Tcells
advertisement
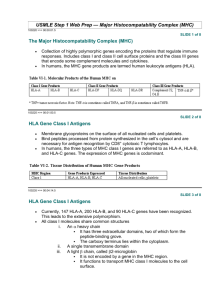
T cells and Cell-mediated Immunity Recall: two major components of the immune system: o innate immunity – non-specific phagocytosis and inflammation o acquired immunity – antigen-specific B and T lymphocyte responses two major types of immune responses o humoral immunity – proteins dissolved in blood and lymph (eg. antibodies, complement) bind to extracellular pathogens and toxins o cell-mediated immunity – immune cells (eg. cytotoxic T lymphocytes, natural killer cells) attack and destroy extracellular pathogens, and cells infected with intracellular pathogens T lymphocytes are important in all parts of the immune response because they o can recognize and respond to specific antigens, either by attacking infected cells directly or by activating other immune cells via cytokines & cell-cell interactions The life story of a T-lymphocyte: Childhood – growing up in the bone marrow hematopoietic stem cell common lymphoid progenitor Tcell precursor (thymocyte) Adolescence – moving to the thymus for maturation and ‘training’ thymocyte arrives in the thymic cortex (TCR- CD4- CD8-, “double negative”) undergoes genomic rearrangement in order to form a unique and functional T-cell receptor gene (TCR+) learns to express both co-receptors (CD4+ CD8+ , “double positive”) positive selection – only cells whose TCR recognizes self MHC survive chooses one co-receptor (CD4+ or CD8+ , “single positive”) negative selection – cells who are too self-reactive are killed the 2% who survive the whole process continue on into the thymic medulla from here, the mature T cells can enter the bloodstream Early Adulthood – traveling throughout the blood, lymph and tissues naïve T cells circulate back and forth between blood and peripheral lymphoid tissue until they encounter an MHC-peptide complex on an antigen-presenting cell (APC) that they can bind particularly well when this binding happens, they are activated and transformed into effector T cells (‘priming’) Late Adulthood – proliferating and working activated T cells proliferate rapidly, forming a population of cells specific to the antigen in question these cells play an important role in the immune response, which varies based on the type of effector cell they become o CD8+ cytotoxic T cells (kill infected cells) o CD4+ TH1 cells (activate infected macrophages) or TH2 cells (activate antigenspecific B cells to make antibodies) Old Age – cell death and immunological memory once the infection has passed, most of the effector cells undergo apoptosis some, however, become long-lived memory cells, which can be re-activated in case of subsequent infection The Major Histocompatibility Complex (MHC) the MHC is a cluster of genes on chromosome 6 (or chromosome 17, if you’re a mouse) that encode important immune proteins the genes in the cluster are divided into 3 classes o Class I MHC proteins present cytosolic peptides to T cells o Class II MHC proteins present exogenous (endocytic) peptides to T cells o Class III includes a variety of other molecules (TNFα and β, complement components, heat shock proteins, steroid 21-hydroxylases) MHC Class I and II proteins are polygenic o in humans, the 3 class I genes are called HLA A, B and C o and the 3 class II genes are called HLA DP, DQ and DR MHC Class I and II proteins are polymorphic o within the population, there are many possible alleles for each of the HLA genes the particular arrangement of MHC alleles found on a given chromosome is called a haplotype o the MHC genes are very closely linked on the chromosome, and tend to be inherited as a unit – so you get a haplotype from each parent o these genes are co-dominantly expressed, so you’ll express the alleles from both parents at once the two MHC classes have different structures and functions: MHC Class I heavy chain + β2-microglobulin found on most nucleated cells binds peptides from the cytoplasm binding at the ends of the groove binds peptides 8-10 amino acids long displays to CD8+ T cells MHC Class II α-chain + β-chain found only on antigen-presenting cells binds peptides from endosomes binding along the sides of the groove binds peptides 10-25 amino acids long displays to CD4+ T cells in both MHC classes, two of the protein domains form a peptide-binding groove this groove is able to bind a wide variety of peptides, because it forms hydrogen-bonds with the peptide bonds connecting the amino acids, rather than with the individual amino acids themselves at the same time, each kind of MHC molecule has a preference for a particular group of peptides, based on the presence of certain amino acid side chains (‘anchor residues’) which fit into the ‘specificity pockets’ in the groove of that molecule Class I MHC molecules bind cytosolic peptides and present them to CD8+ T cells o healthy cells present normal self peptides (eg. from ribosomes, histones, cytochromes, etc.), which the T cells know to ignore o infected cells present foreign viral proteins, which elict a cytotoxic T cell response to kill the infected cell Class II MHC molecules bind endosome peptides and present them to CD4+ T cells o the APC internalizes the pathogen via phagocytosis or endocytosis o in the endosome, the pathogen is killed and broken down into peptides o the peptides bind to Class II MHC molecules, and are presented on the cell surface where they can elicit a helper T cell response (resulting in macrophage activation and/or cytokine production) T cells that make it out of your thymus are ‘MHC restricted’ – that is, they only respond to antigenic peptides if they’re displayed on your particular kinds of MHC molecules so your haplotype determines what kinds of peptides your cells can display to passing T cells, and thus it helps determine the kind of immune response you’ll have to a given pathogen this can be clinically relevant, since things like ragweed allergy and autoimmune diseases (eg. Grave’s disease, Type I diabetes, rheumatoid arthritis, etc.) can be linked to particular MHC alleles T Cell Receptor (TCR) recall: each B cell expresses a unique immunoglobulin molecule, with a particular antigenic specificity – this is accomplished by randomly recombining heavy and light chain genes at the genomic (DNA) level a similar process occurs in T cells, where each cell randomly recombines its TCR α and β genes to produce a unique TCR molecule with a particular MHC+peptide specificity first the β chain undergoes VDJ recombination if that’s successful, the α chain undergoes VJ recombination if that’s successful, the cell expresses a mature α β TCR and can undergo positive and negative selection positive selection results in MHC restriction negative selection results in self-tolerance note: T cells also exist, but they only constitute 1% of blood lymphocytes and have limited diversity so we don’t pay much attention to them T cell self-tolerance in the thymus, dendritic cells display normal MHC+peptide combinations to the developing T cells any T cells which are activated by these self-antigens are made to undergo apoptosis however, there must be some MHC+peptide combinations that are normal in some parts of the body but aren’t found in the thymus – why don’t we react to those? answer: naïve T cells require more than just binding to MHC+peptide in order to become activated and stimulate an immune response they need a co-stimulatory signal, which occurs when a B7 molecule on the APC binds to a CD28 molecule on the T cell once they have become properly activated by the co-stimulatory signal, future interactions only require the TCR to MHC+peptide binding in order to provoke a response the co-stimulatory signal is typically provided by dendritic cells, which only express lots of the B7 molecule and MHC in response to an inflammatory stimulus (eg. bacterial LPS) so, T cells only get activated when there is already an inflammatory reaction in progress eg. the need for adjuvents in vaccines in order to get a decent immune response also, naïve T cells may be ‘ignorant’ of self-antigens, but if something stimulates them to become effector T cells, they will have lower thresholds and may respond eg. viral infection that triggers an auto-immune reaction