Sickle Cell and Thalassaemia: A Guide to School Policy
advertisement

Sickle Cell and
Thalassaemia:
Health and Safety
A Guide to School Policy
This work is licensed under Creative Commons. Except for the ERSC logo on the final page, it may
be freely used and distributed provided original authorship is acknowledged. It may be adapted
for re-use, provided the resultant work is shared back with the sickle cell and thalassaemia
communities by offering the revised material to the Sickle Cell Open: Online Topics and Education
Resources (SCOOTER) project at www.sicklecellanaemia.org.
Simon Dyson
Unit for the Social Study of Thalassaemia and Sickle Cell,
De Montfort University,
Leicester, United Kingdom
sdyson@dmu.ac.uk
We would like to thank the following for their critical appraisal of earlier drafts of this policy
leaflet:
• Professor Elizabeth Anionwu, CBE, Emeritus Professor of Nursing, University of West London.
• Suzi Crawford, Specialist Nurse Counsellor, Soho Health Centre, Birmingham.
• Dr Paul Telfer, Senior Lecturer in Haematology at Queen Mary, University of London , and
Honorary Consultant Haematologist at St Bartholomew's and The Royal London NHS Trusts.
2
Health and Safety in Schools
This booklet has been produced based on research examining the experiences of young people with
sickle cell disorder in schools in England. An important part of school inclusiveness is recognising the
importance of offering care to young people with long-standing illness, particularly since a major
part of childhood is spent in attending school. The 1974 Health & Safety at Work Act places a duty
upon education employers to ensure the health and safety of pupils. Part of this responsibility is to
have a health and safety policy that includes supporting pupils with medical conditions. Pupils with
sickle cell disorder or beta-thalassaemia major come under this legislation and guidance.
What is Sickle Cell Disorder (SCD)?
Sickle cell disorder (SCD) is a collective name for a series of serious inherited chronic conditions that
can affect all systems of the body. It is one of the most common genetic conditions in the world and
affects around 1 in 2,000 of all babies born in England1. These sickle cell disorders are associated
with episodes of severe pain called sickle cell painful crises. People with sickle cell disorder have a
type of haemoglobin (called haemoglobin S (HbS) or sickle haemoglobin) which differs from normal
adult haemoglobin (haemoglobin A or HbA). This can cause red blood cells to change shape and
become blocked in the blood vessels, causing acute pain. Many systems of the body can be affected
meaning that different key organs can be damaged and many different symptoms can occur in many
different parts of the body. The main types of sickle cell disorder are sickle cell anaemia,
haemoglobin SC disease and sickle beta-thalassaemia. Despite its name sickle beta-thalassaemia is a
sickle cell disorder and is distinct from beta-thalassaemia major described below.
What is Beta-Thalassaemia Major?
Beta-thalassaemia major is a serious inherited blood condition in which the red blood cells are
nearly empty of haemoglobin, the key part of the blood that carries oxygen around the body. The
first life-saving step of treatment involves having blood transfusions every 3-4 weeks for the rest of
their lives. This extra blood introduces extra iron into the body that the body cannot get rid of easily.
The second step of treatment involves drugs that get rid of the excess iron. Depending upon the
individual’s suitability for particular drugs some may take these orally, either by tablet or in a drink,
whilst others may have to have injections that are delivered slowly over 10-12 hours, 5-7 days a
week. Some young people with SCD, identified by screening as being at high risk of a stroke, may
also be on regular blood transfusions and drugs or injections to reduce iron in the body. For both
thalassaemia major and SCD attendance at regular hospital outpatient clinics, attendance for regular
blood transfusions and attendance for treatment may all impact on school attendance.
How can the symptoms of sickle cell disorders (SCD) be prevented?
Certain factors have been identified as more likely to precipitate a painful sickle cell crisis. These
include infections, cold and/or damp conditions, pollution, dehydration, strenuous exertion, stress,
sudden changes in temperature, alcohol, caffeine, and smoking. Advice to people living with a sickle
cell disorder on preventing crises includes keeping warm, eating healthily, taking moderate exercise,
taking plenty of fluids, seeking medical advice if they have a fever, avoiding smoking and alcohol,
keeping up to date with medications and vaccinations, and trying to live a stress free life.
1 Streetly, A., Latinovic, R., and Henthorn, J. (2010) Positive Screening and carrier results for the England-wide universal
newborn sickle cell screening programme by ethnicity and area for 2005-7, Journal of Clinical Pathology, 63: 626-629
3
Preventive measures to support people with SCD or beta-thalassaemia major
Since those with SCD or thalassaemia are ill-suited to hard manual work, it becomes doubly
important for those with SCD or thalassaemia to receive a good education and sound careers advice.
School absences: If schools/colleges do not have strong supportive frameworks on sickle cell disorder
to reduce school absences, then studies have suggested that a pupil with SCD could miss weeks of
schooling a year, most often in short absences of 2-3 days at a time. Most pupils with SCD do not feel
supported by schools in catching up these absences. A minority have absences at or beyond levels
defined by government as persistently absent. It is important such pupils are not mislabeled by
education welfare officers as truant and their parents pressured to account for themselves if such
absences are the result of serious episodes of illness.
Good Practice: School Absences
One school has a policy of regular twilight catch-up sessions after school. This learning centre is
staffed on a rota basis so that pupils who have missed a lesson for any reason can be helped to catch
up in the presence of teachers. This not only helps the young person with sickle cell disorder catch
up, but it does so without drawing attention to them as different from other pupils.
Water: Young people with SCD need to be well hydrated to reduce the likelihood of becoming ill.
Have a ready supply of fresh drinking water available. Do not restrict drinking water in class. Ensure
water fountains are working and kept in the highest state of cleanliness so young people with SCD
are not put off using them and risk of infection is kept to a minimum.
Using the Toilet: People with SCD cannot concentrate urine as readily. They produce large quantities
of dilute urine and need to go to the toilet more often. Do not restrict toilet breaks for children.
Good Practice: Using the Toilet
One school has instituted a system of issuing the young person with a laminated card stating that the
young person has the right to excuse themselves during lesson in order to go to the toilet.
Tiredness: The person with SCD may experience severe anaemia. This may mean they feel tired,
lethargic and unable to concentrate. They may feel tired to the point where they feel they need to
sleep. Young people with beta-thalassaemia major are likely to be tired towards the end of their 4
week cycle of transfusions. It is important that teachers do not mistake serious medical symptoms of
SCD or beta-thalassaemia major for laziness. Climbing several flights of stairs several times per day to
get to and from the classroom is physically demanding for some young people with SCD. In some
cases issuing a personal lift pass may be appropriate.
Physical Exercise: Avoid hard, physical exercise involving strenuous exertion that could precipitate a
sickle cell crisis. Encourage moderate exercise. Listen to the young person who will come to know
their own safe limits of physical activity. For SCD or beta-thalassaemia major do not refuse requests if
a young person asks to be excused or stop activity because of tiredness or pain. For children with
SCD, cold or wet weather, or exposure of the skin to cooling wind may all be a trigger to episodes of
illness. Obligatory sports and gym sessions out of doors in cold and wet weather is a potent
stimulant to crisis for some children. It is important to listen to the child and parent, and follow
advice from their specialist medical teams about this.
4
Good Practice: Swimming
Young people with SCD are advised not to become cold. This may happen when swimming in
unheated pools or by delays in drying off afterwards. It is always important to listen to the views of
parents and the young person about inclusion in activities such as swimming. One school made an
arrangement with their local swimming pool to have the pool temperature increased when the class
with the child with SCD was due to take part in a swimming session. This ensured inclusion of the
young person in a valued school activity without making the young person feel separate from peers.
Infection: Young people with SCD and thalassaemia may have a damaged or missing spleen (the
organ that helps to fight infections). Enable safe storage and dispensing of any antibiotic drugs
prescribed for the young person with sickle cell disorder or thalassaemia.
Temperature: Avoid activities that require outdoor work in cold or damp conditions; avoid underheating of classrooms, especially mobile classrooms; maintain good ventilation of study areas. Allow
coats to be worn in class, and permit the child with SCD to stay inside at break in cold or wet and
windy weather.
Good Practice: Temperature
Young people with SCD may become ill if they are too hot or too cold. Schools should work with the
young person to establish agreed warmer clothing for indoor use within school. They should not be
made to go outside in cold or rainy or windy weather during breaks. Staff supervising breaks, such as
assistants or dinner staff, should be instructed not to enforce this. One school was aware that its
complement of rooms included mobile classrooms that readily became too hot or too cold. It used its
timetabling system to ensure that classes with a child with sickle cell disorder were timetabled away
from such unsuitable classrooms. This kept the young person with SCD safe, but did so without
drawing attention to him as different from others.
Individual Health Care Plans: All children with SCD or beta-thalassaemia major should have
individual health care plans, which should be reviewed yearly. As both SCD and beta-thalassaemia
major have numerous possible complications affecting many systems of the body, it is important,
where possible, to include a specialist sickle cell or thalassaemia nurse in drawing up this plan.
Good Practice: Individual Health Care Plans
All young people with a medical condition at school should have an individual health care plan2. One
local area works with the local specialist sickle cell nurse counselor, as well as the school nurse, the
parents and the young person themselves, to draw up these plans. The plans are individual but cover
as a minimum: preventive measures to keep the child well at school; arrangements for giving pain
medication to the child; what constitutes an emergency and what to do; key contacts, especially the
consultant who will be the key health professional caring for the child; and a list of school staff
(including school secretaries, canteen staff, caretakers, not just teachers) who have attended a
professional update on sickle cell/thalassaemia). The plan is reviewed each year and the list of staff
who have received an update checked against those the young person is likely to meet during their
academic year.
2
Department for Education and Skills (2005) Managing Medicine in Schools and Early Years Settings
5
Medical Issues and Medical Emergencies for Sickle Cell Disorders
Acute chest syndrome: Signs include chest pain, coughing, difficulty breathing, and fever. It can
appear to be similar to flu like symptoms. However, it is important to see a consultant ASAP.
Aplastic crisis: This is when the bone marrow temporarily slows its production of red blood cells,
usually due to infection with a virus called ParvovirusB19. This results in a severe drop in the red cell
count and severe anaemia. Signs include paleness, fatigue, and rapid pulse.
Fever: Children with sickle cell disorder are at increased risk for certain bacterial infections. A fever
of 101° Fahrenheit (38° Celsius) or higher, could signal an infection. Children with sickle cell
disorder and fever should be seen by a consultant without delay.
Hand-foot syndrome (also called dactylitis): Painful swelling of the hands and feet, plus fever. It is
most likely to occur in children under five. It is important nursery and pre-school staff are aware of
this to avoid false accusations of non-accidental injury.
Painful crises: These may occur in any part of the body and may be brought on by cold or heat or
dehydration. The pain may last a few hours or up to 2 weeks or even longer, and may be so severe
that a child needs to be hospitalized. It is important to listen to the young person who will come to
know whether the pain is mild or moderate and will pass (where schools can promote school
inclusion by permitting rest and re-integration into school later that day) or whether they need to go
to hospital.
Splenic sequestration crisis: The spleen becomes enlarged by trapping the sickle shaped red blood
cells. This leads to fewer cells in the general circulation. Early signs include paleness, weakness, an
enlarged spleen, and pain in the abdomen. It is important that nursery and pre-school staff are
aware of this life-threatening event, as it is more likely in younger children.
Strokes: The higher risk is in children aged 2-10 years. Apply the FAST approach:
Facial weakness: can the person smile, or has their mouth or eye drooped?
Arm: can the young person raise both their arms above shoulder height?
Speech problems: can the person speak clearly and understand what you say?
Time: to dial the emergency number for an ambulance.
It can be difficult to differentiate the symptoms of stroke from those of a sickle crisis, where pain can
result in restriction of movement. Children with SCD have a Transcranial Doppler Scan yearly from
age 2 to assess risk of stroke.
Silent Strokes: Changes in a young person’s behaviour or concentration or a sudden deterioration in
the quality of their school work could be due to several reasons. In up to a fifth of young people with
sickle cell disorders, small areas of brain damage are evident on a sensitive brain scan (MRI scan)
resulting from impaired blood supply. It is important to liaise with the young person’s medical
consultant in order to investigate if such changed behaviour is owing to a silent stroke.
Priapism: An unwanted painful erection of the penis, unrelated to thoughts about sex. Urgent
medical help should be sought if it lasts more than two hours.
6
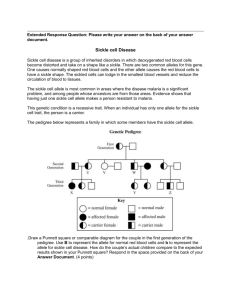
How does someone get sickle cell disorder (SCD) or beta-thalassaemia major?
Sickle cell disorders and beta-thalassaemia major are inherited, that is passed on through the family.
They are not infectious diseases and cannot be caught like coughs or colds. Sickle cell or
thalassaemia carriers are sometimes referred to as having sickle cell/thalassaemia trait. Carriers
have a normal and an affected gene. In the case of sickle cell carriers their red blood cells contain
both normal haemoglobin (adult haemoglobin, haemoglobin A) and sickle haemoglobin
(haemoglobin S). Carriers are usually perfectly healthy themselves, and may not know they have
trait unless they have a blood test. If someone is a carrier it cannot turn into sickle cell disorder or
beta-thalassaemia major. For example, if both partners are sickle cell carriers (haemoglobin AS), then
in each pregnancy there is a one in four chance that they could have a child with sickle-cell anaemia
(haemoglobin SS, a type of sickle cell disorder); a one in four chance of a child with normal
haemoglobin (haemoglobin AA), and a one in two chance of a child who is a sickle cell carrier (AS).
Good Practice: Sickle Cell and Thalassaemia in the Curriculum
One means of creating a positive school ethos is to make the curriculum relevant to the pupils. The
pattern of genetic inheritance for both sickle cell and thalassaemia are an integral part of the
genetics part of the GCSE science curriculum. The Sickle Cell Society has produced guidance on how
sickle cell can be incorporated into various key stages of the national curriculum
http://www.sicklecellsociety.orgThe UK Thalassaemia Society http://www.ukts.org has advice for
science teachers on using thalassaemia for lessons on genetics including online DVDs.
Pain: SCD is an unpredictable condition, variable over time and between different people. This
creates uncertainty for the young person. The painful crises can come on quite suddenly. Pain can
make a person grumpy, unresponsive and uncooperative. The pain of a sickle cell crisis can be mild,
moderate or severe. Since pain is such a common experience for people with SCD it is vital that the
school develops a policy for supporting children when in pain. The care plan needs to be worked out
individually for each child, with input from teacher, school nurse, sickle cell nurse specialist, child and
parents. It is very important that the policy includes instructions about giving painkillers (including
who is responsible for administration, which pain killers and how to decide which one to give).
Medication: A key part of the Individual Health Care Plan should include arrangements for giving
medication, and agreed procedures for assessing the severity of the pain. The key is to listen to the
young person. Where pain is mild or moderate a key aim should be to keep the young person in
school, by combining pain medication with an opportunity for rest and time out in a safe
environment so that they can return to lessons later in the day. A blanket policy on not administering
drugs or on having a young person collected as an outcome of administering any medication will in
effect be an exclusionary policy for the young person with a sickle cell disorder.
Teacher Awareness: All staff should be made aware of sickle cell/thalassaemia. Some schools cover
this using part of a teacher day. Staff need to know what to do if the child has a painful crisis, how to
recognize signs and symptoms of a stroke in young people with SCD, and learn to listen to the child if
the child says they are feeling unwell. Ensure there are robust systems for relaying this information
when the child has a supply teacher, when they change class or when they change school. Ensure the
availability of a safe area for a pupil with SCD or thalassaemia to recover and take time out from
activities. They may be able to return to study later in the day.
Challenging Discrimination: Ensure that SCD/thalassaemia is discussed as part of Personal, Health
and Social Education and make sure that other pupils are challenged on any discriminatory views.
7
A Framework for an Individual Health Care Plan for Someone with Sickle Cell Disorder
Name:
Date of Birth:
School:
Current Class/Group:
Condition 1: Sickle Cell Anaemia (HbSS)
Condition 2:
Condition 3:
Date of Plan:
Review Date:
PARENT/GUARDIAN/CARER CONTACTS
Contact Name:
Relationship:
Contact number:
Contact Name:
Relationship:
Contact number:
KEYWORKER RESPONSIBLE IN SCHOOL:
Photograph
CONTACT NUMBERS
Emergency Contact Name:
Emergency Contact number:
Hospital Consultant Name:
Hospital Consultant Number:
Specialist Nurse Name:
Specialist Nurse Number:
GENERAL PRACTITIONER:
Name:
Contact Name:
Building/Department:
Contact number:
Contact Number:
Date of Health and Safety Risk Assessment Carried out by School:
PREVENTION:
Key worker to ensure that each member of school staff is aware of importance of following
preventive measures….
Unrestricted access to drinking water during class time
Unrestricted access to use of the toilet, including during class time
Keeping warm: permitting coat/hat/gloves indoors, not sending outside in break
Not forcing to undertake exercise if they say they are tired or in pain
8
MEDICATION
Name of medication:
Reason for medication:
Dosage:
Time of medication:
Special Considerations:
Medication will be stored:
Arrangement for Delivery to School:
Written Records Arrangement:
PAIN MANAGEMENT
The aim is to strike a balance between responding appropriately to medical emergencies and
maintaining an inclusive school environment where a pupil with sickle cell disorder is not constantly
sent home for episodes of minor pain. Ask the specialist sickle cell nurse or hospital consultant if
there is a pain scale suitable for use in getting the young person with sickle cell disorder to say how
severe the pain they are in. There are scales in which a young person is shown drawings of a series of
cartoon faces ranging from happy (no pain) to sad and crying (most pain). Such a scale could be
included in the individual health care plan. The following scale is for illustrative purposes only and
any scale used should have the approval of the young person’s hospital consultant.
0
I am not in
any pain
2
I am in a little
pain but don’t
need my
medication
4
6
8
10
I feel if I have
my
medication I
can be in class
I feel I need to
have time out
but may feel
better later
I feel I need to
go home
I feel I need to
go to hospital
OTHER PARTICULAR NEEDS/ISSUES
This section can contain information specific to the young person’s individual
condition (for example, information about silent strokes, leg ulcers, priapism,
headaches, seizures or other possible complications of sickle cell disorder).
9
Stakeholders in drawing up IHCP
Name of Person:
Signature:
Date:
Guardian/Carer:
Signature:
Date:
School Nurse:
Signature:
Date:
Sickle Cell/Thalassaemia Specialist Nurse:
Teacher:
Signature:
Date:
Signature:
Date:
School staff Who Have Received Sickle Cell/Thalassaemia Awareness Session:
Name:
Date:
Space to include examples of good practice developed by the school:
Water
[Name] is allowed to take his water bottle into assembly. He sits at the end
of the row in order to be able to access this discreetly.
Exercise
Use other aspects of the sports activity to promote inclusion e.g. scorekeeping, timing with stopwatch
(For Beta-Thalassaemia Major or Sickle Cell Disorder) Blood Transfusions
Work with hospital to schedule regular blood transfusions so that [name] is
most energized at beginning of period of exams.
10
Further Information
RESEARCH
For a link to the research evidence underpinning the production of this information, please visit:
http://www.sicklecelleducation.com
This site includes resources for teachers including:
My Pupil has Sickle Cell Disease [Leaflet]
My Friend has Sickle Cell Disease [Leaflet]
What to Do if You Suspect your Pupil is having a Sickle Cell Crisis {Poster]
Sickle Cell and Stroke [Leaflet]
If You Teach a Child with Thalassaemia [Leaflet]
SICKLE CELL VOLUNTARY GROUPS
The Sickle Cell Society
http://www.sicklecellsociety.org
Organization for Sickle Cell Anaemia Research
http://www.oscarbirmingham.org.uk
http://www.oscarsandwell.org.uk
http://www.oscarbristol.org.uk
Sickle Cell Young Stroke Survivors
http://www.scyss.org
Broken Silence
http://www.brokensilence.org
THALASSAEMIA VOLUNTARY GROUPS
UK Thalassaemia Society
http://www.ukts.org (includes on-line DVDs)
OTHER RESOURCES
National Health Service Sickle Cell and Thalassaemia Screening Programme
http://www.sct.screening.nhs.uk
For a downloadable copy of A Parent’s Guide to Care and Management of Your Child with Sickle Cell
Disease
SCOOTER Open Education Resources for Sickle Cell and Thalassaemia
http://www.sicklecellanaemia.org/
For free sickle cell/thalassaemia images and other open educational resources
11
A downloadable copy of this leaflet is available at:
www.sicklecelleducation.com
www.sicklecellanaemia.org
This leaflet was first produced in 2011 on the basis of research funded by the United Kingdom
Economic and Social Research Council (RES-000-23-1486) a research grant held by Simon Dyson,
Lorraine Culley and Sue Dyson (De Montfort University); Karl Atkin (University of York) and Jack
Demaine (Loughborough University).
Version 1.1
12
Date: 5th January 2011