Adverse Incidents and Near Misses Management Policy
advertisement

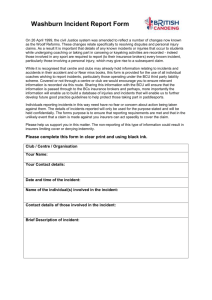
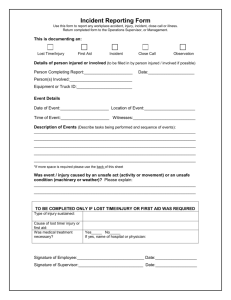
Policy for the Management of Adverse Incidents and Near Misses Version 3 Name of responsible (ratifying) committee Serious Incident Review Group Date ratified 28 January 2014 Document Manager (job title) Head of Risk Management Date issued 07th February 2014 Review date January 2016 (unless requirements change) Electronic location Management Policies Related Procedural Documents Risk Management Strategy Management of Serious Incidents Requiring Investigation Investigation of Incidents, Complaints and Claims. Management of Complaints, Concerns, Comments and Plaudits Being Open Policy Management of Claims, Clinical Negligence Liabilities to Third Parties and Property Expenses Scheme Disclosure of Information to the Police Policy How to Report an Adverse Incident Key Words (to aid with searching) Incident; Serious Incident; Adverse Incident In the case of hard copies of this policy the content can only be assured to be accurate on the date of issue marked on the document. For assurance that the most up to date policy is being used, staff should refer to the version held on the intranet Version Date Ratified 3 Jan 14 Brief Summary of Changes Alignment to NRLS definitions Inclusion of Duty of Candour requirements Addition of screening incidents Update to responsibilities Changes to monitoring Removal of Guidance on Grading Incidents replaced by NRLS definitions Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Author A Green Page 1 of 23 CONTENTS QUICK REFERENCE GUIDE ............................................................................................................. 3 1. INTRODUCTION.......................................................................................................................... 4 2. PURPOSE ................................................................................................................................... 4 3. SCOPE ........................................................................................................................................ 4 4. DEFINITIONS .............................................................................................................................. 4 5. DUTIES AND RESPONSIBILITIES .............................................................................................. 5 6. PROCESS ................................................................................................................................... 6 7 TRAINING REQUIREMENTS ...................................................................................................... 9 8 REFERENCES AND ASSOCIATED DOCUMENTATION .......................................................... 10 9 EQUALITY IMPACT STATEMENT ............................................................................................ 10 10 MONITORING COMPLIANCE - As a minimum, the following elements will be monitored.......... 11 Appendix A: Reportable incidents ..................................................................................................... 12 Appendix B: Guidance on grading incidents ...................................................................................... 14 Appendix C: How to Report an Adverse Incident .............................................................................. 15 Appendix D: Reporting to External Agencies..................................................................................... 20 Appendix E: Informing external agencies: when, why and by whom ................................................. 21 Appendix F: VTE Reporting and Investigation Process ..................................................................... 22 Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 2 of 23 QUICK REFERENCE GUIDE For quick reference the guide below is a summary of actions required. This does not negate the need those involved in the process to be aware of and follow the detail of this policy. PROCESS FOR THE REPORTING AND MANAGEMENT OF AN ADVERSE INCIDENT INCIDENT OCCURS 1. Address the immediate health needs of the person(s) involved 2. Grade the incident (ref: NRLS guidance in Appendix B)– Red(Severe/Death)/Amber(Moderate)/Yellow(Low)/Green/Near miss(No Harm) NB: incident may be re-graded following review by your Manager or the Risk Management Department, following further investigation 3. Report the incident onto DatixWeb using the on-line electronic adverse incident reporting form (guidance in Appendix C) 4. Consider the level of required communication with the patient 5. Any VTE Incident follow the process at appendix F Severe/Death Moderate Low No Harm No Harm RED (including ‘Never Events’) AMBER YELLOW GREEN NR MISS Must be reported immediately, will require an initial investigation panel arranged and managed in accordance with the Trust Policy on the Management of Serious Incidents Requiring Investigation Issues reported to / monitored via: CSC Governance Teams Serious Incident Review Group Pressure Ulcer Review Group Governance & Quality Committee Trust Board CSC Performance Reviews CCGs PSSG Complete an on-line electronic adverse incident form Inform appropriate senior member of staff Risk Advisors will be automatically alerted to the incident and notified via email Line Managers will be automatically alerted to the incident and notified via email Senior member of staff to ensure appropriate type, level and ownership of investigation (to be investigated by CSC in which incident occurred) is completed and risk management advised of the outcome of the investigation. The incident must then be closed on DatixWeb Complete an on-line electronic adverse incident form Inform appropriate senior member of staff Senior member of staff must review the incident within 5 days, complete details of any long-term action and close the incident on DatixWeb within a further 5 days Issues reported to / monitored via: CSC Governance Committees/CSC SIRG Governance & Quality Committee as part of CSC reporting Issues reported to / monitored via: CSC Governance Committees/CSC SIRG Patient Safety Working Group Governance & Quality Committee as part of CSC reporting VTE weekly panel It is essential that staff receive feedback via their line management route, on reported incidents and actions taken. Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 3 of 23 1. INTRODUCTION In a service as large and complex as the NHS, things will sometimes go wrong. When they do, the response should not be one of blame and retribution, but of learning and a drive to reduce risk for future patients, visitors and staff. Therefore, the Trust is committed to developing a just culture and to encouraging a willingness to admit mistakes without fear of punitive measures. In support of this, the Trust accepts that completion of an incident form does not constitute an admission of liability and will not result in automatic disciplinary action. There are occasions, of course, when it may be necessary to take action against individuals which will be governed by appropriate HR policies: acts of maliciousness or criminal or gross/repeated professional misconduct. The policy has been formulated in response to the Department of Health publications An Organisation with Memory, Building a Safer NHS, Doing Less Harm and the National Patient Safety Agency publications Building a memory: preventing harm, reducing risks and improving patient safety, Seven Steps to Patient Safety and Being Open: Communicating Patient Safety Incidents with Patients and their Carers. The policy is also designed to ensure compliance with the requirements of external agencies. However, the ultimate aim is to reduce the risk of harm to patients, staff and other users of Trust premises through improving the safety and quality of services and the environment. 2. PURPOSE This policy sets out the processes for the appropriate identification and reporting of adverse incidents and near misses. 3. SCOPE This policy applies to all permanent, locum, agency, bank and voluntary staff of Portsmouth Hospitals NHS Trust, the MDHU (Portsmouth) and Carillion, whilst acknowledging that for staff other than those directly employed by the Trust the appropriate line management or chain of command will be taken into account ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ 4. DEFINITIONS Adverse incident: an event or omission relating to a patient, visitor or staff member or any event or circumstances arising during NHS care that could have or did lead to unintended or unexpected harm, loss or damage. See Appendix A for more information on incidents that should be reported. Patient safety incident: any unintended or unexpected incident which could have, or did, lead to harm for one or more patients receiving NHS-funded healthcare. Serious incident requiring investigation (SIRI): (commonly classified as a ‘red’ incident) an incident that occurred during NHS funded healthcare (including in the community) which resulted in one or more of the following: unexpected or avoidable death or severe harm of one or more patients, staff or members of the public a ‘never event’ – all never events are defined as a SIRI although not all necessarily result in severe harm or death. a scenario that prevents, or threatens to prevent, an organisation’s ability to continue to deliver healthcare services, including data loss, property damage or incidents in Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 4 of 23 population programmes like screening and immunization where harm potentially may extend to a large population allegations or incidents of physical abuse and sexual assault or abuse loss of confidence in the service, adverse media coverage or public concern about healthcare or an organisation If in doubt, it is better to report an incident as a potential SIRI, as this can then be confirmed by the Clinical Service Centre (CSC) or at the Initial Investigation Panel meeting. All grade 3 and 4 pressure ulcers, death attributable to either C Diff or MRSA (part 1 of death certificate), death or major harm attributable to VTE ,and ‘Never Events’ – as defined by the Department of Health (Appendix A) – must be reported as SIRIs Never Event: a largely preventable patient safety incident that should not occur if the available preventative measures have been implemented Near miss: a situation in which an event or omission, or a sequence of events or omissions, arising during clinical care fails to develop further, whether or not as a result of compensating action, thus preventing injury to a patient Harm: an injury (physical or psychological), disease, suffering, disability or death to patients, staff or members of the public. In most instances, harm can be considered to be unexpected if it is not related to the natural course of the patient’s illness, treatment or underlying condition. Root Cause Analysis: A well recognised way of investigating incidents, claims and complaints, which offers a framework identifying what, how and why the event happened. Analysis can then be used to identify areas of change, develop recommendations and look for new solutions. DatixWeb: A Patient Safety & Risk Management System that provides a comprehensive picture of our organisation’s risks by collating information from incidents affecting patients, staff & visitors 5. DUTIES AND RESPONSIBILITIES Deputy Director of Nursing/Head of Patient Safety The Deputy Director of Nursing/Head of Patient Safety, has responsibility for ensuring the strategic implementation of this policy. The Head of Risk Management The Head of Risk Management has responsibility for the operational and day-to- day implementation of this policy. Risk Management Team The Risk Advisors are responsible for supporting and advising staff at all levels across the Trust, to ensure that this policy is implemented across the Trust and for ensuring external agencies (Appendices D and E) are informed, if required. Risk Analyst The Risk Analyst has responsibility for ensuring that the database of incidents is maintained, providing reports for CSCs and Trust Board. Clinical Service Centre (CSC) Governance Leads The Governance Leads are responsible for ensuring that all adverse incidents and near misses are reported and managed in line with this policy and are discussed at CSC Governance Committees or CSC SIRG and shared with staff. All Managers Managers are responsible for ensuring their staff are released for training, are fully assisted and supported throughout the reporting and handling of an adverse incident or near miss and Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 5 of 23 receive feedback on the outcome of any investigation. Where staff experience particular difficulties associated with an adverse incident or near miss, managers should consider referring the staff member or members to the Occupational Health Department or the AQUILIS counseling service, in accordance with the Human Resources Policy for Supporting Staff The Reporter of any incident must: Ensure the immediate safety of those directly affected by the adverse event or near miss Complete an on-line electronic adverse incident form Immediately inform the appropriate senior member of staff/line manager 6. PROCESS 6.1 Near Misses (No harm to patient, impact prevented) The reporter must: Ensure the immediate safety of those directly affected by the incident Complete an on-line electronic adverse incident form Inform the appropriate senior member of staff / line manager The senior member of staff must: Review the incident within 5 days, and confirm the grading. Complete details of any long-term actions necessary, on the electronic form and close the incident on DatixWeb within a further 5 days Ensure feedback is provided to the reporter Note: consideration should be given to the potential severity of the near miss had it actually impacted upon a patient, staff member or visitor and the appropriate level of investigation pursued. 6.2 Incidents graded Green (No harm to patient, impact not prevented) or Yellow (Low harm) The reporter must: Ensure the immediate safety of those directly affected by the incident Complete an on-line electronic adverse incident form Inform the appropriate senior member of staff / line manager The senior member of staff must: Review the incident within 5 days and confirm the grading Complete details of any long-term actions necessary, on the electronic form and close the incident on DatixWeb within a further 5 days Ensure feedback is provided to the reporter 6.3 Incidents graded Amber (Moderate harm) The reporter must: Ensure the immediate safety of those directly affected by the incident Complete an on-line electronic adverse incident form Inform the appropriate senior member of staff/line manager Risk Advisors and Line Managers will be automatically notified of the incident via email The senior member of staff must: Review the incident within 5 days and confirm the grading; Ensure an amber investigation is instigated, in conjunction with the CSC Governance Lead/Head of Nursing; As part of the ‘Amber’ investigation process, complete a Root Cause Analysis (RCA), make certain a member of staff is identified to communicate with the Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 6 of 23 patient or relatives and ensure compliance with Duty of Candour requirements. Further guidance is available in the Trust’s Being Open Policy Ensure feedback on decision to investigate is given to reporter; Inform Risk Management of the outcome of the investigation and close the incident on DatixWeb 6.4 Incidents graded Red (severe/permanent harm or death) Incidents graded red should be managed in accordance with the Trust Policy for the Management of Serious Incidents. But briefly Within office hours (08:30 – 17:00) The witness to the SIRI will: Ensure the immediate safety of those directly affected by the SIRI; Complete an on-line electronic adverse incident form; and Immediately inform the appropriate senior member of staff/line manager Risk Advisors, Line Managers and relevant specialist members of staff (eg Risk Management Pharmacist) will be automatically notified of the incident via email The senior member of staff will: Inform the CSC Management Team; Inform the patient’s consultant; Determine who will speak to the patient or relatives and ensure compliance with Duty of Candour requirements see Being Open Policy Preserve the scene of the incident, if necessary e.g. retention of equipment; Request statements; and Ensure the appropriate support is provided to staff Inform the on-call Supervisor of Midwives if applicable Out of hours (With the exception of pressure ulcers and VTEs) The senior member of staff will inform: Hospital duty manager (for clinical incidents only) On-call consultant On-call duty Director On-call duty Director to inform CCG/Comms Team (if necessary; depending on type/severity/scale of SIRI) e.g. an incident potentially causing high media interest or disruption to service provision Inform the on-call Supervisor of Midwives if applicable Determine who will speak to the patient or relatives and ensure compliance with Duty of Candour requirements see Being Open Policy All confirmed SIRIs must be subject to a panel, investigated using full RCA and be signed off through the Serious Incident Review Group (SIRG) see SIRI Policy 6.5 Guidance on grading can be found at Appendix B. Advice can also be sought from the Risk Management Department 6.6 All incidents must be documented in the patient’s health records, including a note of the incident number 6.7 Safeguarding 6.7.1 If a concern is regarding the welfare of an adult patient and a suspected safeguarding incident, staff should refer to the Adult Safeguarding policy, complete the reporting form and contact the Safeguarding Adults Office 6.7.2 If a concern is regarding the welfare of a child, and a suspected safeguarding incident, staff should refer to the Child Safeguarding policy, complete the reporting form and contact the named nurse or midwife for safeguarding children. Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 7 of 23 6.8 Screening Incidents Incidents relating to national screening programmes must be discussed with the Regional Quality Assurance Director in line with local and national guidelines and escalated to Commissioners as appropriate. PHT currently participates in the following national screening programmes: Breast Cancer Bowel Cancer Cervical Cancer Diabetic retinopathy (managed by Care UK) Newborn screening 6.9 The Investigation Adverse incidents and near misses are subject to an appropriate level of investigation and root cause analysis and where relevant an improvement strategy prepared. Not all events need to be investigated to the same extent or depth and the investigation and analysis should be relative to the seriousness, complexity of the event and/or whether it resulted in actual harm and the potential for learning, such as those which are high frequency but may be of low severity. Further detail can be found in the Trust Policy for the Investigation of Incidents, Complaints and Claims. Red Incidents (Severe harm or Death) Any red or potential red incident will be subject to an initial investigation panel. Once confirmed the incident must be managed as set out in the Trust Policy on the Management of Serious Incidents Requiring Investigation, this includes full RCA investigation, sign off at SIRG and is subject to external reporting requirements. Duty of Candour requirements must be followed to ensure the patient/family are fully aware of the event and subsequent investigation Amber Incidents (Moderate harm) Investigations into amber incidents will be carried out by only one or two key staff, e.g. local manager and clinician with advice from the Risk Management Department, if required. Whilst these investigations may require less input than investigations into red incidents it is essential to establish the root cause(s), lessons to be learned and to comply with the Duty of Candour requirements. All incidents in this category will be subject to review and monitoring by the relevant CSC Governance Committees, to ensure learning and the implementation of any required changes in practice. Yellow (Low harm) / Green (No harm, impact not prevented) / Near Miss (No harm, impact prevented) Incidents: It is the responsibility of the CSC Management Team to ensure that all incidents in this category are investigated with the appropriate thoroughness and subject to aggregated review and monitoring by the relevant CSC Governance Committees, to ensure learning and the implementation of any required changes in practice. They are unlikely to warrant individual investigation, but root cause analysis of trends should be undertaken, perhaps as part of a working group, and a preventative risk management strategy established to prevent recurrence. 6.10 Central recording of adverse incidents and near misses All adverse incidents and near misses and the outcome of any investigations are automatically inputted onto the electronic database (DatixWeb) which is maintained within the Risk Management Department, to support analysis and feedback, identification of key themes and organisational learning. 6.11 Organisational Learning No adverse event policy will be effective unless there is organisational learning and feedback on the lessons learned and any required changes in practice implemented. The Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 8 of 23 Trust has introduced a number of processes to enable learning and feedback, which include: Internal A systematic approach to the recording and trending of incidents through the use of an electronic reporting system and database; Monthly Quality Exception reports to the Trust Board; Monthly Business Intelligence reports to the Trust Board; Quarterly Quality Report to the Trust Board and Governance and Quality committee. The report provides an aggregated view of issues concerning patient safety, patient experience and clinical effectiveness Presentation of quarterly information to the Patient Safety Steering Group; Production of reports specifically tailored to the needs of various groups e.g. pressure ulcer review group, falls group; Monitoring of incidents at the monthly CSC Governance Committees; and A Risk Management intranet site that can be accessed by all staff and that holds all relevant documents and reports, including: incident reports; legal updates from solicitors; NRLS updates. External Reporting of all patient safety incidents to the National Reporting and Learning System (NRLS). The reports produced by the NRLS, are then used for both benchmarking and learning across the Trust; Reporting of all patients safety incidents to the Care Quality Commission, via the NRLS; Reporting onto STEIS Receipt by the Commissioners of the quarterly Quality Report and the monthly Quality Exception and Business Intelligence reports, used to inform the Commissioner’s targets for the Trust; A monthly meeting with the Commissioners at which various aspects of incidents are discussed, to provide assurance on organisational learning; Reporting of any relevant incident to external agencies, as required (Appendix E) 6.12 Staff are also able to raise concerns in line with the Trust’s Whistleblowing Policy. This policy enables staff to raise concerns about wrongdoing at work in a way which protects their interests, and which ensures at the same time, that instances of wrongdoing, alleged wrongdoing or apparent wrongdoing are properly investigated and dealt with. The policy is designed to: Provide a way for members of staff concerned about the care or safety of patients to speak out in the event of other procedures failing or being exhausted. Provide an effective and confidential process to enable staff to challenge practices or behaviours if they believe others are acting in an unlawful and/or unethical way Ensure victimisation or retribution against staff will not be tolerated Protect staff if they speak out appropriately 7 TRAINING REQUIREMENTS 7.1 Training forms part of the Trust’s Essential Skills and Training Requirements; as identified in the Training Needs Analysis. It is included in mandatory Corporate Induction and in Essential Updates 7.2 Staff undertake Essential Update refresher training via the Electronic Staff Record (ESR) system every two years Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 9 of 23 7.3 All training is recorded on the ESR from which the Learning and Development Team provide a monthly heat map to each CSC, to enable monitoring of compliance 7.4 Compliance is further monitored through the CSC performance reviews with the Executive Team 8 REFERENCES AND ASSOCIATED DOCUMENTATION External National Patient Safety Agency, July 2005. Building a Memory: preventing harm, reducing risks and improving patient safety www.npsa.nhs.uk National Health Service Litigation Authority, April 2011, Risk Management Standards www.nhsla.com National Health Service Litigation Authority, April 2010, Clinical Negligence Scheme for Trusts - Clinical Risk Management Standards – Maternity www.nhsla.com Hampshire County Council Protecting People from Abuse guide Internal Management of Serious Incidents Requiring Investigation Investigation of Incidents, Complaints and Claims. Management of Complaints, Concerns, Comments and Plaudits Management of Claims Clinical Negligence Liabilities to Third Parties and Property Expenses Scheme Being Open Policy Risk Management Strategy Maternity Risk Management Strategy Trust Policy and Protocol on Whistleblowing Policy Health & Safety Policy Disclosure of Information to the Police 9 EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly Adverse Incident and Near Misses Issue 3 07/02/2014 (Review date: January 2016 unless requirements change) Page 10 of 23 10 MONITORING COMPLIANCE - As a minimum, the following elements will be monitored Minimum requirement to be monitored Lead Tool Frequency of Report of Compliance 95% of incidents/ near misses are reported in accordance with this policy Internal Audit Audit of random selection of 50 DatixWeb reports Annually 95% of relevant incidents will be appropriately reported to external agencies Head of Risk Management Audit of random selection of 20 SIRIs Annually Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Reporting arrangements Policy audit report to: Head of Risk Management Patient Safety Steering Group Policy audit report to: Lead(s) for acting on recommendations Head of Risk Management Patient Safety Steering Group Page 11 of 23 Appendix A: Reportable incidents Reportable Incidents Whilst it is not possible to cover every eventuality, the following incidents must always be reported: some of which will be considered to be Serious Incidents Requiring Investigation (SIRIs) and investigated in accordance with that policy. For ease of reference the incidents have been loosely grouped into: clinical care; information governance; accident/damage/theft/loss; other; and never events Clinical Care Absence of consent form / incomplete consent form Unmarked / incorrectly marked surgical site Inappropriate surgery performed Unexpected outcomes Unexpected death Any major clinical incident e.g. failure to diagnose a serious illness Medication incidents Patient slips/trips/falls Pressure ulcers Unexpected patient moves (more than 4 moves) Any incident involving multiple patients e.g. cervical screening incidents Absconding patient Suicide / serious self-harm Incidents relating to radiology regulations (IRMER) Death related to Clostridium Difficile (C Diff) Death related to Methicillin Resistant Staphylococcus Aureus (MRSA) VTE/PE Information Governance Breach of confidentiality Loss of person identifiable data Incidents relating to health records, including unavailability Breach of security Accidents / Damage / Theft / Loss Involving any person on Trust premises Incidents involving any vehicle on Trust premises Theft of property: Trust, staff or patient Loss of property: Trust, staff or patient Damage to Trust property: premises; fixtures; equipment etc Injury or ill-health suffered as a result of handling patients or inanimate object Contact with bodily fluids – needlesticks Contact with harmful chemicals or spillages Fire: actual or false alarm Other Expression or act of violence or aggression “Rogue” staff Procedure or protocol related incidents, including failure to follow Never Events (as defined by the DoH) Wrong site surgery Wrong implant/prosthesis Retained foreign object post-operation Wrongly prepared high-risk injectable medication leading to death or severe harm Maladministration of potassium-containing solutions leading to death or severe harm Wrong route administration of chemotherapy Wrong route administration of oral/enteral treatment leading to death or severe harm Intravenous administration of epidural medication leading to death or severe harm Maladministration of insulin leading to death or severe harm Overdose of midazolam during conscious sedation leading to death or severe harm Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 12 of 23 Opioid overdose of an opioid-naïve patient leading to death or severe harm Inappropriate administration of daily oral methotrexate Fall from unrestricted windows leading to death or severe harm Entrapment in bedrails leading to death or severe harm Transfusion of ABO-incompatible blood components leading to death or severe harm Transplantation of ABO or HLA-incompatible organs leading to death or severe harm Misplaced naso or oro-gastric tube leading to death or severe harm Wrong gas administered leading to death or severe harm Failure to monitor and respond to oxygen saturation in patient undergoing general/ regional anaesthesia or conscious sedation and leading to death or severe harm Introduction of intravascular air embolism leading to death or severe harm Misidentification of patients as a result of failure to use standard identification processes and leading to death or severe harm Severe scalding of patients as a result of water used for washing/bathing and leading to death or severe harm Maternal death due to post-partum haemorrhage after elective C-section If in doubt, it is always better to report than not, but advice can be obtained from your line manager or the Risk Management Department Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 13 of 23 Appendix B: Guidance on grading incidents NRLS Definitions of Levels of Harm No Harm (Near Miss): Impact prevented – any patient safety incident that had the potential to cause harm but was prevented, resulting in no harm to people receiving NHS-funded care No Harm (Green): Impact not prevented – any patient safety that ran to completion but no harm occurred to people receiving NHS-funded care. Low (Yellow): Any patient safety incident that required extra observation, or minor treatment and caused minimal harm to one or more persons receiving NHS-funded care. Moderate Harm (Amber): Any patient safety incident that resulted in a moderate increase in treatment and which caused significant but not permanent harm, to one or more persons receiving NHS-funded care Severe (Red): Any patient safety incident that appears to have resulted in permanent harm to one or more persons receiving NHS-funded care Death (Red): Any patient safety incident that directly resulted in the death of one or more persons receiving NHSfunded care. Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 14 of 23 Appendix C: How to Report an Adverse Incident HOW TO REPORT AN ADVERSE INCIDENT Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 15 of 23 DatixWeb for Incidents Contents 1. Introduction 2. Accessing the Adverse Incident Reporting Form 3. Adding a new Adverse Incident 4. Additional Fields 5. Submitting the Adverse Incident Reporting Form Any questions associated with this document or any DATIX related questions should be addressed to: Risk Analyst Portsmouth Hospitals Trust Room 0.23 De La Court House Queen Alexandra Hospital Cosham Hants 02392 286000 x 3477 1. Introduction DID YOU KNOW THAT … All accidents, adverse incidents and near misses must be reported, even if they appear to be minor Serious adverse incidents (SIRIs)(RED) must be immediately reported to your line manager or duty manager and the risk department by telephone. Once you have been trained, you MUST use DATIX (our electronic report form) to report all adverse events and near misses 1.1. What is DATIX? A Patient Safety & Risk Management System Used by more than 75% of NHS organisations as well as private health care providers. Provides a comprehensive picture of our organisation’s risks by collating information from incidents affecting patients, staff & visitors 1.2. Things to REMEMBER A question mark on the form means that there is some helpful information available which can be revealed by the clicking the button A red star denotes mandatory fields Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 16 of 23 A down arrow indicates that there are options available from the drop down box If in any doubt when completing the form then refer to your line manager or direct any queries to the risk management team. Q. Are you uncertain whether to report an adverse incident? A. If in doubt, report it! 2. Accessing the Adverse Incident Report Form Click on the button on the PHT intranet Home Page as shown below. 3. Adding a New Adverse Incident The DIF1 form is available to all staff that have a PHT login. No user names or passwords are required to access the DIF1 form. The form is split into sections, each section focusing on a different aspect of the adverse event being reported i.e. Summary of incident Additional information Person reporting the incident The first section of the form gives users some additional information to aid completion and answer any initial questions they may have. Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 17 of 23 REMEMBER: Once an Adverse Event Form has been started it must be completed – if you close the form prior to submitting, the information will not be retained and you will have to start again. 3.1. Summary of Incident This section lets the reviewer know details of the incident and where it took place and who was involved. A ‘question mark’ on the form means there is some helpful information available which can be revealed by clicking the button and a red asterix indicates a mandatory field. Other fields might open dependant on choice entered into previous fields. 3.2. Additional Information Clicking on the drop down boxes reveals the ‘pick lists’ for reporters to choose from, this will then open up extra sections to gather more detailed information. Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 18 of 23 3.2.1 Was anyone one else involved in this incident? Enter the details of anybody else involved, as with the above question, extra fields will open dependant on the options selected. You can add additional names by clicking on the ‘Add another‘ button. 3.2.2 What Category of incident is this? Select from the dropdown box an option which fits the incident; this will open up additional sections for further detailed information gathering. 3.2.3 Does this incident involve safeguarding? If answering yes, a new field will open asking which team needs to be notified. A pop up will give you the opportunity to open a safeguarding form to fill out on-line. You can save this form to your own profile on the network and send to the team via e-mail.0 3.2.4 Tick the box it there are any documents to attach to this incident. This will open up another section where you can browse and locate files to add to the incident form. Additional or supporting documents relating to the incident will need to be scanned and saved to the PC before they can be attached to the incident. 3.3. Details of Person Reporting the Incident. This is about you the reporter, fill in the relevant details. Populate ‘your e-mail address’ with your PHT email address and you will get an acknowledgement from the Datix system once your form has been submitted. Once you are happy that all the information has been entered, click on the submit button Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 19 of 23 Appendix D: Reporting to External Agencies INCIDENT THAT MAY REQUIRE EXTERNAL REPORTING INCLUDING THOSE RELATING TO A SUSPICION OF CRIME/ARRESTABLE/SERIOUS OFFENCE IMMEDIATELY REPORT THE INCIDENT/ISSUE TO YOUR LINE MANAGER / SENIOR PERSON IN THE DEPARTMENT / WARD Record that you have reported it / to whom / when. Complete on-line electronic adverse incident form LINE MANAGER / SENIOR PERSON ESCALATES INFORMATION Line manager / senior to record to whom escalated / when CLINICAL SERVICE CENTRE MANAGEMENT TEAM HOSPITAL DUTY MANAGER DUTY EXECUTIVE RISK MANAGEMENT DEPARTMENT ext 3475/6 Any of the above will be able provide further advice on who needs to be notified OTHER AGENCIES POLICE If there is a suspicion that a crime or arrestable offence may have been committed or you have been requested by the person affected to call the police on their behalf (Details of what constitutes a crime or arrestable offence can be found in the ‘Disclosure of Information to the Police Policy’ 2013 which can be found on the Trust intranet under: policies and guidelines→ management polices→ Disclosure of Information to the Police 2013) These include but are not limited to: Care Quality Commission Coroner Counter-fraud Agency Disclosure and Baring Service Environment Agency Environmental Health Agency Health and Safety Executive Information Commissioner Medicines and Healthcare Products Regulatory Agency (MHRA) Professional Regulatory Bodies. Strategic Health Authority IF IN ANY DOUBT PLEASE TAKE ADVICE – DON’T IGNORE ANY POTENTIALLY REPORTABLE ISSUE Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Page 20 of 23 Appendix E: Informing external agencies: when, why and by whom The following are examples of the external agencies that may need to be informed in the event of an adverse incident. If you need any advice in this regard please do not hesitate to contact the Risk Management Department Agency Circumstances Reporter Care Quality Commission Counter-fraud Agency SIRIs related to breach of radiology regulations e.g. IRMER Actual or suspected fraud Environment Agency Major contamination of the environment Environmental Health Agency SIRI involving food poisoning originating in, or being transferred through the Trust Health and Safety Executive The Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 1995 (RIDDOR), place a legal duty on employers to report work-related deaths[1], major injuries[2] or over-three-day injuries[3], work related diseases[4], and dangerous occurrences (near miss accidents)[5]. When the Trust 1. Dismisses or withdraws permission for an individual to engage in a regulated or controlled activity, or would have done so had that individual not resigned, retired, been made redundant or been transferred to a position which is not a regulated or controlled activity because 2. they think that the individual has: engaged in relevant conduct satisfied the Harm Test; or received a caution or conviction for a relevant offence All level 3 information governance SIRIs Health and Safety Manager Suspected safety problems with medicines, medical devices, blood and blood components. Member of staff who discovers the problem– guidance available on Pharmacy intranet web site Death or injury where it is considered there are unusual or suspicious circumstances Theft of / malicious damage to, Trust property Violent or aggressive incidents where it is considered police involvement is required Arson Where there are concerns about the practice of a healthcare professional. Medical Director / Director of Nursing Disclosure and Baring Service Information Commissioner Medicines and Healthcare Products Regulatory Agency (MHRA) Police Professional Regulatory Bodies. Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Radiation Protection Adviser Deputy Director of Nursing/Head of Patient Safety/Executive Director of Finance/CSC Management Team Director of Human Resources and Workforce Head of Hotel Services – Carillion Deputy Director of Nursing/Head of Patient Safety CSC Management Team / Head of Human Resources Information Governance Manager Security Manager / Duty Director Medical Director / Director of Nursing / Senior Manager Deputy Director of Estates Medical Director / Director of Nursing of specific professional lead, depending on healthcare professional involved. Page 21 of 23 Appendix F: VTE Reporting and Investigation Process VTE Reporting and Investigation Confirmed DVT or PE diagnosis Department / ward complete DATIX form VTE Admin Support identify PE’s from PACS reports – if not already on DATIX complete form VTE Admin Support made aware of DVT’s by Vascular Lab – if not already on DATIX complete form Department / ward complete DATIX form Incident closed/rejected and logged as COMMUNITY NO Risk / VTE Admin Support review – Relevant hospital attendance within 90 days? No further PHT investigation YES VTE Admin Support email CSC Management Team - to inform of event, request IMR, give details of panel date / time of attendance CSC arranges for completion of Initial Management Report (IMR ) and CSC representative to attend VTE panel IMR must include: IMR completed and sent to VTE in-box in time for scheduled Weekly VTE panel VTE@porthosp.nhs.uk • • • CSC present IMR at Weekly VTE Panel Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) • If patient had been an inpatient, had surgery or attended ED with POP application within previous 90 days. If patient risk assessed and assessment documented on admission to hospital. If any thrombosis risk factor is identified, that thromboprophylaxis (mechanical or chemical) was prescribed in accordance with NICE guidelines Whether any prescribed prophylaxis was delayed or omitted Page 22 of 23 VTE Panel and ongoing Process CSC representative presents IMR at weekly VTE panel meeting VTE panel grade incident GREEN Appropriate assessment and prophylaxis followed RED AMBER PHT/NICE assessment and prophylaxis guidelines not followed and PHT/NICE assessment and prophylaxis guidelines not followed but no DEATH OR MAJOR HARM DEATH OR MAJOR HARM SIRI process instigated and reported to CCG by Risk Dept Investigator appointed to complete RCA. Submit to VTE@porthosp.nhs.uk within 28 days UNAVOIDABLE Investigator appointed to complete RCA. Submit to VTE@porthosp.nhs.uk within 28 days CSC rep presents completed reports to VTE Incident Review Group for sign off Definition of MAJOR HARM: Patient requiring Thrombolysis DCCQ admission Resuscitation Adverse Incident and Near Misses Issue 3 (Review date: January 2016 unless requirements change) Learning fed back to CSC / Trust wide via Governance structure CSC presents feedback of action plan outcome to Thrombosis Committee Page 23 of 23