Inverted nipples
advertisement

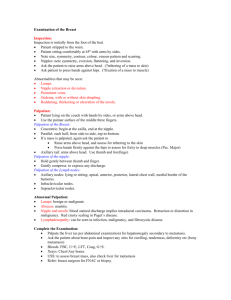
Lip Teh Inverted Nipples First described by Ashley Cooper 1840 2% of women have at least 1 inverted nipple Unilateral more common than bilateral Aetiology 1. CONGENITAL (most common) i. Lack of dense connective tissue beneath the nipple that normally plays an important role in maintaining its projection. Worse in association with greater subcutaneous fat accumulation. (Schwager) ii. A lack of smooth muscle growth into the nipple from the areolar iii. Scarring under the nipple iv. Arrest of the ductal system development = relative shortness of the lactiferous ducts, which tether the nipple and prevent it projecting. v. Abnormal fibromuscular structures encompass the lactiferous ducts and are inserted in the nipple dermis, holding it in the inverted position. (Pitanguy) 2. Acquired i. Mastitis ii. Macromastia iii. Breast reduction surgery iv. Breast carcinoma (need to exclude) v. Scarring post breast feeding Classification (Han and Hong 1999) Grade I. The inverted nipple is easily pulled out, maintains its projection fairly well without traction. Gentle finger pressure around the areola or gently pinching the skin causes the nipple to pop back out. Minimal or no fibrosis. There is no soft-tissue deficiency of the nipple. The lactiferous duct should be normal without any retraction. Grade II. The nipple can be pulled out manually, but not as easily as in grade I. After releasing traction, the nipple tends to fall back and invert again. Moderate degree of fibrosis. The lactiferous ducts are mildly retracted but do not need to be cut for the release of fibrosis. On histologic examination, these nipples have rich collagenous stromata with numerous bundles of smooth muscle Grade III. The nipple is severely inverted and retracted. It is very difficult to pull out these nipples manually. Despite application of pressure on the nipple to force it to protrude, it promptly retracts. The fibrosis is remarkable and lactiferous ducts are short and severely retracted. The bulk of soft tissue is markedly insufficient in the nipple. Histologically, there are atrophic terminal duct lobular units and severe fibrosis Lip Teh Clinical Problems 1) Functional a. Breast feeding b. Frequent irritation and inflammation due to poor hygiene and the inability to clean within the inversion. 2) Cosmetic/Psychological/sexual Treatment 1) medical (for breast feeding) a. Breast shells( milk cups, breast cups, or breast shields) i. uses elasticity of the skin during pregnancy ii. applying gentle constant pressure to the areola in an effort to break the adhesions under the skin that prevent the nipple from protruding. iii. Ideally, shells should be worn starting in the third trimester of pregnancy for a few hours each day. iv. After the baby is born, these same shells can be worn about 30 minutes prior to each feeding to help draw out the nipple even more. v. any milk collected in them should NOT be saved. b. Hoffman Technique. i. Manually stretching out nipple 5x/day c. Breastpump./Nipple suction device i. After birth, breastpump can be helpful at drawing out a flat or inverted nipple immediately before ii. can be used at other times following delivery to help further break the adhesions under the skin by pulling the nipple out uniformly from the center. d. Nipple stimulation. i. After birth, if the nipple can be grasped, a mother can roll her nipple between her thumb and index finger for a minute or two and then quickly touch the nipple with a moist, cold cloth or ice wrapped in cloth e. Nipple shield. i. flexible nipple made out of silicone that is placed over the mother's nipple during feedings so that latch-on is possible for the baby. ii. To prevent the baby from becoming too addicted to nursing with the shield, it should be removed as soon as the baby is latched-on and nursing well. iii. Possible problems associated with the use of nipples shields include a drop in the mother's milk supply and insufficient transfer of milk to the baby. 2) Surgical a. Goals i. restoration of an adequate projecting nipple together with an areola Lip Teh ii. preservation of the lactiferous for a patient who may want to breast-feed. b. 2 main types i. Ducts preserved (Grade I-II) ii. Ducts sacrificed (Grade III) 1. Hartrampf and Schneider(1976) reported that the nipples maintained normal sensation and erectile power Surgical Methods Create tightness at the neck of the inverted nipple. 1) Skin excision Kehrer(1888), Deaver(1917)and Basch(1893) introduced methods of excising a ring of areolar skin from around the nipple or subcutaneous myotomy of the areolar muscle. However, these techniques are more applicable to a depressed nipple than to a truly inverted nipple Axford(1889) created a tight neck by excising three elliptical pieces of skin radially and applying a purse-string suture around the nipple. Grodsky(1937) introduced a method for creating four triangles of skin with the base on the nipple margin and the apex toward the areola, followed by direct closure of the defects to produce nipple projection. DuFourmentel, (1950) expressing dissatisfaction with the techniques designed to preserve the lactiferous ducts, introduced a technique for attaining aesthetic objectives based on a V-Y technique that cuts all the fibrous bands but not the ducts. Namba technique (1966) involves the creation of a tight neck at the nipple base with three simple half-Z-plasties without sacrificing the duct system or adding bulk to the nipple to maintain nipple projection.( tighten the neck base and elongate the length of the neck.) Schematic diagram of the Namba technique. (Above, left) Preoperative design. The length of a-c is about 1 cm. The angle of acd is 30 to 45 degrees. (Above, center) Triangular flaps are elevated. 2) Purse String method Lip Teh Stark (1980) cut the areola to a depth of 1 cm around the nipple and placed two horizontal mattress sutures from 6 to 12 o'clock and from 9 to 3 o'clock. This type of suturing or a purse-string suture at the base may interfere not only with blood supply to the nipple but also with lactation. Peled 1999 Traction will indicate the need and success of release of the deep tissues. This is done with the sharp edge of a regular injection needle, 18 gauge, introduced at 6 o'clock deeply at the base of the nipple or with a microsurgical blade. By moving the needle horizontally in a fan-like movement while pulling the traction suture, the breast ducts are divided and the skin is released. In cases of ill-defined or missing nipples, there is no need for release. Through the same hole at 6 o'clock, a subcuticular, pursestring, 4-0 clear nylon suture is placed. The stitch takes small deep bites, exiting the skin at the marked line every 5 to 6 mm, and entering through the same skin hole described for knifeless otoplasty. It progresses around the entire circumference. At the completion of the subcutaneous, buried, purse-string suture, both thread ends come out at 6 o'clock, the same hole originally entered. While pulling the traction suture, the purse string is tied, creating the nipple mound . The knot buries spontaneously under the skin, and the hole is left open for spontaneous healing. The wrinkling of the areolar skin at the base of the nipple improves spontaneously in 3 weeks. Not suitable for nipple projection in scarred skin 3) Piercing (Scholten 2001) With body jewellery Nipple is brought out with a pair of forceps, and a holding suture of 2-0 Vicryl is used to further evert the nipple. Gentle traction is applied until there is good projection. The nipple is pierced through the marking points at its base with a 16-gauge Biovalve intravenous catheter needle. To achieve maximal nipple projection, the first half of the nipple is pierced inward, whereas the second half is in a more outward direction. The position of the needle is assessed without traction from the suture. Small adjustments at this stage can be made if necessary. When a satisfactory position is achieved, body jewellery replaces the needle and the polytetrafluoroethylene catheter is slowly withdrawn. I normally insert a so-called barbell, which is a straight bar of stainless steel, tapped at both ends with balls that screw in place. For initial treatment, I prefer to use high-quality stainless steel. However, when the piercing is completely healed, this device can be replaced with other materials (e.g., polytetrafluoroethylene, titanium, gold, or silver). An everted nipple with a projection of at least 9 to 10 mm could be achieved in all cases. Healing is generally complete within 2 weeks. In case of treatment in the later stages of pregnancy, the nipple will stay everted until suckling of the newborn baby begins, at which time the body jewelry can be removed, although this is not strictly necessary. Should wear jewellery for at least 3 months. Recurrence rate likely to be high Add bulk beneath the nipple 1) Elsahy (1976) Two de-epithelialized triangular dermal flaps at 3 and 9 o'clock. A curved circumferential incision is made around the nipple, so the pathologic fibrous bands and lactiferous ducts are left undisturbed. Lip Teh Flaps wrapped around the nipple in a subcutaneous tunnel as a sling 2) Teimourian (1980) Modification of above. Differences a) The directions of the flaps were altered from 3 and 9 o'clock to 12 and 6 o'clock to create less interference with the blood and nerve supply to the nipple b) all the lactiferous ducts were cut c) the dermal flaps were used as supportive bulk under the nipple rather than as a sling. Superior to Elsahy's procedure in that nipple projection is better achieved and the recurrence rate is lower; but this technique excludes the possibility of future lactation Schematic diagram of modified Teimourian technique. (Left and center) Preoperative design. The length of a-b is 1.5 cm. The length of a-c is less than 1 cm. The length of a-d is about 1.5 cm (varies with size of nipple). (Right) Cross-sectional view of operative method. Triangle flap a-b-d is de-epithelialized and developed as composite flap. Dissection is continued below composite flap toward bundle of lactiferous ducts. Shortened lactiferous ducts and associated fibrous structures are completely interrupted. Two superior and inferior composite flaps are hinged toward dissected space and sutured together to provide structural bulk. Points a and b are subdermally approximated to tighten nipple neck base. 4) intranipple strutting with bilateral deepithelialized dermal flaps (Lee 1998) Lip Teh The nipple proper is dissected free from the underlying attachment under loupe vision, with splitting and stretching by sharp Metzenbaum dissection in the vertical plane so as to minimize ductal injury with selective release of fibrous bands. The deepithelialized skin flaps were positioned erect in intranipple slits, forming a strut. The remaining proximal portion of the deepithelialized skin flaps are sutured together in the subcutaneous tunnel. The V-Y fashioned closure of the donor defect further accentuates nipple projection by placing the flap base in a more centripetal direction. Complications 1. infection 2. hematoma 3. nipple sensory change 4. loss of erectile function 5. loss of lactation 6. partial/total nipple necrosis 7. incomplete correction 8. partial/complete relapse(3-10%) 9. scarring Diagram showing the most common pattern of blood supply. Lip Teh The operative technique in three grades. (Above) Grade I. The eversion of the nipple is maintained only by purse-string suture. (Center) Grade II. The fibrosis (small x) is released, and a purse-string suture is added. (Below) Grade III. Lactiferous ducts are cut, and the fibrosis is released. Triangular dermal flaps are turned under the nipple and sutured together. A purse-string suture is added. Lip Teh