MMH Practical Guideline of Chronic Myeloid Leukemia
advertisement

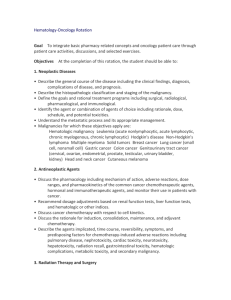
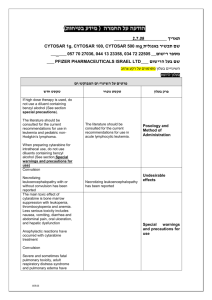
MMH Practical Guideline of Chronic Myeloid Leukemia 2004/7/7 Introduction Chronic myeloid leukemia (CML) is a clonal stem cell disorder characterized by increased proliferation of myeloid elements at all stages of differentiation. The hallmark of CML is the Philadelphia chromosome (Ph), a reciprocal translocation between the long arms of chromosomes 9 and 22 [i.e., t(9;22)], resulting chimeric BCR-ABL gene. Clinical Features Symptoms Early chronic phase may have no symptoms. Fatigue, weight loss, abdominal fullness and anorexia, easy bruising or bleeding, abdominal pain, or fever. Signs The most common finding is splenomegaly, which can be massive (in about 10% of patients, the spleen is not enlarged, even on splenic scan). Diagnosis History and physical examination CBC, platelets: Morphologic review Leukocytosis usually > 25,000/ul Myeloid cells at all stages of maturation in the peripheral smear. Chemistry profile: MAR Bone marrow aspirate and biopsy Leukocyte alkaline phosphatase (LAP) score: markedly diminished. HBsAg, Anti-HCV Ab Abdominal echo Chromosome study: Karyotypic cytogenetics for the detection of the t(9;22) 10% Ph negative: FISH or PCR 1 Staging and Prognosis Stage Chronic phase Features/Definitions <5% blasts and promyelocytes in PB or BM Accelerated phase Increasing spleen size and increasing WBC count unresponsive to therapy Blasts 10-19% of WBCs in peripheral and/or nucleated BM cells PB basophils >= 20% Persistent thrombocytopenia (< 100,000/μL) Median survival 5–6 yr <1 yr unrelated to therapy, or persistent thrombocytosis (> 1,000,000/μL) unresponsive to therapy Cytogenetic evidence of clonal evolution Blast crisis Blasts >= 20% of PB white cells or of nucleated BM cells Extramedullary blast proliferation Large foci or clusters of blasts in the BM biopsy A few months PB, peripheral blood; BM, bone marrow. Primary Treatment for Chronic Phase Imatinib mesylate (Glivec) 400mg po daily and evaluation every 3 months. Screen for allogeneic bone marrow transplantation (BMT) (HLA testing) if feasible. Hematologic remission (at least partial response): Continue imatinib mesylate. Monitor cytogenetics or FISH or PCR every 3-6 months after complete hematologic response. Not in hematologic remission, or in hematologic relapse: Increase imatinib mesylate dose (600-800mg/day, if tolerated) or interferon-α ± cytarabine or BMT if feasible or clinical trial or chemotherapy (e.g. hydroxyurea) 2 Treatment Schedule Drug Treatment plan Toxicity Response Rate Imatinib mesylate 400 mg p.o. daily, maximum 800 mg/day The major Leukopenia, anemia, thrombocytopenia, diarrhea, cytogenetic response was 87.1%. edema, fluid retention, GI upset, muscle cramps, rash. Hydroxyurea 500–2,000 mg p.o. daily (or Leukopenia common, daily dose of =< 50 mg/kg) anemia, thrombocytopenia, nausea, rash 90% hematologic remission; 34–44% 5-yr survival Interferon α-2a/b 5 × 106 Units/m2 per day s.c. Fever, myalgia, rashes, depression, leukopenia, 19% cytogenetic responses; 52–79% anemia, thrombocytopenia 5-yr survival Interferon α-2a/b + cytarabine Interferon α-2a/b, 5 × 10 Units/m2 per day s.c.; cytarabine, 20 mg/m2 s.c. single daily dose for 10 days (d 1–10; total dose/cycle = 200 mg/m2). Cytarabine cycle is repeated monthly. 6 Nausea, vomiting, diarrhea, 41% cytogenetic mucositis, weight loss, response rate; 86% leukopenia, anemia, 3-yr survival thrombocytopenia Discontinue cytarabine after complete cytogenetic response is achieved. Treatment for Blast Crisis Laboratory studies: Bone marrow exam, flow cytometry, cytochemistry (peroxidase, TdT), cytogenetics. Lymphoid: ALL-type induction chemotherapy or clinical trial. Myeloid: AML-type induction chemotherapy or clinical trial. Refractory or relapse: Allogeneic BMT (if feasible) or clinical trial. Supportive Care Strategies for Leukocytosis and Thrombocytosis Factors to consider when choosing treatment include: Patient’s age, risk factors for thromboembolic disease, and degree of thrombocytosis. Symptomatic leukocytosis: 3 e.g. dyspnea, tachypnea, rales, interstitial infiltrates, headaches, blurred vision. Treatment options include hydroxyurea, apheresis, or imatinib mesylate. Symptomatic thrombocytosis: e.g. erythromelalgia, headache, dizziness, visual and acoustic symptoms, thrombosis or hemorrhage. Treatment options include hydroxyurea, antiaggregants, anagrelide or apheresis. Criteria for Hematologic Remission Complete hematologic response Complete normalization of peripheral blood counts with leukocyte count < 10,000/μL Platelet count < 450,000/μL No immature cells, such as myelocytes, promyelocytes, or blasts in peripheral blood No signs and symptoms of disease with disappearance of palpable splenomegaly Partial hematologic response Same as complete hematologic response, except for: Presence of immature cells Platelet count < 50% of the pretreatment count, but > 450,000/μL Persistent splenomegaly, but < 50% of the pretreatment extent Criteria for Cytogenetic Remission Complete: No Ph-positive metaphases Partial: 1%-34% Ph-positive metaphases Minor: 35%-90% Ph-positive metaphases 4