TROPonin I in Cardiovascular patients in CriticAL care. A multicentre
advertisement
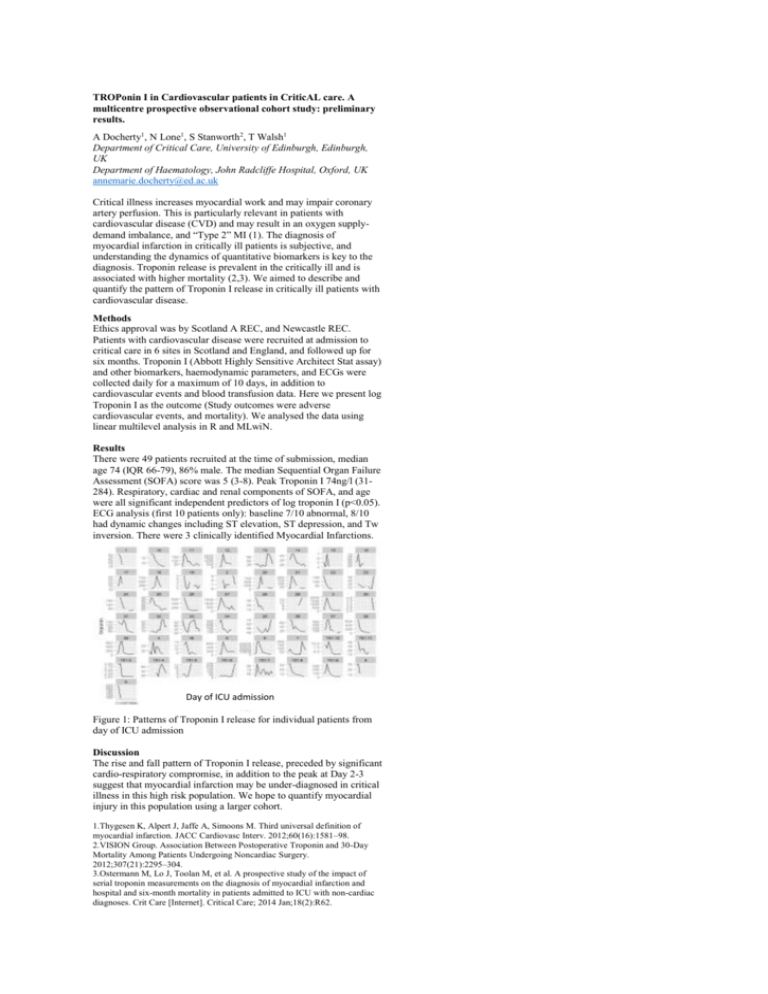
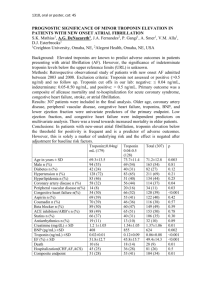
TROPonin I in Cardiovascular patients in CriticAL care. A multicentre prospective observational cohort study: preliminary results. A Docherty1, N Lone1, S Stanworth2, T Walsh1 Department of Critical Care, University of Edinburgh, Edinburgh, UK Department of Haematology, John Radcliffe Hospital, Oxford, UK annemarie.docherty@ed.ac.uk Critical illness increases myocardial work and may impair coronary artery perfusion. This is particularly relevant in patients with cardiovascular disease (CVD) and may result in an oxygen supplydemand imbalance, and “Type 2” MI (1). The diagnosis of myocardial infarction in critically ill patients is subjective, and understanding the dynamics of quantitative biomarkers is key to the diagnosis. Troponin release is prevalent in the critically ill and is associated with higher mortality (2,3). We aimed to describe and quantify the pattern of Troponin I release in critically ill patients with cardiovascular disease. Methods Ethics approval was by Scotland A REC, and Newcastle REC. Patients with cardiovascular disease were recruited at admission to critical care in 6 sites in Scotland and England, and followed up for six months. Troponin I (Abbott Highly Sensitive Architect Stat assay) and other biomarkers, haemodynamic parameters, and ECGs were collected daily for a maximum of 10 days, in addition to cardiovascular events and blood transfusion data. Here we present log Troponin I as the outcome (Study outcomes were adverse cardiovascular events, and mortality). We analysed the data using linear multilevel analysis in R and MLwiN. Results There were 49 patients recruited at the time of submission, median age 74 (IQR 66-79), 86% male. The median Sequential Organ Failure Assessment (SOFA) score was 5 (3-8). Peak Troponin I 74ng/l (31284). Respiratory, cardiac and renal components of SOFA, and age were all significant independent predictors of log troponin I (p<0.05). ECG analysis (first 10 patients only): baseline 7/10 abnormal, 8/10 had dynamic changes including ST elevation, ST depression, and Tw inversion. There were 3 clinically identified Myocardial Infarctions. Day of ICU admission Figure 1: Patterns of Troponin I release for individual patients from day of ICU admission Discussion The rise and fall pattern of Troponin I release, preceded by significant cardio-respiratory compromise, in addition to the peak at Day 2-3 suggest that myocardial infarction may be under-diagnosed in critical illness in this high risk population. We hope to quantify myocardial injury in this population using a larger cohort. 1.Thygesen K, Alpert J, Jaffe A, Simoons M. Third universal definition of myocardial infarction. JACC Cardiovasc Interv. 2012;60(16):1581–98. 2.VISION Group. Association Between Postoperative Troponin and 30-Day Mortality Among Patients Undergoing Noncardiac Surgery. 2012;307(21):2295–304. 3.Ostermann M, Lo J, Toolan M, et al. A prospective study of the impact of serial troponin measurements on the diagnosis of myocardial infarction and hospital and six-month mortality in patients admitted to ICU with non-cardiac diagnoses. Crit Care [Internet]. Critical Care; 2014 Jan;18(2):R62.