Cardiopulmonary Physiology
advertisement

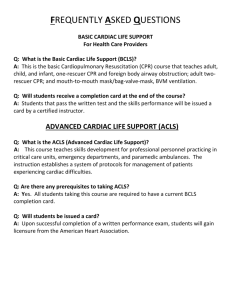
Cardiopulmonary Physiology Millersville University Dr. Larry Reinking Chapter 6 - Regulation of Cardiac Pumping Cardiac output can change from a resting value of about 6 L/min to more than 20 L/min during vigorous exercise. These changes are mediated by external factors such as circulating catecholamines and nervous input to the heart (extrinsic regulation) or by the heart itself (intrinsic regulation). The ability of the heart to regulate, without nerves, is really quite surprising. In racing greyhounds, denervation of the heart has little effect on cardiac output and results in only a 5% reduction in running performance. Cardiac output increases satisfactorily during exercise in heart transplant patients. At rest, in humans, heart performance is actually inhibited by nervous input. When both divisions of the autonomic nervous system are blocked, the heart rate in young adults increases from a resting 70 beats/min to 105 beats/min. This chapter will examine these factors that regulate cardiac pumping. Muscle Preload and Afterload The concepts of preload and afterload are important for understanding striated muscle performance. We will again refer to skeletal muscle as a basis for comparison. The following illustrates a classical skeletal muscle experiment that, perhaps, you have performed. Figure 6.1 Work Performed with Preload and Afterload in Skeletal Muscle work performed b res t pre-load a co ntraction sarcomeres point a pre-load c point b res t after-load after-load co ntraction point c load In this experiment an isolated skeletal muscle is stimulated and lifts a load. Under preload conditions, the muscle is presented with the load, and is stretched, before contracting. With after-load, the load is supported and the muscle will not be stretched prior to contraction. As seen above, skeletal muscles perform poorly when afterloaded. The shape of the preload curve is due, mainly, to the geometry of the sarcomeres. At point a, the muscle has only been slightly stretched by the preload and the sarcomeres are ‘crunched’. As a result, few cross bridges will be able to form and muscle contraction is weak. Optimal stretching and cross-bridging occurs at point b, resulting in the most forceful contraction. Further loading over stretches the sarcomeres, fewer cross-bridges form, and muscle contraction is weaker (point c). Afterloaded muscle, due to the lack of stretching, will have sub optimal cross-bridge geometry and poor contractile performance for all loads. Chapter 6 1 Cardiac muscle experiences preload and afterload conditions. Preloading occurs during diastolic filling when the ventricular walls stretch. Afterload work is encountered when the semilunar valves open and the heart encounters arterial pressure and resistance. Hypertension, elevated arterial pressure, represents additional afterload. Like skeletal muscle, cardiac muscle performs poorly when presented with a large afterload. INTRINSIC REGULATION (AUTOREGULATION) An isolated heart will regulate its cardiac output to match venous return. In other words, the heart will pump out exactly what it receives. This is referred to as intrinsic regulation of myocardial contractility. These controls can be directly related to changes in muscle fiber length (categorized as heterometric autoregulation) or to other intrinsic, length independent causes (termed homeometric autoregulation). The strength of cardiac contraction is reflected by the volume of blood ejected with each beat (the stroke volume). In an isolated heart, cardiac output is the product of the stroke volume (SV) and the heart rate (HR). CO = SV . HR Equation 6.1 Thus, intrinsic regulation can be accomplished by altering either the stroke volume, heart rate or both. Frank-Starling Law (Starling’s Law of the Heart) This principle describes the relationship between end-diastolic length of myocardial fibers and left ventricular work. Cardiac Performance Curve cardiac output left ventricular work Figure 6.2 Cardiac Performance and End-diastolic Volume s ymp. s tim. paras ympathetic s timulation end-diastolic volume rt. atrial press. or venous press. This relationship can be explained in terms of sarcomere geometry, in a fashion analogous to skeletal muscle example on the previous page. As the ventricular volume increases during diastolic filling, the muscular walls are stretched, altering the length of the myocardial sarcomeres. The length of the sarcomeres affect the ability to cross bridge, and as a consequence, the contractile ability and stroke volume change. At a low end-diastolic volume, the heart will have poor contractility (low stroke volume) due to ‘crunched’ sarcomeres. End-diastolic volume represents the preload condition for the ventricular myocardium. The major determinant of end-diastolic volume is the ‘filling pressure’ of the heart which can be measured as the right atrial pressure or by the nearly identical central venous pressure. Since these pressures are much easier to determine, they are typically used in place of enddiastolic volume. Cardiac output is directly related to the work of the heart. Using these replacement terms, the more common form of the Frank-Starling law is seen in the graph at the right of Figure 6.2. The relationship depicted in these graphs is also called the cardiac Chapter 6 2 performance curve. Note that cardiac performance (i.e., strength of contractility) can be altered by autonomic stimulation. A shift to the left indicates an increase in cardiac performance while a shift to the right is a decrease in performance. Thus, the Frank-Starling relationship is really a family of curves that depend on extrinsic input. Cardiac Preload is related to Cardiac Afterload is related to end-diastolic sarcomere length diastolic pressure end-diastolic ventricular volume vascular resistance filling pressure Stretch of Branched Myofibers A simple geometrical relationship may also contribute to the above heterometric effect as illustrated by this exaggerated drawing of ventricular myocardial fibers: Figure 6.3 Geometry of Stretched Myocardial Fibers low end-diastolic volume high end-dias tolic volume At low end-diastolic volume there is little stretch on the myofibers and they do not pull in the same direction. At higher end-diastolic volume the ventricular walls are stretched causing the branched fibers to be closer to parallel. During contraction, these fibers shorten in the same general direction and may create a more efficient contraction. Limitations of the Frank-Starling Principle The Frank-Starling law is a cornerstone of cardiology, however, it does have some short comings. Consider the following example. A fresh rat heart, when dropped into a beaker of warm saline, will ‘jet around’ in the solution like a tiny squid. The Frank-Starling principle emphasizes that ventricular filling is a function of venous pressure. However, in the case of the isolated rat heart, there is no filling pressure! The Frank-Starling law was developed using isolated hearts and probably does not may take into account all the factors at play in vivo. Actually, the heart may also act as a suction pump. At the end of systole some energy may be stored in the elastic components of the ventricular walls. During the rapid inflow period the walls rebound an suck blood into the ventricle. The anatomical arrangement of collagen and elastic fibers around the myofibers is consistent with this idea. Also the heart moves within the chest. As blood is ejected upward, during systole, the heart is forced downward (i.e., Newton’s law of motion). During diastole the heart rebounds, a motion that would augment ventricular filling. This last concept would be similar to filling a plastic bag by sweeping it through a tub of water. The Frank-Starling law best describes cardiac function in depressed hearts where the cardiac performance is low and venous pressure is high. In healthy hearts, the Frank-Starling principle is at play but other factors such as suction filling probably contribute to overall cardiac function. Heart Rate Effect Chapter 6 3 The previously described intrinsic controls alter stroke volume. The other way to regulate cardiac output, of course, is to alter heart rate. An increase in atrial filling will initiate a reflex response that causes heart rate to increase as much as 75%. Part of this response is due to stretching of the SA node which, in turn, can cause the rate of pacemaker firing to increase by up to 15%. The remainder of this response is due to vagal signals, from the atria to the brain, and the activation of sympathetic input to the heart. This portion of the heart rate response is called the Bainbridge reflex and is, actually, an extrinsic type control. Also, the stretching of the atria releases peptide hormones into the circulation (more on this in later chapters). Rate Induced Regulation The previous control dealt with heart rate as a response. However, a change in heart rate will induce a change in the force of contractility. In an experimental situation, a strip of ventricular muscle will increase its force of contraction when the rate of stimulation increases (for skeletal muscle this called the staircase effect or Treppe). This response appears to be caused by an accumulation of intracellular calcium, which as we saw in Chapter 4, increases cross-bridging and the force of contraction. This length independent control is a type of homeometric autoregulation. EXTRINSIC REGULATION As shown previously, the Frank-Starling relationship is modified by the parasympathetic and sympathetic divisions of the autonomic nervous system. This autonomic input originates from the medulla oblongata and is the result of the processing of signals from a variety of systemic regulatory mechanisms. At rest, parasympathetic influences predominate over sympathetic effects. Parasympathetic Input Parasympathetic input to the heart is primarily to the nodal tissue via the right and left vagus nerves. Thus, the primary effects of parasympathetic stimulation will be on heart rate (chronotropic effect). The right vagus principally innervates the SA node, while the left vagus primarily supplies the AV node. Acetylcholine, the parasympathetic neurotransmitter, slows the rate of pacemaker firing and slows conduction through the AV node (see chapter 4 for mechanism). Thus, we can say that parasympathetic input induces bradycardia or has negative chronotropic effect. Secondary effects (all inhibitory) include decreased contractile strength, depressed myocardial metabolism and, possibly, coronary artery constriction. Acetylcholine’s affect on the heart is mediated by muscarinic type cholinergic receptors and is blocked by atropine . Cardiac nodal tissue has a high levels of cholinesterases and, therefore, the effects of parasympathetic stimulation are short lived. Sympathetic Input Sympathetic nerves to the heart originates from several thoracic and one or two cervical segments of the spinal cord. Both the myocardium and nodal tissue are innervated by these fibers. In many species, the left and right sides of the sympathetic chains differentially innervate the working myocardium or the nodal tissue. This also probably true in humans. In addition to norepinephrine released by the nerve endings, the heart will also be influenced by circulating epinephrine. The adrenergic receptors are principally of the 1 type (i.e., isoproterenol is more active than norepinephrine or epinephrine) and are inhibited by beta blockers such as propranolol and atenolol. Degradation of catecholamines is limited in heart tissue and therefore the effects of Chapter 6 4 sympathetic stimulation decay rather slowly. The main cardiac effects of catecholamines are increased contractility (positive inotropic effect) and increased heart rate (tachycardia or a positive chronotropic effect). Secondary effects include an increased myocardial metabolism and, possibly, dilation of the coronary arteries. Table 6.1 Summary of Autonomic Effects on the Heart Parameter Nervous input Neurotransmitter Receptor Antagonist Agonist Persistence of effect Heart rate effect Contractility effect Myocardial metabolism Coronary arteries Parasympathetic Sympathetic vagus nerves sympathetic chains acetylcholine norepinephrine (+ circulating epi) muscarinic 1 adrenergic atropine propranolol, other 1 blockers muscarine isoproterenol > epi = norepi decays rapidly decays slowly negative chronotropic (1°) positive chronotropic (1°) negative inotropic (2°) positive inotropic (1°) depressed (2°) elevated (2°) constriction (2°) ?? dilation (2°) ?? 1° = primary effect 2° = secondary effect cardiac output Limit of Heart Rate Effect on Cardiac Output As stated previously, cardiac output increases with beating frequency for an isolated heart. This relationship, however, will apply only over a limited range: Figure 6.4 Heart Rate and Cardiac Output heart rate At lower heart rates this relation holds, however, at higher heart rates the cardiac output plateaus and then declines. A rapid heart rate is accompanied by a shortened cardiac cycle and a shortened period of diastolic filling. As we saw above, less filling results in a decreased contractility. In humans, the peak for this type of curve occurs in the range of 130-170 beats/min. Above 170 beats/min ventricular filling is severely compromised and cardiac output drops. In an intact human, other factors such as changes in peripheral resistance will complicate this relationship. CARDIAC OUTPUT AND VENOUS RETURN Chapter 6 5 During the discussion of the Frank-Starling law, we examined the effect of venous pressure on cardiac output. Now we will examine the converse; the effect of cardiac output on venous pressure. Cardiac output alters venous pressure because as the heart pumps, the recoiling ventricles ‘draw’ on the venous supply. If we were interested in the effect of cardiac output on arterial pressure we could simply refer to an equation from Chapter 3 (Equation 3.11): Pa = (CO . RT)+Pv. It would seem logical that we could rearrange this equation for venous pressure (Pv). This is not a valid approach because of the compliant nature of the venous circulation. Veins are nearly twenty times more compliant than arteries and readily collapse when pressure drops below zero. Thus, as cardiac output increases, the ventricles ‘draw’ more from the veins, venous pressure drops and, at sometime, the veins collapse so that no further rise in cardiac output can occur: Figure 6.5 Effect of Cardiac Output on Venous Pressure The relationship shown above is called the vascular performance curve. Another concept, the mean circulatory pressure is useful in our analysis. Mean Circulatory pressure (Pmc) is the residual pressure that can be measured in the circulatory system when cardiac output is zero. In other words, this is the pressure in the vessels if the heart stops. The value for Pmc is about 7 mm Hg. Combining mean circulatory pressure with arterial compliance (Ca) and venous compliance (Cv) gives us an equation for the relationship shown by the vascular performance curve. Equation 6.2 R C CO Pv = Pmc - T a Ca + Cv If this concept is combined with the cardiac performance curve (i.e., Frank-Starling relationship), we now have a powerful tool for understanding cardiac performance in an intact individual: Chapter 6 6 cardiac output cardiac performance curve Figure 6.6 'equilibrium point' Combined Cardiac Performance and Vascular Performance Curves vas cular performance curve Pmc 0 7 Pmc = mean circulatory pressure venous pressure In Figure 6.6, 'equilibrium point' represents the actual value for cardiac output and venous pressure (about 6 l/min and 2 mm Hg in young adults). This equilibrium point is a balancing act between the cardiac performance curve and the vascular performance curve. If cardiac output increases, venous pressure decreases, cardiac output then drops, venous pressure increases, .. etc. Alterations of Performance Curves The combined cardiac and vascular performance curves are helpful for predicting changes in cardiac output, venous pressure during pathophysiological situations. please consult graphs in lecture handout packet 1. Vascular Volume Changes - An increase in vascular volume (as might occur with an accidental over infusion or during 'fluid forcing' in a trauma unit) causes the vascular performance curve to shift to the right. As a result there will be a new equilibrium point and the final result is increased cardiac output, increased venous pressure and increased mean circulatory pressure. Increased vascular volume is also called hypervolemia. A decrease in blood volume, hypovolemia (as might occur with blood loss or dehydration), causes a shift of the vascular performance curve to the left. Cardiac output, venous pressure and mean circulatory pressure will all decline. 2. Cardiac Failure - Cardiac failure is reflected in a shift of the cardiac performance curve to the right. Initially, there will be a drop in cardiac output and rise in venous pressure. Cardiac failure, however, will produce renal insufficiency and, therefore, fluid retention. As a result, the vascular performance curve shift to the right. The final equilibrium point shows a large increase in venous pressure, an increased mean circulatory pressure but little change in cardiac output. 3. Increased Cardiac Performance - A hyperdynamic heart (as during exercise or the result of a cardiotonic drug) will have a vascular performance curve shifted to the left. In strenuous exercise there may also be a significant changes in the vascular performance curve due to vasodilation. 4. Changes in Vascular Resistance - Resistance changes alter the slope of the vascular performance curve, mean circulatory pressure does not change. Vasodilation causes an upward shift to the slope with the end results of increased cardiac output and increased venous pressure. The changes for vasoconstriction via sympathetic stimulation cause the opposite changes. Chapter 6 7 Vasoconstriction, however, will cause a severe after-load and a secondary shift in the cardiac performance curve to the right. Cardiac Output, Venous Return and Respiratory Activity Since they share a common space with the lungs, the heart and great vessels are under the influence of negative thoracic pressures. Negative pressure in the thorax is a few mm Hg but can become many times this during forced inspiration. These pressure changes associated with breathing will alter venous return to the ventricles. During normal breathing, thoracic pressure drops during inspiration causing an expansion of the vein cava and an increased venous return to the right heart. At the same time however, the dropping thoracic pressure causes an expansion of the vessels in the lung, momentary pooling occurs and left cardiac stroke volume drops. Thus, there is a slight variation in cardiac output in synchrony with breathing. Pulsus paradoxus is an alternating strong and weak pulse at the radial artery. It is reflection of the above alternating stoke volume. This alternation of pulse is very minor in healthy individuals but can become pronounced in some situations such as cardiac tamponade (compression of the heart by fluid in the pericardial space or by a restrictive pericardium). Valsalva maneuver is the forced expiration against a closed glottis. This maneuver will increase thoracic pressure and hinder venous return. Positive pressure ventilation also increases thoracic pressure, compresses veins and diminishes cardiac return. Chapter 6 8