Comprehensive Psychiatric Evaluation
advertisement

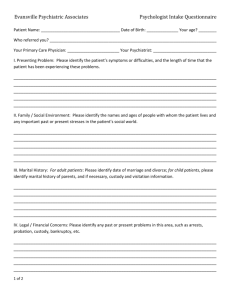
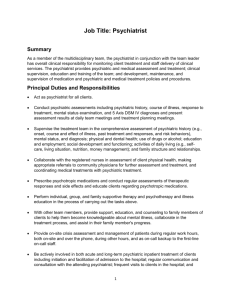
Comprehensive Psychiatric Evaluation A Guide for Parents A general, comprehensive psychiatric evaluation has as its central component a face-to-face interview with the patient. The interview-based data are integrated with data that may be obtained through other components of the evaluation, such as a review of medical records, a physical examination, diagnostic tests, and history from collateral sources. A general evaluation usually takes more than 1 hour to complete, depending on the complexity of the problem and the patient's ability and willingness to work cooperatively with the psychiatrist. Several meetings with the patient may be necessary. Evaluations of lesser scope may be appropriate when the psychiatrist is called on to address a specific, limited diagnostic or therapeutic issue. The aims of a general psychiatric evaluation are: 1) to establish a psychiatric diagnosis, 2) to collect data sufficient to permit a case formulation, and 3) to develop an initial treatment plan, with particular consideration of any immediate interventions that may be needed to ensure the patient's safety, or, if the evaluation is a reassessment of a patient in long-term treatment, to revise the plan of treatment in accord with new perspectives gained from the evaluation. Components of a comprehensive psychiatric evaluation The following are the most common components of a comprehensive, diagnostic psychiatric evaluation. However, each evaluation is different, as is each individual's symptoms and behaviors are different. Evaluation may include the following: description of behaviors present (i.e., when do the behaviors occur, how long does the behavior last, what are the conditions in which the behaviors most often occur) description of symptoms noted (physical and psychiatric symptoms) effects of behaviors/symptoms as related to the following: o work performance o school performance o relationships and interactions with others (i.e., spouse, co-workers, family members, neighbors) o family involvement o activity involvement psychiatric interview personal and family history of emotional, behavioral, or developmental disorders complete medical history, including description of the individual's overall physical health, list of any other illnesses or conditions present, and any treatments currently being administered laboratory tests, in some cases (may be used to determine if an underlying medical condition is present), including the following: o blood tests o x-rays - a diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. o educational assessments o speech and language assessments o psychological assessments _________________________________________________________ Adapted from: American Psychiatric Association, www.psych.org The University of Chicago Hospitals, www.uchospitals.edu