Principles of the procedures
advertisement

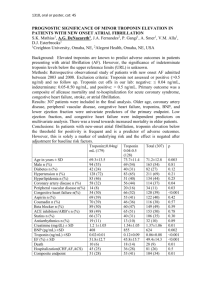
AccuTnI ASSAY PROCEDURE AccuTnI QUANTITATIVE DETERMINATION IN HUMAN SERUM AND PLASMA BY THE ACCESS IMMUNOASSAY SYSTEMS Table of Contents Principle 2 Specimen Collection 3 Reagents and Equipment 4 Calibration Details 6 Quality Control 7 Procedure 7 Results 7 Procedural Comments 8 Limitations of the Procedure 8 References 10 This document is provided as an aid to writing laboratory procedures following CLSI guidelines but does not include all activities identified in CLSI GP2-A5 Laboratory Documents: Development and Control; Approved Guideline – Fifth Edition. Each laboratory is responsible for ensuring their procedures are comprehensive and complete. Beckman Coulter, Inc. Brea, CA 92821 Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 1 of 12 A34078G Principle Principles of the procedures The Access AccuTnI assay is a two-site immunoenzymatic (“sandwich”) assay. A sample is added to a reaction vessel along with monoclonal anti-cTnI antibody conjugated to alkaline phosphatase and paramagnetic particles coated with monoclonal anti-cTnI antibody. The human cTnI binds to the anti-cTnI antibody on the solid phase, while the anti-cTnI antibody - alkaline phosphatase conjugate reacts with different antigenic sites on the cTnI molecules. After incubation in a reaction vessel, materials bound to the solid phase are held in a magnetic field while unbound materials are washed away. Then, the chemiluminescent substrate Lumi-Phos* 530 is added to the vessel and light generated by the reaction is measured with a luminometer. The light production is directly proportional to the concentration of cTnI in the sample. The amount of analyte in the sample is determined from a stored, multi-point calibration curve. Summary and Explanation Coronary artery disease is not only a leading cause of death in men and women in the US, but is also associated with other life-threatening complications (1,2,3). The development of symptoms of coronary artery disease, which at times is unexpected and sudden, is associated with increased risk for adverse cardiac events such as death, myocardial infarction (MI), or hospitalization requiring urgent revascularization. Therefore, patients presenting with ischemic syndromes require prompt management. Specific and sensitive cardiac markers (troponin I and T) have been used in conjunction with other clinical findings and patient history information to better identify subjects with MI (1,2,4,5,6). These specific cardiac markers have also been used to identify those patients at higher risk for short- and long-term adverse cardiac events (endpoints/outcomes) (1,7,8,9,10). Cardiac troponin I is a contractile protein exclusively present in the cardiac muscle (11,12). It is one of three subunits of the troponin complex (I, T, C), which with tropomyosin are bound to actin in the thin filament of the myofibril. cTnI is found as free troponin I (free TnI) and complexed with troponin C (binary IC), with troponin T (binary IT) or with both troponin C and troponin T (ternary ITC). Its physiological role is to inhibit the ATPase activity of the actin-myosin complex in the absence of calcium, and therefore, to prevent muscular contraction (13). Three tissue isoforms have been identified: Fast troponin I and slow troponin I with molecular weights of 19,800 Da each, expressed in fast twitch and slow twitch skeletal muscle fibers, respectively. cTnI with a molecular weight of 24,000 Da contains an additional 31 amino acid residues in the N-terminal. Sequencing of cTnI from mammals has shown important differences between the cardiac (14) and skeletal (15) forms. All three troponin I isoforms are encoded by different genes. The human cTnI exhibits only 52% and 54% amino acid sequence homology with the human fast and slow skeletal troponin I, respectively. The Access AccuTnI monoclonal antibody pair is selected to be cTnI specific. In addition, it has been well documented that skeletal muscle does not express cTnI, either during development or in response to stimuli (16). Therefore, the absolute cardiospecificity of cTnI allows distinction between cardiac and skeletal injuries, and allows diagnosis of myocardial infarction distinct from muscle lesions (rhabdomyolysis, polytraumatism) and non-cardiac surgery (16,17,18,19). Elevated troponin I levels have also been documented in cases of unstable angina (UA) (20) and congestive heart failure (CHF) (21). cTnI levels in acute myocardial infarction (AMI) exhibit similar rise and fall patterns to those found in CK-MB. The collection of at least three blood samples during the early triage period has been recommended (22). cTnI is 13 times more abundant in the myocardium than CK-MB and does not normally circulate in the blood, so the signal to noise ratio is more favorable for the detection of myocardial necrosis (23). Cumulative data from several studies indicate troponin I levels are detectable (above quoted values for non-AMI samples) 3-6 hours after the onset of chest pain. Troponin I levels peak at approximately 12-16 hours and can remain elevated for 4-9 days post-AMI. These same studies noted that the time to peak concentration of cTnI occurred later in patients who did not receive thrombolytic therapy (17,24,25). Unstable angina comprises a broad spectrum of patients with varying levels of risk for suffering an adverse event such as death, MI, or other major cardiac complications requiring hospitalization and potentially urgent revascularization (UR). However, it has been reported that it is difficult to predict who will suffer an adverse Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 2 of 12 A34078G event in those patients with UA and without evidence of ST segment elevation (NSTEMI) (1). The development and commercialization of the more specific and sensitive cardiac troponin I (cTnI) immunoassays have significantly contributed to the diagnosis of MI and to the risk stratification of patients with NSTEMI/UA. The 2000/2002 American College of Cardiology (ACC) and the American Heart Association (AHA) Guideline Update for the management of these patients strongly recommends to include cTnI measurements for the risk stratification of patients presenting with symptoms suggestive of acute coronary syndromes (2,6). In light of the potential adverse outcomes faced by these patients such as cardiac death or nonfatal ischemic events, an assessment of the prognosis should assist physicians in identifying and managing high risk patients. Ultimately, the assessment of the prognosis will be useful in both selecting the site of care and in identifying patients most likely to benefit from specific therapeutic interventions. The 2002 ACC and the European Society of Cardiology (ESC) guidelines recommend that individual laboratories define their own reference range and that an elevated value of cTnI be defined as a measurement above the 99th percentile of a normal control group (i.e. the 99th percentile upper reference limit) (4,5). Recent studies have shown that the predominant cTnI form present in blood of patients after AMI is the binary troponin IC complex with smaller amounts of the ternary ITC complex, binary IT complex and free cTnI (26,27,28,29). The pattern of release of these forms over the course of AMI is still under investigation. The differential recognition of complexed and free cTnI forms is common for many commercial methods (26,30,31). For some assays, the relative responses to the various forms of cTnI are nearly equal, while other assays demonstrate a substantial difference. The latter may lead to over- and under-estimation of the true concentration of troponin I in a complex biological milieu. Equimolar binding, defined as the ability to recognize both the complexed and free cTnI forms equally, allows an unbiased determination of the total cTnI present in samples from the same subject over the course of AMI. The Access AccuTnI assay recognizes the binary troponin IC or IT or ternary troponin ITC complexes and free cTnI equally. In addition, the assay responds to both the phosphorylated and dephosphorylated forms of cTnI complex equally (32). cTnI is highly susceptible to proteolysis and enzymatic modification. Substantial degradation occurs both invivo and in-vitro. The C-terminal of the molecule is preferentially cleaved then followed by the cleavage of the N-terminal (27,33,34). The Access AccuTnI assay utilizes monoclonal antibodies directed against the more stable region of the molecule, and is therefore less affected by degradation of cTnI. Specimen Collection A. Lithium heparin plasma is the recommended sample. Serum and plasma (heparin) are acceptable samples. Heparin and serum samples should not be used interchangeably (22). Each laboratory should determine the acceptability of its own blood collection tubes and serum separation products. Variations in these products may exist between manufacturers and, at times, from lot-to-lot. The AMI cutoff value presented in the Clinical Performance section applies to heparin plasma and serum samples. A study performed by Beckman Coulter, Inc. comparing EDTA plasma samples to heparin plasma samples produced the following correlation: y = 0.864x – 0.049, r = 0.999. B. Observe the following recommendations for handling, processing, and storing blood samples (ensure sample tube manufacturer recommendations are followed): 1. Collect all blood samples observing routine precautions for venipuncture (35). 2. Allow samples to clot adequately before centrifugation (35). 3. Keep tubes stoppered at all times (35). 4. Store samples tightly stoppered at room temperature (15 to 30°C) for no longer than two hours. 5. Samples should be centrifuged and refrigerated within two hours of blood draw. 6. Serum or plasma should be physically separated from contact with cells as soon as possible with a maximum time limit of two hours from the time of collection. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 3 of 12 A34078G 7. Remove any residual fibrin or cellular matter. Failure to do so can contribute to falsely elevated results. 8. For plasma, avoid transferring material from the white blood cell/platelet layer located just above the red blood cells. If a fixed angle rotor is used for centrifugation, care should be taken to avoid resuspending platelets. 9. Turbid serum or plasma samples containing particulate matter should be transferred from the original tube and recentrifuged prior to assay. A specimen (original tube) that contains a separating device (gel barrier) is never to be recentrifuged. 10. If the assay will not be completed within 24 hours, or for shipment of samples, freeze at -20°C or colder (35). 11. Samples may be stored for six months at -20°C. C. Use the following guidelines when preparing specimens: 1. Ensure residual fibrin and cellular matter has been removed prior to analysis. 2. Follow blood collection tube manufacturer’s recommendations for centrifugation. D. Each laboratory should determine the acceptability of its own blood collection tubes and serum separation products. Variations in these products may exist between manufacturers and, at times, from lot-to-lot. E. Thaw samples only once and centrifuge all thawed samples prior to analysis. Do not thaw in a water bath. Reagents and Equipment Beckman Coulter, Inc. 250 S. Kraemer Blvd. Brea, CA 92821 U.S.A. A. R1: Access AccuTnI Reagent Pack Cat. No. 33340: 100 determinations, 2 packs, 50 tests/pack. Provided ready to use. Store upright and refrigerate at 2 to 10°C. Refrigerate at 2 to 10°C for a minimum of two hours before use on the instrument. Stable until the expiration date stated on the label when stored at 2 to 10°C. Stable at 2 to 10°C for 56 days after initial use. Signs of possible deterioration are a broken elastomeric layer on the pack or control values out of range. If the reagent pack is damaged (i.e., broken elastomer), discard the pack. 1. R1a: Paramagnetic particles coated with mouse monoclonal anti-human cardiac troponin I (cTnI) suspended in TRIS buffered saline, with surfactant, bovine serum albumin (BSA) matrix, < 0.1% sodium azide, and 0.1% ProClin** 300. 2. R1b: 0.1 N NaOH. 3. R1c: Mouse monoclonal anti-human cTnI alkaline phosphatase conjugate diluted in ACES buffered saline, with surfactant, BSA matrix, protein (bovine, goat, mouse), < 0.1% sodium azide, and 0.25% ProClin 300. B. Access AccuTnI Calibrators Cat. No. 33345: S0-S5, 1 mL/vial Quantitative assay calibration is the process by which samples with known analyte concentrations (i.e., assay calibrators) are tested like patient samples to measure the response. The mathematical Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 4 of 12 A34078G relationship between the measured responses and the known analyte concentrations establishes the calibration curve. This mathematical relationship, or calibration curve, is used to convert RLU (Relative Light Unit) measurements of patient samples to specific quantitative analyte concentrations. Provided ready to use. Freeze upon receipt at -20°C or colder. Mix contents thoroughly by gently inverting before use. Avoid bubble formation. Stable until the expiration date stated on the label when stored at -20°C or colder. After initial use, the thawed vials are stable at 2 to 10°C for 60 days. Label the vials with the date of thaw or the date of expiration. Return calibrators to 2 to 10°C after each use. Do not refreeze opened vials. Signs of possible deterioration are control values out of range. Refer to calibration card for exact concentrations. Refer to the appropriate system manuals and/or Help system for information on calibration theory, configuring calibrators, calibrator test request entry, and reviewing calibration data. 1. S0: Buffered bovine serum albumin (BSA) matrix with surfactant < 0.1% sodium azide, and 0.1% ProClin 300. 2. S1–S5: Recombinant troponin complex at cTnI levels of approximately 0.3, 1.2, 5.0, 25 and 100 ng/mL (µg/L) in buffered BSA matrix with surfactant, < 0.1% sodium azide, and 0.1% ProClin 300. 3. Calibration Card: 1 C. Access Substrate Cat. No. 81906: 4 x 130 mL Provided ready to use. Refer to the following chart for storage conditions and stability. An increase in substrate background measurements may indicate instability. Condition Unopened Storage 2–8°C Stability Until expiration date stated on the label Equilibration prior to use (unopened) 15–30°C (room temperature) Minimum 18 hours Maximum 14 days In use (opened) External fluids tray substrate position Maximum 14 days Refer to the appropriate system manuals and/or Help system detailed instructions. R2 Access Substrate: Lumi-Phos 530 (buffered solution containing dioxetane Lumigen* PPD, fluorescer, and surfactant). D. Access, Access 2, SYNCHRON LXi: Access Wash Buffer II, Cat. No. A16792, 4 x 1950 mL UniCel DxI: Unicel DxI: Wash Buffer II, Cat. No. A16793, 1 x 10 L Provided ready to use. Stable until the expiration date stated on the label when stored at room temperature (15 to 30°C). An increase in substrate background measurements or increased relative light units for the zero calibrators in “sandwich”-type assays may indicate instability. Refer to the appropriate system manuals and/or Help system detailed instructions. R3 Wash Buffer: TRIS buffered saline, surfactant, < 0.1% sodium azide, and 0.1% ProClin 300. E. Quality Control (QC) materials: commercial control material. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 5 of 12 A34078G F. Access Sample Diluent A Cat. No. 81908: 4 mL/vial The analyte level in patient samples may exceed the level of the specific S5 calibrator. If a quantitative value is required, it will be necessary to dilute the samples in order to determine the analyte concentration. Provided ready to use. Allow the contents to stand for 10 minutes at room temperature. Mix gently by inverting before use. Avoid bubble formation. Stable until the expiration date stated on the vial label when stored at 2 to 10°C. Samples can be accurately measured within the analytic range of the lower limit of detection and the highest calibrator value of the specific assay. If a sample contains more analyte than the stated value of the S5 calibrator, dilute the sample following dilution instructions in the specific assay labeling under “Limitations of the Procedure” in the reagent pack section. Refer to the appropriate system manuals and/or Help system for instructions on how to enter a sample dilution in a test request. Access Sample Diluent A: Buffered BSA matrix with surfactant, < 0.1% sodium azide, 0.5% ProClin 300. G. Access Immunoassay System and supplies H. Warnings and Precautions 1. For in vitro diagnostic use. 2. Patient samples and blood-derived products may be routinely processed with minimum risk using the procedure described. However, handle these products as potentially infectious according to universal precautions and good clinical laboratory practices, regardless of their origin, treatment, or prior certification. Use an appropriate disinfectant for decontamination. Store and dispose of these materials and their containers in accordance with local regulations and guidelines. 3. Sodium azide may react with lead and copper plumbing to form highly explosive metal azides. On disposal of liquids, flush with a large volume of water to prevent azide build-up (36). 4. Xi. Irritant: 0.5% ProClin 300. R 43: May cause sensitization by skin contact. S 28-37: After contact with skin, wash immediately with plenty of soap and water. Wear suitable gloves. 5. Substrate is sensitive to air exposure. Keep tightly closed at all times. Do not pool bottles of substrate. 6. The Material Safety Data Sheet (MSDS) is available upon request. Calibration Details Run the Access AccuTnI S0 and S1 Calibrators in quadruplicate, and the S2–S5 Calibrators in duplicate. An active calibration curve is required for all tests. For the Access AccuTnI assay, calibration is required every 56 days. Refer to the appropriate system manuals and/or Help system for information on calibration theory, configuring calibrators, calibrator test request entry, and reviewing calibration data. The Access AccuTnI Calibrators are provided at six levels - zero and approximately 0.3, 1.2, 5.0, 25 and 100 ng/mL. Assay calibration data are valid up to 56 days. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 6 of 12 A34078G Quality Control Quality control materials simulate the characteristics of patient samples and are essential for monitoring the system performance of immunochemical assays. Because samples can be processed at any time in a “random access” format rather than a “batch” format, quality control materials should be included in each 24-hour time period (37). Include commercially available quality control materials that cover at least two levels of analyte. More frequent use of controls or the use of additional controls is left to the discretion of the user based on good laboratory practices or laboratory accreditation requirements and applicable laws. Follow manufacturer's instructions for reconstitution and storage. Each laboratory should establish mean values and acceptable ranges to assure proper performance. Quality control results that do not fall within acceptable ranges may indicate invalid test results. Examine all test results generated since obtaining the last acceptable quality control test point for this analyte. Refer to the appropriate system manuals and/or Help system for information about reviewing quality control results. Procedure A. Access Instrument Refer to the appropriate system manuals and/or Help system for preparation and operation. B. Assay Procedure Refer to the appropriate system manuals and/or Help system for information on managing samples, configuring tests, requesting tests, and reviewing test results. Results A. Patient test results are determined automatically by the system software using a weighted four parameter logistic curve (4PLC) math model. The amount of analyte in the sample is determined from the measured light production by means of the stored calibration data. Patient test results can be reviewed using the appropriate screen. Refer to the appropriate system manuals and/or Help system for complete instructions on reviewing sample results. B. Expected Values 1. Each laboratory should establish its own reference ranges to assure proper representation of specific populations and sample types, and to reflect current practice and criteria for AMI diagnosis at their institution. 2. Myocardial infarction has been redefined by the National Academy of Clinical Biochemistry (NACB) and the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC) Committee (4,5,22). These organizations recommend the use of biochemical markers in conjunction with the 97.5th percentile (NACB) or 99th percentile (ESC/ACC) reference ranges to aid in the diagnosis of myocardial infarction and cardiac damage. 3. The 97.5th and 99th percentiles (upper reference limit) as determined using lithium heparin plasma samples for a population of apparently healthy adults with no known cardiac disease are shown in the following table: n Age Range 97.5th percentile 99th percentile 254 19–88 0.03 ng/mL (95% CI at this concentration is 0.02–0.04) 0.04 ng/mL (95% CI at this concentration is 0.03–0.05) Note: The 95% confidence interval of a measurement of concentration at a level of the upper reference limit is calculated as two times the total %CV at the corresponding concentration. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 7 of 12 A34078G The total imprecision at 0.03 and 0.04 ng/mL was determined to be 20 and 14% CV, respectively, from the medians of nine determinations (32). 4. World Health Organization (WHO) (40) requires two of the following criteria for confirmation of AMI: evolutionary changes in the ECG or history of chest pain coupled with elevated cardiac enzymes. After a myocardial infarction, cTnI concentrations are detectable 3-6 hours after the onset of chest pain, peak at approximately 12-16 hours, and can remain elevated for 4-9 days post-AMI. 5. Any condition resulting in myocardial injury can potentially elevate cTnI levels above the expected normal range. Clinical studies have documented these conditions to include stable or unstable angina pectoris, congestive heart failure, myocarditis, and cardiac surgery or invasive testing (4,5,16,41,42). 6. Non-atherosclerotic mechanisms such as arteritis, coronary artery dissection, coronary embolism, and cocaine or amphetamine use may be responsible for acute ischemic syndrome potentially leading to cTnI levels above the reference range for healthy individuals (43,44,45). 7. The diagnostic cut-off value above which a sample is considered positive for AMI using the Access AccuTnI assay was determined by ROC analysis (46). See the Clinical Performance section for further information. 8. The AMI cutoff value presented in the Clinical Performance section applies to heparin plasma and serum samples. Procedural Comments A. Refer to the appropriate system manuals and/or Help system for a specific description of installation, start-up, principles of operation, system performance characteristics, operating instructions, calibration procedures, operational limitations and precautions, hazards, maintenance, and troubleshooting. B. Mix contents of new (unpunctured) reagent packs by gently inverting pack several times before loading on the instrument. Do not invert open (punctured) packs. C. Use forty (40) µL of sample for each determination in addition to the sample container and system dead volumes. Refer to the appropriate system manuals and/or Help system for the minimum sample volume required. D. The system default unit of measure for sample results is ng/mL. To change sample reporting units to the International System of Units (SI units), µg/L, refer to the appropriate system manuals and/or Help system. To manually convert concentrations to the International System, multiply ng/mL by multiplication factor 1. E. Run the Access AccuTnI S0 and S1 Calibrators in quadruplicate, and the S2–S5 Calibrators in duplicate. Limitations of the Procedure A. Samples can be accurately measured within the analytic range of the lower limit of detection and the highest calibrator value (approximately 0.01–100 ng/mL [µg/L]). If a sample contains less than the lower limit of detection for the assay, report the results as less than that value (i.e., < 0.01 ng/mL [µg/L]). If a sample contains more than the stated value of the highest Access AccuTnI Calibrator (S5), report the result as greater than that value (i.e., > 100 ng/mL [µg/L]). Alternatively, dilute one volume of sample with 9 volumes of Access Sample Diluent A. Refer to the appropriate system Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 8 of 12 A34078G manuals and/or Help system for instructions on entering a sample dilution in a test request. The system reports the results adjusted for the dilution. B. For assays employing antibodies, the possibility exists for interference by heterophile antibodies in the patient sample. Patients who have been regularly exposed to animals or have received immunotherapy or diagnostic procedures utilizing immunoglobulins or immunoglobulin fragments may produce antibodies, e.g. HAMA, that interfere with immunoassays. Additionally, other heterophile antibodies such as human anti-goat antibodies may be present in patient samples. (47,48) Such interfering antibodies may cause erroneous results. Carefully evaluate the results of patients suspected of having these antibodies. C. Other potential interferences in the patient sample could be present and may cause erroneous results in immunoassays. Some examples that have been documented in literature include rheumatoid factor, endogenous alkaline phosphatase, fibrin, and proteins capable of binding to alkaline phosphatase.(38,39) Carefully evaluate the results of patients suspected of having these types of interferences. D. The Access AccuTnI results should be interpreted in light of the total clinical presentation of the patient, including: symptoms, clinical history, clinical examination, electrocardiogram (ECG), data from additional tests, and other appropriate information. Medical decisions should not be based on a single AccuTnI determination at one time point. (22) E. Samples containing up to 40 mg/dL bilirubin (conjugated), 1000 mg/dL fibrinogen, 1000 mg/dL Triolein (triglycerides), 500 mg/dL hemoglobin, or 6000 mg/dL of human serum albumin do not affect the concentration of cTnI assayed. All cTnI values obtained in the presence of each interferent were 10% of the control. F. The following table describes the cross-reactivity of the assay with other myofibrillar proteins. Each of the potential cross reactants was added to a lithium heparin plasma pool containing approximately 2 ng/mL purified cTnI complex and assayed in replicates of 10. This study was based on CLSI EP7-P. (49) Analyte Added (ng/mL) Substance Cross-Reactivity (%) Skeletal troponin I 1000 0.034 Cardiac troponin C 1000 -0.002 Recombinant human cardiac troponin T 1000 -0.004 Actin (rabbit) 1000 -0.003 Myosin 1000 0.001 Tropomyosin (rabbit) 1000 -0.008 Human CK-MB 1000 -0.001 Myoglobin 1000 -0.002 G. The lowest detectable level of cTnI distinguishable from zero (Access AccuTnI Calibrator S0) with 95% confidence is 0.01 ng/mL (g/L). H. The Access AccuTnI assay does not demonstrate any "hook" effect up to 1,920 ng/mL (g/L). Beckman Coulter, the stylized logo, Access, SYNCHRON LX, UniCel and DxI are trademarks of Beckman Coulter, Inc. and are registered in the USPTO. *Lumi-Phos and Lumigen are trademarks of Lumigen, Inc., a subsidiary of Beckman Coulter, Inc. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 9 of 12 A34078G **ProClin is a trademark of Rohm and Haas Company or its subsidiaries or affiliates. References Beckman Coulter, Inc. Access AccuTnI product insert, Brea, CA 92821, P/N A34077. Beckman Coulter, Inc. Access Substrate product insert, Brea, CA 92821, P/N 386966. Beckman Coulter, Inc. Access Wash Buffer II product insert, Brea, CA 92821, P/N A16534. Beckman Coulter, Inc. UniCel DxI Wash Buffer II product insert, Brea, CA 92821, P/N A16543. 1. Heidenreich PA, Go A, Melsop KA, Alloggiamento T, McDonald KM, Hagan V, Hastie T, Hlatky MA. Prediction of risk for patients with unstable angina. AHRQ Publication No. 01-E001 December, 2000; Number 31. 2. Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J, Levin TN, Pepine CJ, Schaeffer JW, Smith EE, Steward DE, Theroux P. ACC/AHA guidelines for the management recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina). Circulation 2000; 102(10): 1193-1209. 3. Cannon CP, McCabe CH, Wilcox RG, Langer A, Caspi A, Berink P, Loper-Sendon J, Toman J, Charlesworth A, Anders RJ, Alexander JC, Skene A, Braumwald E. Oral glycoprotein IIb/IIIa inhibition with orbofiban in patients with unstable coronary syndromes (OPUS-TIMI 16) trial. Circulation 2000; 102: 149-156. 4. Alpert JS, Thygesen K, et al. Myocardial infarction redefined - A consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the Redefinition of Myocardial Infarction. JACC 2000; 36(3): 959-969. 5. The Joint European Society of Cardiology/American College of Cardiology Committee. Myocardial Infarction redefined—a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the Redefinition of Myocardial Infarction. European Heart Journal 2000; 21: 1502-1513. 6. Braunwald E, Antman EM, Beasley JW, Califf RM, Dheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J, Levin TN, Pepine CJ, Schaeffer JW, Smith EE, Steward DE, Theroux P. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina). 2002. 7. Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, Fischer GA, Fung AY, Thompson C, Wybenga D, and Braunwald E. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996; 335: 1342-1349. 8. Tanasijevic MJ, Cannon CP, Antman EM. The role of cardiac troponin-I (cTnI) in risk stratification of patients with unstable coronary artery disease. Clin Cardiol 1999; 22: 13-16. 9. Morrow DA, Rifai N, Tanasijevic MJ, Wybenga DR, De Lemos JA, Antman EM. Clinical efficacy of three assays for cardiac troponin I for risk stratification in acute coronary syndromes: A thrombolysis in myocardial infarction (TIMI) IIB substudy. Clin Chem 2000; 46(4): 453-460. 10. Antman EM, Fox KM. Guidelines for the diagnosis and management of unstable angina and non-Qwave myocardial infarction: Proposed revisions. Am Heart J 2000; 139: 461-75. 11. Wilkinson JM, Grand RJA. 1978. Comparison of amino acid sequence of troponin I from different striated muscles. Nature 271: 31-35. 12. Wade R, Eddy R, Shows TB, Kedes L. cDNA sequence, tissue-specific expression and chromosomal mapping of the human slow-twitch skeletal muscle isoform of troponin I. Genomics 1990; 7: 346-357. 13. Perry SV. The regulation of contractile activity in muscle. Biochem Soc Trans 1979; 7: 593-617. 14. Cummins P, Perry V. Troponin I from human skeletal and cardiac muscles. Biochem J 1978; 171: 251259. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 10 of 12 A34078G 15. Vallins JW, Brand NJ, Dabhaden N, et al. Molecular cloning of human cardiac troponin I using polymerase chain reaction. FEBS Lett 1990; 270: 57-61. 16. Adams III JE, Bodor GS, Davila-Roman VG, Delmez JA, Apple FS, Ladenson JH, et al. Cardiac troponin I: a marker with high specificity for cardiac injury. Circulation 1993; 88: 101-106. 17. Larue C, Calzolari C, Bertinchant JP, Leclercq F, Grolleau R, Pau B. Cardiac-specific immunoenzymometric assay of troponin I in the early phase of acute myocardial infarction. Clin Chem 1993; 39: 972-979. 18. Bakker AJ, Koelemay MJW, Gorgels JPMC, van Vlies B, Smits R, Tijssen JGP, Haagen FDM. Failure of new biochemical markers to exclude acute myocardial infarction at admission. Lancet 1993; 342: 12201222. 19. Mair J, Wagner I, Puschendorf B, Mair P, Lechleitner P, Diensti F, et al. Cardiac troponin I to diagnose myocardial injury (letter). Lancet 1993; 341: 838-839. 20. Galvani M, Ottani F, Ferrini D et al. Prognostic influence of elevated values of cardiac troponin I in patients with unstable angina. Circulation 1997; 95: 2053–2059. 21. Missov ED, De Marco T. Clinical insights on the use of highly sensitive cardiac troponin assays. Clin. Chem. Acta. 1999; 284: 175–185. 22. Wu HBA, Apple FS, Gibler B, Jesse RL et al. National Academy of Clinical Biochemistry Standards of Laboratory Practice: Recommendations for the use of cardiac markers in coronary artery disease. Clin. Chem 1999; 45(7): 1104-1121. 23. Adams JE, Schechtman KB, Landt Y, Ladenson JH, Jaffe AS. Comparable detection of acute myocardial infarction by creatin kinase MB isoenzyme and cardiac troponin I. Clin. Chem. 1994; 40: 1291-1295. 24. Mair J, Morandell D, Genser N, Lechleitner P, Dienstl F, Puschendorf B. Equivalent early sensitivities of myoglobin, creatine kinase MB mass, creatine kinase isoform ratios, and cardiac troponins I and T for acute myocardial infarction. Clinical Chemistry 1995; 41: 1266-1272. 25. Mair J, Genser N, Morandell D, Maier J, Mair P, Lechleitner P, Calzolari C, Larue C, Ambach E, Dienstl F, Pau B, Puschendorf B. Cardiac troponin I in the diagnosis of myocardial injury and infarction. Clinica Chimica Acta. 1996; 245: 19–38. 26. Wu AHB, Feng YJ, Moore R, Apple FS, McPherson PH, Buechler KF, Bodar G. Characterization of cardiac troponin I forms in the blood of patients with acute myocardial infarction and comparison of assays for troponin T and I. Clin Chem 1998; 44: 1198-1208. 27. Morjana NA. Degradation of human cardiac troponin I after myocardial infarction. Biotechnol. Appl. Biochem 1998; 28: 105-111. 28. Giuliani I, Bertinchant JP, Granier C, Laprade M, Chocron S, Toubin G, Etievent JP, Larue C, Trinquier S. Determination of cardiac troponin I forms in the blood of patients with acute myocardial infarction and patients receiving crystalloid or cold blood cardioplegia. Clin Chem 1999; 45: 213-222. 29. Katrukha AG, Bereznikova AV, Esakova TV, Pettersson K, Lovgren T, Severina ME, Pulkki K, VuopioPulkki LM, Gusev NB. Troponin I is released in bloodstream of patients with acute myocardial infarction not in free form but as complex. Clin Chem 1997; 43: 1379-1385. 30. Datta P, Foster K, Dasgupta A. Comparison of immunoreactivity of five human cardiac troponin I assays toward free and complexed forms of the antigen: implications for assay discordance. Clin Chem 1999; 45: 2266-2269. 31. Newman D, Olabiran Y, Bedzyk WD, Chance S, Gorman EG, Price C. Impact of antibody specificity and calibration material on the measure of agreement between methods for cardiac troponin I. Clin Chem 1999; 45: 822-828. 32. Uettwiller-Geiger D, Wu AHB, Apple FS, Jevans AW, Venge P, Olson MD, Darte C, Woodrum DL, Roberts S, Chan S. Multicenter evaluation of an automated assay for troponin I. Clin Chem 2002; 48(6): 869-76. 33. Lagugger R, Organ L, Collier C, Atar D, Van Eyk JE. Extensive troponin I and T modification detected in serum from patients with acute myocardial infarction. Circulation 2000; 102: 1221-1226. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 11 of 12 A34078G 34. McDonough JL, Arrell DK, Van Eyk JE. Troponin I degradation and covalent complex formation accompanies myocardial ischemia/reperfusion injury. Circ Res 1999; 84: 9-20. 35. Approved Guideline-Procedures for the handling and processing of blood specimens, H18-A3. 2004. Clinical and Laboratory Standards Institute. 36. DHHS (NIOSH) Publication No. 78-127, August 1976. Current Intelligence Bulletin 13 - Explosive Azide Hazard. Available http://www.cdc.gov/niosh. 37. Cembrowski GS, Carey RN. Laboratory Quality Management: QC QA. ASCP Press, Chicago, IL, 1989. 38. Lum G, Solarz D, Farney L. False Positive Cardiac Troponin Results in Patients Without Acute Myocardial Infarction. Labmedicine 2006; 37(9): 546-550. 39. Lingwood D, Ballantyne JS. Alkaline phosphatase–immunoglobulin conjugate binds to lipids in vitro, independent of antibody selectivity. Journal of Immunological Methods 2006; 311: 174–177. 40. World Health Organization. Report of the Joint International Society and Federation of Cardiology/World Heath Organization Task Force on Standardization of Clinical Nomenclature. Nomenclature and criteria for diagnosis of ischemic heart disease. Circulation 1979; 59: 607-9. 41. JP Etievent, et. al. Use of Cardiac Troponin I as a Marker of Perioperative Myocardial Ischemia. Annual of Thorac Surgery 1995; 59: 1192-1194. 42. TM Guest, et. al. Myocardial Injury in Critically Ill Patients. Journal of American Medical Association 1995; 273, 24: 1945–1949. 43. Braunwald E, Jones RH, Maek DB et al. Diagnosing and managing unstable angina; Circulation 1994; 90: 613-622. 44. Theroux P, Fuster V. Acute coronary syndromes. Unstable angina and non-Q-Wave myocardial infarction. Circulation 1998; 97: 1195-1206. 45. Falk E, Shak PK. Pathology of acute coronary syndromes. In Braunwald E (ed). Atlas of Heart Diseases. Acute myocardial infarction and other acute ischemic syndromes. Mosby-2001 book 1996; St Louis, 3.13.31. 46. Zweig MH, Campbell G. Receiver-Operating Characteristic (ROC) Plots: A fundamental Evaluation Tool in Clinical Medicine. Clin. Chem. 1993; 39, 4: 561-577. 47. Kricka L. Interferences in immunoassays – still a threat. Clin Chem 2000; 46: 1037–1038. 48. Bjerner J, et al. Immunometric Assay Interference: Incidence and Prevention. Clin Chem 2002; 48: 613-621. 49. Interference testing in clinical chemistry, EP7-P. 1986. National Committee for Clinical Laboratory Standards, V6, N13. Beckman Coulter, Inc. does not automatically distribute revised CLSI procedures. If you receive a revised copy of the assay insert, call Technical Support to determine if the CLSI procedure has also been revised. Printed in U.S.A. Formatted per CLSI Document GP2-A5 2012 Beckman Coulter, Inc. Page 12 of 12 A34078G