Stability of buccal tablets
advertisement

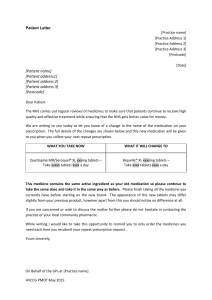
Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al FORMULATION AND EVALUATION OF BIOADHESIVE BUCCAL TABLETS OF SIMVASTATIN B. AGAIAH GOUD* AND KUMARA SWAMY SAMANTHULA* Department of Pharmaceutics, S.R.R. College of Pharmaceutical Sciences, Valbhapur, Elkathurthy, Karimnagar - 505 476, Andhra Pradesh, India. The objective of this study was to develop mucoadhesive buccal tablets of Simvastatin using mucoadhesive polymers. Simvastatin has short biological halflife (3hr), high first-pass metabolism and poor oral bioavailability (5%), hence an ideal candidate for buccal delivery system. The tablets were prepared by direct compression technique using carbopol-934, sodium carboxy methyl cellulose (Na CMC) and hydroxyl propyl methyl cellulose (HPMC) as mucoadhesive polymers. For poorly water-soluble drugs that do not show pH-dependent solubility, an approach to increase the dissolution rate is the addition of solubilizing agents or surfactants to the dissolution media. Formulations were evaluated for mass variation, hardness, friability, drug content, swelling studies, erosion studies, invivo residence time, in-vitro release studies in pH 7.0 phosphate buffer with 0.5% SDS and ex-vivo permeation studies through porcine buccal mucosa. Formulation FS5 and FH5 exhibited controlled drug release (8hr). Formulation FS5 selected as optimized formulation based on physicochemical parameters and ex-vivo permeation studies and follows zero order drug release. FTIR studies show no evidence on interaction between drug, polymers and other excipients. The results indicate that suitable bioadhesive buccal tablets for simvastatin with desired invivo residence time and controlled release could be prepared. 68 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Key words: Mucoadhesion, sodium carboxy methyl cellulose, hydroxyl propyl methyl cellulose, simvastatin, swelling index, buccal drug delivery. Introduction Oral drug administration has been one of the most suitable and widely accepted by the patients for the delivery of most therapeutically active drugs. But, due to some unsuitable physiological conditions of the gastro-intestinal tract like relatively poor absorption, presence of various digestive enzymes of the gastrointestinal tract and first pass metabolism by hepatic enzymes, the administration of some drugs is affected1,2. In recent years, delivery of therapeutic agents through various transmucosal routes has received significant attention owing to the agents that are subjected to first-pass metabolism or are unstable within the acidic environment of the gastrointestinal tract.3 Mucoadhesive formulations have been researched for delivery to the mucosa of oral (buccal, sublingual and gingival), eyes, nose, rectum and vagina4. Among these systems, the buccal mucosa offers many advantages like relatively large surface area of absorption, easy accessibility, simple delivery devices, avoiding hepatic first pass metabolism gastrointestinal degradation and feasibility of controlled drug delivery.5 Through this route it is possible to realize mucosal (local effect) and transmucosal (systemic effect) drug administration. In the first case, the aim is to achieve a site-specific release of the drug on the mucosa, whereas the second case involves drug absorption through the mucosal barrier to reach the systemic circulation. Recently much attention has been focused on the design and evaluation of buccal drug delivery systems keeping in view their potential for future market. Therefore a buccal drug delivery system needs to be developed and optimized i.e., a bioadhesive buccal drug delivery system will have to be developed which adheres to the buccal mucosa in a safe way for a 69 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al satisfactory period of time so as to release the drug to the maximum possible extent in an effective way. 6 Simvastatin is HMG Co - A reductase inhibitors widely used in the treatment of hyperlipidemias and cardiovascular diseases and it is known to have low oral bioavailability (5%) due to an extensive high first-pass effect and its availability in less dose size i.e., in few mg. Hence, it is suitable candidate for buccal drug delivery. The aim of the present study was to design and develop bioadhesive buccal tablets of simvastatin that could be applied to the buccal mucosa to release the drug unidirectionally in buccal cavity in order to decrease gastric irritation and avoid first pass effect for improvement in bioavailability, to reduce the dosing frequency and to improve patient compliance. Materials and methods Materials Simvastatin was gift sample from Aurobindo Pharma Ltd, Hyderabad, India. Carbopol 934P was obtained from S.D. Fine Chemicals, Mumbai. Sodium carboxy methyl cellulose, hydroxyl propyl methylcellulose K4M was obtained from Loba chemicals, Mumbai. Micro Crystalline Cellulose obtained from Laksmi chemicals, India. PEG 6000 obtained from India glycol Pvt Ltd., Mumbai, India. All other ingredients used in formulations were of analytical grade. Preparation of buccal tablets Buccal tablets were prepared by a direct compression method, before going to direct compression all the ingredients were screened through sieve no.100, except lubricant all the ingredients were thoroughly blended in a glass mortar with pestle for 15 min. After sufficient mixing lubricant was added and again mixed for additional 2-3 min. The mixture is 70 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al compressed using 8 mm flat faced punch on 8 stages rotary tablet compress machine (Rimek Minipress Karnavati Eng. Ltd, Ahmadabad, India). Formulation chart is given in table 1. All tablets contained MCC as filler, magnesium stearate as lubricant, butylated hydroxyl anisole, citric acid, ascorbic acid as anti oxidants and bioadhesive polymers with different mixing ratios of carbopol 934P and CMC sodium and carbopol 934P and HPMC K4M. Table 1: The tablets were prepared using carbopol 934, Sodium CMC and HPMC K4M with different ratios Formulation code FS1 FS2 FS3 FS4 FS5 FH1 FH2 FH3 FH4 FH5 CP:SCMC/CP:HPMC 5:1 3:1 2:1 1.4:1 1:1 5:1 3:1 2:1 1.4:1 1:1 Simvastatin 10 10 10 10 10 10 10 10 10 10 Carbopol-934 50 45 40 35 30 50 45 40 35 30 Na CMC 10 15 20 25 30 - - - - - HPMC K4M - - - - - 10 15 20 25 30 MCC 47 47 47 47 47 47 47 47 47 47 Magnesium stearate 02 02 02 02 02 02 02 02 02 02 02 02 02 02 02 02 02 02 02 02 Citric acid 02 02 02 02 02 02 02 02 02 02 Ascorbic acid 02 02 02 02 02 02 02 02 02 02 Total weight(mg) 125 125 125 125 125 125 125 125 125 125 Ingredients (mg) Butylated hydroxyl anisole (BHA) CP: Carbopol, Na CMC: Sodium carboxy methyl cellulose, HPMC: Hydroxy propyl methyl cellulose, MCC: Micro crystalline cellulose Drug content Ten tablets were taken and powdered; powder equivalent to one tablet was weighed accurately and allowed to dissolve in 10 ml ethanol and make up to 100 ml with distilled water on a rotary shaker overnight. After filtration through whatmann filter paper and 71 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al sufficient dilution with distilled water, samples were analyzed spectrophotometrically at 239 nm (Elico SL – 159, Hyderabad, India). This procedure was repeated thrice. Amount of drug present was determined from the standard curve of simvastatin. Swelling study Three buccal tablets were weighed individually (W1) and placed separately in 2% agar gel plates with the core facing the gel surface and incubated at 37 ± 1°C. After every 1 h time interval until 8 h, the tablet was removed from the petri dish and excess surface water was removed carefully with blotting paper. The swollen tablet was then reweighed (W2) and the swelling index (SI) were calculated using the formula given in equation (Vishnu et. al., 2007). Swelling Index = [(W2-W1) ÷ W1] × 100 Where, W1 = initial weight of the tablet W2 = final weight of the tablet Matrix erosion After swelling study, the swollen tablets were dried at 60°c for 24 h in an oven and kept in desiccator for 48 h and reweighed (W3). Matrix erosion was calculated using following formula.7 % Matrix erosion = [(W1-W3) ÷ W3] × 100 Surface pH study The surface pH of the buccal tablets was determined in order to investigate the possibility of any side effects in-vivo. As the acidic or alkaline pH may cause irritation to the buccal mucosa, the pH was maintained to neutral as closely as possible. A combined glass electrode was used for this purpose. The tablet was allowed to swell by keeping it in contact with 1 ml of distilled water (pH 6.5 ± 0.05) for 2 h at room temperature. The pH was 72 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al measured by bringing the electrode in contact with the surface of the tablet and allowing it to equilibrate for 1 min.8 In vitro drug release of buccal tablets The drug release rate from buccal tablets was studied using the USP type II dissolution test apparatus. The dissolution medium consisted of 500 mL of phosphate buffer pH 7.0. The release was performed at 37oC ± 0.5oC, with a rotation speed of 50 rpm.6 The backing layer of buccal tablet was attached to the glass slide with instant adhesive (cyanoacrylate adhesive). The slide was placed in to the bottom of the dissolution vessel. Samples (5 mL) were withdrawn at predetermined time intervals and replaced with fresh medium. The samples were filtered through filter paper and analyzed by UV spectrophotometer at 239 nm. Ex vivo permeation of buccal tablets Tissue isolation: Porcine buccal tissue from domestic pigs was obtained from a local slaughter house and used within 2 hours of slaughter. The tissue was stored in Krebs buffer pH 7.0 at 40 C after collection. The epithelium was separated from the underlying connective tissue with a surgical technique and delipidized membrane was allowed to equilibrate for approximately one hour in receptor buffer to regain lost elasticity. Study protocol: Ex vivo permeation study of simvastatin buccal tablets through the porcine buccal mucosa was performed using Franz-type diffusion cell. The freshly excised porcine buccal mucosal membrane was clamped between donor and receiver chambers of the Franztype diffusion cell, facing the mucosal side towards the donor compartment. The receiver chamber was filled with fresh pH 7.0 buffer solution and after the buccal membrane was equilibrated for 30 min 9. The buccal tablet was placed in donor chamber and 1mL of buffer 73 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al solution (pH 7.0) was added10 and the receptor compartment was maintained at 37±0.20C and continuously stirred at 50 rpm throughout the study. Aliquots (2mL) were collected at predetermined time intervals and filtered through a filter paper, and the amount of drug permeated through the buccal mucosa was then determined by measuring the absorbance at 239 nm using a UV spectrophotometer. The medium of the same volume (2mL), which was prewarmed at 37°C, was then replaced into the receiver chamber.11 The experiments were performed in triplicate (n = 3) and mean value was used to calculate the flux (J) and permeability coefficient (P). J = (dQ/dt) A P = (dQ/dt) ΔCA Where J is Flux (mg.hrs-1cm-2); P is permeability coefficient (cm/h); dQ/dt is the slope obtained from the steady state portion of the curve; ΔC, the concentration difference across the mucosa and A the area of diffusion (cm2). Due to the low permeability of drug from the formulation, permeation enhancer (PEG 6000) was added into the optimized formulation to increase the permeability. The enhancement ratio for flux was determined by dividing the cumulative amount permeated of simvastatin in the presence of PEG 6000 (Qenh) by the amount of simvastatin alone (Q control). Enhancement ratioflux=Qenh/Qcon 74 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Kinetic modeling of drug dissolution profiles The dissolution data was fitted to Zero order, First order, Higuchi and Korsmeyer Peppas to ascertain the kinetic modeling of the drug release. The method was adopted for deciding the most appropriate model.12, 13 Release kinetics: Data of in vitro release was fit into different equations to explain the release kinetics of simvastatin release from buccal tablets. The kinetic equations used were zero order and first order equations. a) Zero order release kinetics: It defines a linear relationship between the fractions of drug released verses time Q = kt Where, Q is the fraction of drug released at time t K is the zero order release rate constant A plot of the fraction of drug released against time will be linear if the release obeys zero order release kinetics. b) First order release kinetics: Wagner assuming that the exposed surface area of a formulation decreased exponentially with time during dissolution process suggested that drug release from most slow release formulation could be described adequately by apparent first order kinetics. The equation used to describe first order release kinetics is In (1-Q) = -kt Where, Q is the fraction of drug released at time t and 75 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al K is the first order release rate constant. Thus, a plot of the logarithm of the fraction of drug remained against time will be linear if the release obeys first order release kinetics. Models of drug release mechanisms: The release data of buccal tablets was fitted into different mechanism models like Higuchi, Korsemeyer – peppas and Hixson – crowel models to interpret the drug release mechanism from tablets. a) Higuchi (Diffusion) equation: It defines a linear dependence of the active fraction released per unit of surface (Q) on the square root of time. Q = kt1/2 Where, k is the release rate constant. A plot of the fraction of drug released against square root of time will be linear if the release obeys Higuchi equation. This equation describes drug release as a diffusion process based on the Fick's law, square root time dependent. b) Korsemeyer – peppas kinetics: A plot of the fraction of the logarithm of % drug released against logarithm of time will be linear if the release obeys Korsemeyer – peppas equation. Log Q = log k + n log t Where, k is the release rate constant. c) Hixson – crowel (Erosion) model: This equation defines the drug release based on formulation erosion alone. Q = 1-(1-kt)3 Where Q is the fraction of drug released at time t 76 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al K is the release rate constant Thus a plot between (1-Q)1/3 against time will be linear if the release obeys erosion equation. Determination of the ex vivo residence time The ex vivo residence time was determined using a locally modified USP disintegration apparatus.14 The disintegration medium was composed of 500 mL pH 7.0 phosphate buffer maintained at 37◦C. The porcine buccal tissue was glued to the surface of a glass slab, vertically attached to the apparatus. The buccal tablet was hydrated from one surface using 0.5 mL of phosphate buffer pH 7.0 and then the hydrated surface was brought into contact with the mucosal membrane. The glass slab was vertically fixed to the apparatus and allowed to run in such a way that the tablet was completely immersed in the buffer solution at the lowest point and was out at the highest point. The time necessary for complete erosion or detachment of the tablet from the mucosal surface was recorded. The experiments were performed in triplicate (n=3). Stability of buccal tablets Stability studies of buccal tablets were performed for optimized formulation in normal human saliva. The human saliva was collected from humans and filtered through filter paper. Buccal tablets were placed in separate petri dishes containing 5 mL of human saliva and placed in a temperature-controlled oven for 6 hr at 37°C ± 0.2°C. At regular time intervals (0, 2, 4, and 6 hr), the buccal tablets were examined for change in color, surface area and integrity.15 The experiments were repeated in triplicate (n = 3). FTIR studies to determine the drug excipients compatibility Fourier Transform Infrared (FTIR) analysis was performed to interpret the interactions of drug with polymers and other ingredients. The powder sample along with KBr was used for FTIR studies. The IR spectrum of a) pure simvastatin, b) physical mixture 77 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al containing drug, CP 934 and HPMC K4M c) physical mixture containing drug, CP 934 and SCMC d) optimized formulation were taken, interpreted and compared with each other. RESULTS AND DISCUSSION Weight variation, Thickness, Hardness, Friability and Assay: The values of weight variation, thickness, hardness, friability and assay of the twenty tablets (Table 2) were found to be within the limits of conventional oral tablets stated in the Indian Pharmacopoeia (IP, 1996). The average mass ranged from 122.8 to 128.1 mg, thick-ness of the tablets varied from 1.55 mm to 1.86 mm, hardness of the tablets was in the range 3.5 to 4 kg/cm2 the friability ranged from 0.22 to 0.51 and the drug content ranged from 95.76 in formulation FS1 to 99.16 in formulation FS5, 95.42 in formulation FH1 to 101.42 in formulation FH5. The mass, thickness, hardness, friability and assay of all compressed tablets were within the limits as per USP. 78 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Table 2: Weight variation, Thickness, Hardness, Friability and Assay (n=20) Hardness Friability Drug Content Weight variation Thickness (mg) (mm) (kg/cm2) (%) (%) FS1 124.6±0.20 1.76±0.16 3.8±0.5 0.23 97.65 FS2 126.1±0.11 1.86±0.13 4.0±0.3 0.48 96.53 FS3 125.6±0.17 1.76±0.14 3.5±0.5 0.51 95.76 FS4 128.1±0.10 1.63±0.16 3.8±0.2 0.22 98.32 FS5 127.0±0.19 1.68±0.15 4.0±0.5 0.35 99.16 FH1 123.5±0.42 1.55±0.25 3.7±0.2 0.38 97.53 FH2 124.2±0.31 1.56±0.14 3.5±0.5 0.41 101.42 FH3 122.8±0.56 1.62±0.17 3.8±0.3 0.29 97.47 FH4 124.4±0.25 1.56±0.17 4.0±0.3 0.25 98.64 FH5 126.3±0.13 1.48±0.14 3.5±0.1 0.28 95.42 Formulation Swelling and Matrix erosion studies: The bioadhesion and drug release profile are dependent upon swelling behavior of the tablets. Swelling index increased as the weight gain by the tablets increased proportionally with the rate of hydration. In swelling study, it was found that the amount of carbopol plays an important role in swelling of the matrix and leads to the drug diffusion. The fastest hydration rate was obtained from FH1 (HPMC K4M) and FS1 (Na CMC) that hydrated above 44 % within 6 hr. It was observed that swelling rate increased with an increase in carbopol polymer content of the prepared tablets. The maximum swelling was seen in the formulations FS1 and FH1. 79 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al The mucoadhesive polymers used were hygroscopic and retain large amounts of water. Tablets containing HPMC K4M as secondary polymers were found to exhibit least matrix erosion. This is because the presence of water that balanced the weight loss due to erosion and was more evident for this groups, as they showed higher hydration rates. The plots of percentage swelling index and matrix erosion are shown in [Fig 1 & 2]. 50 18 45 % Swelling 1hr 35 2hr 30 3hr 25 4hr 20 5hr 15 6hr 10 % Matrix erosion 16 40 14 12 10 Series1 8 6 4 2 5 0 0 FS1 FS2 FS3 FS4 FS5 FH1 FH2 FH3 FH4 FH5 FS1 FS2 FS3 FS4 FS5 FH1 FH2 FH3 FH4 FH5 Formulation code Formulation code Fig 1: Percentage swelling of developed buccal tablets Fig 2: Matrix erosion of developed buccal tablets Surface pH study The surface pH of all formulations was within a range of 6.2 to 7.0, close to neutral pH. These results reveal that all the formulations provide an acceptable pH in the range of salivary pH (6.6 to 7.0). They did not produce any local irritation to the mucosal route. The results of all the above mentioned tests are shown in table 3. 80 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Table 3: Surface pH values of formulations Formulation code Surface pH FS1 6.4 ± 0.31 FS2 6.6 ± 0.25 FS3 7.0 ± 0.19 FS4 6.4 ± 0.23 FS5 6.5 ± 0.24 FH1 6.5 ± 0.19 FH2 6.3 ± 0.22 FH3 6.2 ± 0.30 FH4 6.6 ± 0.21 FH5 6.8 ± 0.22 In vitro drug release of buccal tablets An ideal controlled release system should be able to release the drug immediately to attain the therapeutic level at a faster rate and maintain this drug level for a prolonged period of time.16 In vitro drug release studies revealed that the release of simvastatin from different formulations varies with characteristics and composition of matrix forming polymers as shown in graphs. The release rate of simvastatin increased with decreased carbopol 934 and increasing concentration of Na CMC and HPMC K4 M in FS5 and FH5 respectively. The most important factor affecting the rate of release from the buccal tablets is the drug: polymer ratio. Carbopol 934P is more hydrophilic and has excellent mucoadhesive, gelling properties and also helps in sustaining effect. An increase in carbopol polymer concentration causes an increase in the viscosity of the gel as well as formation of a gel layer with a longer diffusion path. Therefore decrease of carbopol content delays the drug release from tablet core. 81 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al The results indicate that as the concentration of secondary polymer increases in the respective series, Higuchi diffusion mechanism turns to zero-order release profiles. Increasing the concentration of secondary polymer in the formulations showed a sustained effect on simvastatin release. The rapidly hydrating polymer dominated in controlling the release of simvastatin from the buccal tablets, as seen from the dissolution profiles and moisture absorption data. Release rate slowed down when increasing the concentration of carbopol 934 and release rate increased with Na CMC and HPMC K4M from 1:1 to 1:3 ratios in FS and FH series. The maximum cumulative percent of drug release from formulation FS5 could be attributed to the presence of higher amount of Na CMC and lower amount of carbopol which will ionize at pH environment of the dissolution medium. This is because as the proportion of these polymers in the matrix increased, there was an increase in the amount of water uptake and proportionally greater swelling leading to a thicker gel layer. The comparison of cumulative percent drug release of all formulations was shown in Figure 3 and 4. Fig 3: Comparison of dissolution profiles of FS1 to FS5 82 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Fig 4: Comparison of dissolution profiles of FH1 to FH5 Kinetics of drug release and mechanism: To know the release mechanism and kinetics of simvastatin, the release data was fitted into mathematical models and n, r2 values for zero order, First order, Higuchi and Peppas models were represented in table 4.The peppas model is widely used, when the release mechanism is not well known or more than one type of release could be involved. The semi-empirical equation17 shown as equation: Mt/M∞ = ktn Where, Mt/M∞ is fraction of drug released at time ‘t’, k represents a constant, and n is the diffusional exponent, which characterizes the type of release mechanism during the dissolution process. For non-fickian release, the value of n falls between 0.5 and 1.0; while in case of fickian diffusion, n = 0.5; for zero-order release (case II transport), n = 1; and for super case II transport, n > 1 18 . The release exponent “n” values were less than 0.5, which indicates that the drug release from all the batches followed fickian mechanism. The higher R2 values for Zero order and Higuchi suggest that the drug release follows zero order kinetics with diffusion mechanism. 83 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Table 4: In-vitro release kinetics of the formulation Formulation zero-order First-order Higuchi R2 Korsmeyer Peppas n FS1 0.967 0.613 0.972 0.329 FS2 0.940 0.552 0.991 0.369 FS3 0.958 0.564 0.983 0.344 FS4 0.953 0.549 0.989 0.379 FS5 0.990 0.647 0.962 0.487 FH1 0.957 0.589 0.972 0.276 FH2 0.969 0.616 0.977 0.341 FH3 0.973 0.618 0.969 0.330 FH4 0.971 0.609 0.970 0.337 FH5 0.952 0.550 0.990 0.384 Ex-vivo drug permeation: Based on the in-vitro drug release, ex-vivo residence time, in-vivo residence time, swelling and matrix erosions of all formulations, the FS5 was selected for ex-vivo drug permeation studies. The oral mucosa of pigs resembles that of humans more closely than any other animal in terms of structure and composition and therefore porcine buccal mucosa was selected for drug permeation studies. The results of drug permeation from buccal tablets through the porcine buccal mucosa reveal that simvastatin was released from the formulation and permeated through the porcine buccal membrane and could possibly permeate through the human buccal membrane. The drug permeation was slow and steady (Fig 5) and 15.97±0.18% and 23.58±0.21% of simvastatin could permeate through the buccal membrane with and without enhancer (PEG 6000) in 8 hours with a flux of 0.68 mg h -1cm-2 and 1.23 mg h -1cm-2 and permeability 84 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al coefficient was 0.068 cm/ hr and 0.123 cm/ hr, respectively. The flux and permeation coefficient was increased to 0.68 to 1.23 mg h -1cm-2 and 0.068 to 0.123 cm/ hr with inclusion of permeation enhancer in the formulation. Fig 5: Ex-vivo permeation of simvastatin Determination of ex-vivo residence time The ex-vivo residence time is one of the important physical parameter of buccal mucoadhesive tablets. The ex-vivo mucoadhesive properties of the tablets were determined using porcine buccal mucosa. Formulation FH1 to FH5 showed higher retention time when compared to the formulation FS1 to FS5 as showed in table 5. As the concentration of carbopol decreased with increasing secondary polymer, the retention time decreased. This test reflects the adhesive capacity of polymers used in formulations. The results revealed that Na CMC containing formulations showed better bioadhesion than the HPMC K4M. 85 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Table 5: Ex-vivo residence time of buccal tablets Formulation Ex-vivo retention time (hr) FS1 6.33 FS2 6.16 FS3 5.75 FS4 5.33 FS5 5.25 FH1 6.50 FH2 6.33 FH3 6.25 FH4 6.16 FH5 5.75 Stability of buccal tablets Stability study was conducted only for optimized formulation (FS5). There was no change in the color and integrity of the tablets. The data obtained from the study presented in table 6. Physical properties of the simvastatin buccal tablets such as thickness and diameter slightly changed owing to swelling of the system in human saliva, buccal tablets maintained their integrity in the human saliva throughout the study, confirming the sufficient strength of the system. 86 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Table 6: Stability profile of optimized formulation in human saliva Sampling interval(hrs) Change in color Change in surface area(cm2) 0 NO NO NO 2 NO 0.5 NO 4 NO 1.3 NO 6 NO 2.1 NO 8 NO 2.8 NO Change in integrity Characterization of drug in buccal tablets FTIR spectroscopic analysis FTIR has been used to assess the interaction between drug and polymers. The FTIR spectra of all samples are shown in Figure 8. Important peaks detected in the spectrum of drug, polymers and formulations are described as follows: The spectrum of pure simvastatin presented characteristic peaks at 3433.06 cm-1 (alcoholic O-H stretching vibration), 2977.89 cm-1 (methyl and methylene C-H asymmetric and symmetric stretching vibration), 1730.03 cm-1 (lactone C=O and ester C=O stretching), 1460.01, 1382.87 cm-1 (methyl and methylene C-H bending vibration), and 1145.64 and 850.55 cm-1 (lactone and ester C-O-C bending vibration), respectively. IR analysis (fig 8) revealed that there was no strong chemical interaction occurred between drug with polymers and other ingredients used in buccal tablets. 87 d) Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al Figure 8: IR spectrum of a) Simvastatin, b) Simvastatin, carbopol and HPMC K4M, c) Simvastatin, carbopol and Na CMC and d) optimized formulation 88 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al CONCLUSION The prepared bioadhesive buccal tablets of Simvastatin can help bypass extensive hepatic first-pass metabolism and improve bioavailability. The buccal tablets showed that NaCMC containing formulations showed better bioadhesion than the HPMC K4M. The drug release rate of formulations prepared with HPMC K4M (Max.60.67%) was retarded due to the high viscosity of the polymer and formation of complex matrix network when compared to the low viscosity polymers Na CMC (Max.78.77%). Similarly, in-vitro permeation studies showed 23.58% drug release of the sustained dosage form. It can be concluded that formulation FS5 could be used to release the drug unidirectional in buccal cavity without the risk of mucosal irritation. ACKNOWLEDGEMENTS The authors wish to thanks Aurobindo Pharma Ltd, Hyderabad, India for providing simvastatin as a gift sample and also to the management of S.R.R College of Pharmaceutical science, Elkathurthy, Karimnagar for providing necessary facilities to carry out the research work. REFERENCES 1. NK Jain (2002). Oral transmucosal drug delivery, CBS publishers and distributors, New Delhi, 52-81. 2. JT McConville (2005). Recent trends in oral drug delivery. Industry overviews and deals, Drug delivery report autumn/winter, 24-26. 89 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al 3. HH Alur, SI Pather, AK Mitra, TP Johnston (1999). Transmucosal sustaineddelivery of chlorpheniramine maleate in rabbits using a novel natural mucoadhesive gum as an excipient in buccal tablets. Int J Pharm, 188:1-10. 4. E Mathiowitz, D Chickering, JS Jacob, C Santos. (1998). Bioadhesive drug delivery systems. In: E. Mathiowitz, editor. Encyclopedia of controlled drug delivery systems. New York: John Wiley and Sons, Inc.; p. 9-13. 5. J Hoogstraate , L Benes, S Burgaud (2001). Oral transmucosal drug delivery systems. In: AM Hillery, AW Lloyd, J Swarbrick , editors. Drug delivery and targeting. London: Taylor and Francis; p. 186-200. 6. M Vishnu Patel, G Bhupendra Prajapati, M Madhabhai Patel (2007). Formulation, evaluation, and comparision of bilayered and multilayered mucoadhesive buccal devices of propranolol hydrochloride. AAPS PharmSciTech, 8(1): Article 22. 7. MV Ramana, C Nagada, M Himaja (2007). Design and evaluation of mucoadhesive buccal drug delivery systems containing metoprolol tartrate. Ind J Pharm Sci, 69(4):515-18. 8. S Asha John, BPR Sathesh, Goli Divakar, K Manoj, Jangid and Kapil (2010). Development and evaluation of buccoadhesive drug delivery system for Atorvastatin calcium, Journal of Current Pharmaceutical Research, 01:31-38 9. EA Affi, MS Mahmoud, NN E1-Samaligy (2006). Increasing bioavailability of silymarin using a buccal liposomal delivery. Int J Pharma, 308:140-148. 10. Mira Becirevic-Lacan, Mario Jug (2004). Influence of hydroxypropyl-_-cyclodextrin complexation on piroxicam release from buccoadhesive tablets. Eur J Pharm Sci, 21:251–260. 90 Journal of Advanced Pharmaceutical Sciences 2011 Vol-1 Issue 1 B. Agaiah Goud et. al 11. AM Mumtaz, HS Ch'ng (1995). Design of a dissolution apparatus suitable for in situ release study of triamcinolone acetonide from bioadhesive buccal tablets. Int J Pharm, 121:129-139 12. YM Rao, YV Vishnu, K Chandrasekhar, G Ramesh (2007). Development of Mucoadhesive patches for buccal administration of Carvedilol. Current Drug Delivery, 4:27-39. 13. DM Brahmankar, SB Jaiswal (2003). biopharmaceutics and pharmacokinetics a treatise. 1st ed. Delhi: Vallabh Prakashan; 230-72. 14. F Nakamura, R Ohta, Y Machida, T Nagai (1996). In vitro and in vivo nasal mucoadhesion of soluble polymers. Int J Pharm, 134:173–181. 15. H Kashappa Goud Desai, TM Pramod Kumar (2004). Preparation and Evaluation of a Novel Buccal Adhesive System. AAPS PharmSciTech, 5(3) Article 35. 16. CR Lopez, A Portero, JL Vila-Jato, MJ Alonso (1998). Design and evaluation of chitosan/ethylcellulose mucoadhesive bilayered devices for buccal delivery. J Contrl release, 55:143-152. 17. NA Peppas, PA Buri (1985) Surface, interfacial and molecular aspects of polymer bioadhesion on soft tissues, J. Control. Release 2, 257–275. 18. V Agarwal, B Mishra (1999). Design, development, and biopharmaceutical properties of buccoadhesive compacts of pentazocine, Drug Dev. Ind. Pharm 25, 701– 709 For Correspondence: B. Agaiah Goud, Principal & Professor Dept. of Pharmaceutics SRR College Of Pharmaceutical Sciences, Valbhapur, Elkaturthy Karimnagar. 91