Urinary Catheter Policy ()
advertisement

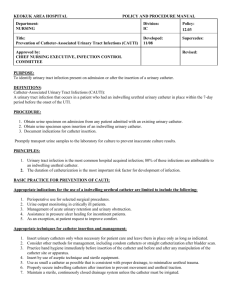
I. PURPOSE To provide guidelines for the replacement of indwelling urinary catheters and indications for urinalyses and urine cultures. II. POLICY A. B. C. III. It is best practice that indwelling catheters be removed as soon as possible and be replaced with an intermittent catheterization program or a toileting program. The need for an indwelling catheter should be re-evaluated on a daily basis. In the absence of an appropriate indication, indwelling urinary catheters should not be changed. Routine or scheduled catheter replacement is not best practice. A nurse may change an indwelling catheter without a physician’s order unless there is a physician order stating that the catheter should not be changed. PROCEDURE A. B. C. Changing Indwelling Urinary Catheters 1. An indwelling catheter will be changed when any of the following conditions exist: A. Encrustation is present on the internal lumen of the catheter. This can be determined by rolling the catheter between the thumb and index finger and palpating for gritty material B. Catheter has been contaminated with feces C. Catheter is obstructed D. Catheter is leaking E. Physician orders the catheter to be changed. 2. Indwelling urinary catheters will be changed using sterile technique by a RN or LPN. 3. If planning to change a urinary catheter, obtain a urine specimen before changing the catheter. 4. Document the indwelling urinary catheter change and any other pertinent findings in the patient’s clinical record. Urinalyses and Urine Cultures: The RN should notify the physician and obtain a urinalysis, and, if indicated, a urine culture in the following situations: 1. A patient has symptoms of UTI and the following conditions are present: A. Urine is cloudy and foul smelling B. Urine has sedimentation C. Patient has a fever of unknown origin. 2. A patient has symptoms of UTI and lower abdominal pain or back pain of unknown origin. Collecting Urine Specimens 1. Patient identity must be verified prior to collecting the specimen, using at least 2 patient identifiers. 2. If the indwelling urinary catheter is not going to be changed, the plastic drainage tubing should be clamped for a short period of time, not to exceed 30 minutes, to allow urine to collect in the tubing. 3. Perform hand hygiene with alcohol hand gel (preferred) or soap and water. 4. The port on the tubing should be cleaned vigorously with alcohol. 5. Aspirate 4 to 10 mL of urine using a sterile syringe. If a luer-lock adaptor is not present, attach a sterile needle to the syringe. 6. Place urine specimen in a sterile specimen cup. 7. Label the specimen cup immediately after collecting the urine specimen, in the presence of the patient. 8. Place the urine specimen in a plastic bag. A completed request form should accompany the specimen to the laboratory. The request form must include two unique patient identifiers that match the specimen label. 9. If the indwelling catheter is going to be changed, then 4 to 10 mL of urine should be obtained from the sterile collection bag to obtain the urine specimen. Follow steps 6 through 8 to complete the procedure for collecting urine specimens. D. Additional Information: Additional information on management of patients with urinary catheters may be found in the Basic Care Standards (Adult) policy, and in the Nurses’ Guide to Clinical Procedures. IV. UWHC CROSS REFERENCES Policy 13.12: Basic Care Standards (Adult) V. REFERENCES Smith-Temple J, Johnson JY. (2006). Nurses’ Guide To Clinical Procedures (5th ed.). Philadelphia: Lippincott Williams & Wilkins CDC: Guideline for Prevention of Catheter-associated Urinary Tract Infections Edward S. Wong, M.D. in consultation with Thomas M. Hooton, M.D. Published: February 1981; last review April 2005. Written by Gray, M. (2004). What Nursing Interventions Reduce the Risk of Symptomatic Urinary Tract Infection in the Patient With an Indwelling Catheter? Journal WOCN, 31, 3-13. Madigan, E., Felber Neff, D. (June, 2003). Care of Patients with Long-Term Indwelling Urinary Catheters. Online Journal of Issues in Nursing, retrieved December, 20, 2006. from ht tp://nursingworld.org/ojin/hirsh/topic2/tpc2_1.htm. Mercer Smith, J. (December 2003). Indwelling Catheter Management: From Habit Based to Evidence Based Practice. Ostomy and Wound Management, 49, 34-44. National Collaborating Centre for Nursing and Supportive Care. Infection control. Prevention of healthcare-associated infections in primary and community care. London (UK): National Institute for Clinical Excellence (NICE). (June, 2003). 1-23. [292 references]. Nicolle, L. E. (May 2001). The Chronic Indwelling Catheter and Urinary Infection in Long Term Care Facility Residents. Infection Control and Hospital Epidemiology, 22, 315-321. Niël-Weise, B. S. & Van den Broek, P. J. (2005). Urinary catheter policies for long-term bladder drainage. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD004201. DOI: 10.1002/14651858.CD004201.pub2. Raz, R., Schiller, D. & Nicolle, L. E. (October 2000). Chronic Indwelling Catheter Replacement Before Antimicrobial Therapy for Symptomatic Urinary Tract Infection. The Journal of Urology, 164, 1254-1258. Simpson, C. & Clark, A. P. (2005). Noscomial UTI: Are We Treating the Catheter or the Patient? Clinical Nurse Specialist, 19, 175-179. Smith, P. W., MD & Rusnak, P. G., RN. (1997). Infection prevention and control in the longterm-care facility. American Journal of Infection Control, 25, 488-512. Tambyah, P. A.,, MBBS, Knasinski, V. RN, BSN, & Maki, D. G., M.D. (2002). The Direct Costs of Noscomial Catheter-Associated Urinary Tract Infection in the Era of Managed Care. Infection Control and Hospital Epidemiology, 23, 27-31.