic nervous system either directly, by binding to and activating adrenergic receptors, or indirectly, by causing the release of norepinephrine from the presynaptic neuron or by inhibiting the reuptake or destruction of norepinephrine. The primary use depends on which receptors are activated. The following are examples of primary actions for the different adrenergic receptors: alpha1-receptors: treatment of nasal congestion or hypotension—causes dilation of pupils during ophthalmic examinations; alpha2-receptors: treatment of hypertension; beta1-receptors: treatment of cardiac arrest, heart failure, and shock; beta2-receptors: treatment of asthma and premature-labor contractions. Adverse effects are tachycardia, hypertension, dysrhythmias, CNS excitation and seizures, dry mouth, nausea, vomiting, and anorexia. 2. Adrenergic-blocking agents. The prototype drug is prazosin (Minipress). The mechanism of action inhibits the sympathetic nervous system and produces many of the same rest-and-digest symptoms of the parasympathomimetics. The primary use is in the treatment of hypertension, dysrhythmias, angina, heart failure, benign prostatic hypertrophy, and narrow-angle glaucoma. Adverse effects are dizziness, drowsiness, headache, loss of energy and strength, palpitations, and dry mouth. 3. Cholinergic agents (parasympathomimetics). The prototype drug is bethanechol (Urecholine). The mechanism of action is to activate the parasympathetic nervous system either directly by binding to cholinergic receptors or indirectly by inhibiting the action of AchE, which prevents the destruction of endogenous Ach so it remains on the cholinergic receptors longer and prolongs its action. Primary use of the drugs is in the treatment of glaucoma, urinary retention, myasthenia gravis, and Alzheimer’s disease. Adverse effects are profuse salivation, increased muscle tone, urinary frequency, bronchoconstriction, and bradycardia. 4. Cholinergic-blocking agents. The prototype drug is atropine (Atropair, Atropisol). The mechanism of action is to inhibit the parasympathetic nervous system by competing with acetylcholine for binding muscarinic receptors. Primary uses of cholinergic-blocking agents are treatment of peptic ulcers and irritable bowel syndrome; to cause mydriasis or cycloplegia during eye examinations; to increase the heart rate in patients experiencing bradycardia; as a preanesthetic; and for treatment of asthma. Adverse effects are tachycardia, CNS stimulation, urinary retention in men with prostate disorders, dry mouth, dry eyes, decreased sweat, and photophobia. Prototype Drug Ch 13-4 prazosin (Minipress) Adams_IRM LEARNING OUTCOME 9 Use the nursing process to care for patients receiving adrenergic agents, adrenergic-blocking agents, cholinergic agents, and cholinergic-blocking agents. Concepts 1. Assessment occurs prior to administration of the drug and includes potential nursing diagnoses, reason for drug, monitoring vital signs, doing a complete health history, cautions and contraindications for drug, allergies, drug history, possible drug interactions, and evaluating lab findings. 2. Nursing diagnosis: knowledge deficient, related to drug therapy; risk for injury, related to side effect of drug therapy; disturbed sleep pattern. 3. Planning patient goals and expectation outcomes such as that the patient will exhibit a decrease in the symptoms for which the drug is being given, demonstrate an understanding of the drug’s activity, accurately describe the drug’s side effects and precautions, and demonstrate proper administration technique. 4. Implementation involves interventions—such as administration of the drug and observing for adverse effects—and patient education and discharge planning. Encourage compliance with medication regimen. Provide additional education regarding medication regimen, such as a consultation with a clinical pharmacist, written and/or visual educational material, and home-health visits to ensure patient’s ability to follow prescribed therapy. 5. Evaluation of outcome criteria includes evaluating the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning” above). Table 13.4 Cholinergic Agents (Parasympathomimetics) Prototype Drug bethanechol (Urecholine) atropine (Atro-Pen, Atropair, Atropisol) Adams_IRM Ch 13-5