Nausea and Vomiting in Adolescents and Adults Rahul Kuver, M.D.
advertisement

Nausea and Vomiting in Adolescents and Adults Rahul Kuver, M.D. , John V. Sheffield, M.D. , and George B. McDonald, M.D. 1.0 Introduction Nausea means feeling "sick to the stomach", a sensation that is associated with the urge to vomit. Vomiting, the forceful discharge of gastric contents, may be a protective physiologic mechanism that prevents entry of potentially harmful substances into the gastrointestinal tract (1). Persistent vomiting can lead to dehydration, severe alkalosis, bleeding and rarely esophageal perforation -irrespective of the cause of vomiting. Vomiting is to be differentiated from retching, regurgitation or rumination. Retching or dry heaves involves the same physiological mechanisms as vomiting, but occurs against a closed glottis; there is no expulsion of gastric contents. Regurgitation is the return of small amounts of food or secretions to the hypopharynx in the context of mechanical obstruction of the esophagus, gastroesophageal reflux disease or esophageal motility disorders. Rumination is similar to regurgitation, except small amounts of completely swallowed food are returned to the hypopharynx from the stomach and is often re-swallowed (2). Rumination is not associated with nausea. This review of nausea and vomiting is based on a MEDLINE literature search encompassing 1990-2000, using the MeSH headings Nausea and Vomiting with the subheadings Complications, Diagnosis, Drug Treatment, Treatment, Etiology, Psychology and Radiography. Certain articles, including placebo-controlled trials of therapy, comprehensive reviews and other publications deemed seminal, were reviewed and are referenced. Certain articles prior to 1990 were also reviewed. The emphasis is placed on articles that provide evidence which can be incorporated into guidelines for diagnosis and management. Certain patients typically present with nausea and vomiting, such as cancer chemotherapy patients, patients recovering from general anesthesia, pregnant women and patients whose symptoms are related to motion. Many of these patients are seen in the primary care setting. In most cases, the history can point to the etiology without the need for sophisticated diagnostic testing or referral. In a minority of patients, unusual causes of nausea and vomiting may require thorough diagnostic testing and referral to a specialist (1). Assessment of the duration of nausea and vomiting is an important initial point in the history. Symptoms present for less than a week may be due to conditions which are separable from those causing symptoms over weeks, months or years. For acute nausea and vomiting, the diagnostic algorithm is based on three key questions (Table 1): 1. Whether immediate therapy is needed due to the consequences of nausea and vomiting regardless of the underlying cause 2. Whether empiric treatment and reassurance are sufficient 3. Whether expeditious work-up is required to establish the cause. For chronic nausea and vomiting, the diagnostic algorithm is based on history and physical exam findings that point to the organ system involved: the gastrointestinal tract, the nervous system or the endocrine system. Psychogenic causes are an important additional category to consider in chronic nausea and vomiting. A subset of patients will have no cause identified despite extensive diagnostic testing. This group of patients may benefit from referral to specialized centers. Certain presentations prompt referral to a gastroenterologist (Table 12). 1.1 Associated Symptoms Certain symptoms are typically associated with nausea and vomiting. Associated upper GI tract complaints such as bloating, early satiety, dysphagia and odynophagia should be sought. Dyspepsia can be associated with nausea. Lightheadedness, abdominal or chest pain, cough or hematemesis are symptoms that should prompt an assessment for conditions that may require immediate therapy regardless of the underlying cause of nausea and vomiting. A missed menstrual period, vertigo, arthralgias, low grade fevers and nausea and vomiting associated with motion are clues that suggest a condition that may be treated empirically . Symptoms that are severe, such as chest or abdominal pain, CNS symptoms, fever with chills, a history of an underlying systemic disease or of immunosuppression should prompt a diagnostic workup. 1.2 Physiology of nausea and vomiting The vomiting reflex is triggered by stimulation of chemoreceptors in the upper GI tract and mechanoreceptors in the wall of the GI tract which are activated by both contraction and distension of the gut as well as by physical damage. A coordinating center in the central nervous system controls the emetic response. This center is located in the parvicellular reticular formation in the lateral medullary region of the brain. Afferent nerves to the vomiting center arise from abdominal splanchnic and vagal nerves, vestibulo-labyrinthine receptors, the cerebral cortex and the chemoreceptor trigger zone (CTZ).The CTZ lies adjacent in the area postrema and contains chemoreceptors that sample both blood and cerebrospinal fluid. Direct links exist between the emetic center and the CTZ. The CTZ is exposed to emetic stimuli of endogenous origin such as hormones associated with pregnancy and to stimuli of exogenous origin such as drugs (3). The efferent branches of cranial nerves V, VII, and IX, as well as the vagus nerve and sympathetic trunk produce the complex coordinated set of muscular contractions, cardiovascular responses and reverse peristalsis that characterizes vomiting (4). The area postrema is rich in dopamine receptors and is a target for the antagonists haloperidol, metoclopramide and the phenothiazines. Histamine-1 and muscarinic cholinergic receptors are present in the nucleus ambiguus and lateral vestibular nucleus. 5-hydroxytryptamine (5HT) receptors are present within the area postrema. 5HT can activate dopamine release. The new 5HT3 receptor antagonists have demonstrated efficacy against cytotoxic chemotherapy-induced emesis (5). Drugs effective against motion sickness-- such as promethazine, diphenhydramine and scopolamine--have little effect against cytotoxic drug-induced emesis. 2.0 Acute nausea and vomiting Symptoms present for less than a week are defined as acute. The causes of nausea and vomiting of short duration are often separable from etiologies leading to more chronic symptoms. In the initial evaluation of a patient presenting with acute nausea and vomiting, assessment regarding the need for immediate therapeutic intervention regardless of the underlying cause is important. If immediate therapeutic intervention to correct the consequences of vomiting are not necessary, or has been performed, then the important questions are whether empiric treatment of nausea and vomiting and reassurance are sufficient, and whether expeditious diagnostic work-up to determine the underlying cause is necessary. These latter two questions are linked, and key historical points can help determine the most appropriate diagnostic testing and therapy. Referral for additional diagnostic tests and/or management needs to be considered for a variety of situations. 2.1 Immediate therapeutic intervention is necessary regardless of the cause. Vomiting with intravascular volume depletion requires immediate intervetion Certain consequences of vomiting require immediate treatment regardless of the cause. The diagnosis and treatment of conditions described in this section are outlined in (Table 2). If vomiting has been severe and protracted, intravascular volume depletion may have occurred, leading to orthostatic hypotension and renal insufficiency. Hypokalemic hypochloremic alkalosis results from loss of gastric hydrochloric acid, increased H+ loss due to renin-angiotensin-aldosterone and volume contraction. In these situations, intravascular access should be established and fluid resuscitation instituted prior to diagnostic studies. Vomiting or retching can cause mucosal injury and bleeding Either vomiting or retching can lead to mucosal injury (e.g. Mallory-Weiss tear), evident as hematemesis and/or melena; excessive blood loss may contribute to intravascular volume depletion. In the case of GI bleeding with a significant drop in hematocrit or signs of intravascular volume depletion, consultation for upper endoscopy should be obtained. In certain situations, depending on the findings on endoscopy and the effectiveness of endoscopic therapy, surgical consultation may be necessary. Vomiting can lead to aspiration Vomitus may be aspirated, leading to respiratory compromise which may be severe enough to require endotracheal intubation and mechanical ventilation. A corollary to this is the development of aspiration pneumonitis or pneumonia. In the case of aspiration and hypoxemia, ensuring a patent airway is of paramount importance. The management of such patients requires a multidisciplinary approach, and may include the services of an intensivist, gastroenterologist and primary care physician. Vomiting or retching can lead to esophageal rupture Vomiting or retching may cause rupture of the esophagus (Boerhaave syndrome), a surgical emergency. Boerhaave syndrome deserves special consideration because a high index of suspicion is required to make a timely diagnosis and surgical intervention is necessary. Spontaneous rupture of the esophagus is an intrathoracic disaster if left untreated. As noted in a recent review of all published cases in the literature since 1980 and 18 additional cases (6), non-specific symptoms such as chest and abdominal pain can lead to mistaken diagnoses such as pulmonary embolus, myocardial infarction, aortic dissection, spontaneous pneumothorax, pancreatitis or perforated peptic ulcer. Forty percent of patients had a history of alcoholism, and 41% had peptic ulcer disease. Pain (83%) and vomiting (79%), often associated with dyspnea (39%) and shock (32%), were the major symptoms. Physical exam may detect crepitus due to air in the soft tissues of the neck and thorax. Chest and abdominal X-rays may show subcutaneous emphysema, pneumothorax, pneumomediastinum, pleural effusion and free mediastinal air. However, up to a third of patients have normal routine X-rays initially (7). Esophagograms with water-soluble contrast agents are diagnostic in most cases. Thoracic CT scans may reveal mediastinal air or pleural fluid even when the esophagogram shows no leak and should be obtained when there is a high degree of suspicion. In the series cited, the mortality rate was 31%, an improvement on the 50% mortality rate noted prior to 1980. Intra-abdominal bleeding is a rare complication of vomiting Intra-abdominal bleeding is a rare complication of vomiting. Hemoperitoneum has been described following vomiting. Splenic laceration secondary to persistent emesis in a pregnant patient was diagnosed at laparotomy (8). Hepatic laceration caused by vomiting leading to massive intra-abdominal hemorrhage was described (9). In both cases, abdominal pain in the context of nausea and vomiting was the chief complaint. Surgical intervention is necessary for diagnosis and treatment. Rectus sheath hematoma, diagnosed by ultrasound or CT, may lead to abdominal pain, and needs to be considered in the patient who is anticoagulated (10). Anticoagulation or low platelet counts may lead to intramural hematomas of the esophagus after vomiting. The presentation is one of severe substernal or intrascapular pain, hematemesis and dysphagia. 2.2. Empiric treatment and reassurance are sufficient If the patient does not have complications of vomiting that require immediate attention, and if the underlying cause of the nausea and vomiting as suggested by the history does not require expeditious work-up and therapy, then the patient can be reassured and treated empirically with anti-emetic agents (Table 11). Before such a decision is made, however, symptoms and signs that favor a selflimited illness should be reviewed and compared with findings that favor serious underlying disease. Such a comparison is provided in (Table 3). Key questions can help identify conditions that can be treated empirically. Certain presentations and etiologies are sufficiently characteristic as to be identifiable as self-limited. In these situations, no specific treatment is necessary, or, if specific therapy is available, the benign nature of the condition precludes the need for an extensive diagnostic evaluation. A majority of patients seen in the ambulatory care setting falls into this category. 2.2.1 Early pregnancy If the patient is a woman of child-bearing age, a pregnancy test should be done. Pregnancy-related nausea and vomiting is common, reported in 70-90% of pregnancies (11)(123). Rising estrogen and progesterone levels during pregnancy have been implicated, as has maternal serum prostaglandin E2 levels (124). The onset is usually shortly after the first missed menstrual period, and symptoms may begin before the woman recognizes that pregnancy has occurred. Symptoms typically begin by four to six weeks of gestation, peaking in severity by eight to twelve weeks, and resolving spontaneously by the 20th week (11). Nausea, sometimes accompanied by vomiting, is noted especially in the morning. In one prospective study of 160 pregnant women, however, "morning sickness" occurred in only 1.8%, whereas 80% reported nausea lasting all day (125). Symptoms usually disappear by the fourth month of pregnancy, although they may persist into the third trimester. Babies born to a mother with nausea and vomiting of pregnancy have birth weights similar to babies born to mothers without these symptoms. Thus, the prognosis for mother and baby is generally excellent. However, in one study a higher than normal incidence of antepartum hemorrhage was noted (12). Vomiting during pregnancy is not teratogenic (13). If pregnancy-related nausea and vomiting are not characteristic of morning sickness (for example, has its onset in the second or third trimester and is severe), then other potentially more serious conditions such as hyperemesis gravidarum, acute fatty liver of pregnancy, and HELLP syndrome need to be considered. In general, referral to an obstetrician for management of nausea and vomiting of pregnancy is indicated for these more serious conditions. Treatment of Pregnancy-related nausea and vomiting For typical pregnancy-related nausea and vomiting, reassurance is often all that is needed, although an anti-emetic may be necessary. Traditionally, dietary advice such as dry toast in the morning and avoiding fatty foods was offered. Antacids for reflux symptoms associated with nausea and vomiting may be used. If an anti-emetic is necessary, then antihistamines may be used and are considered safe for use during pregnancy. The efficacy or safety of phenothiazines or metoclopramide have not been established for nausea and vomiting of pregnancy in controlled trials despite their widespread use (11). Clinical trials assessing the efficacy of anti-emetic therapy are of varialbe quality. An analysis of such trials showed that anit-histamines, pyridoxine, and P6 acupressure appeared to reduce the frequency of nausea in early pregnancy (126). A risk-benefit assessment of drug therapy for nausea and vomiting of pregnancy show that controlled trials demonstrated the safety and efficacy of dicyclomine, anti-histamine H1 receptor antagonists, and phenothiazines (127). The pooled data, however, were not homogenous. A prospective trial comparing pregnancy outcomes in women given metoclopramide in the first trimester for the treatment of nausea and vomiting in pregnancy compared to women who received nonteratogenic drugs, showed no increased risk of fetal malformations, spontaneous abortions, or decreased birth weight of the infants in the metoclopramide group (135). The effectiveness of pyridoxine (vitamin B6) for nausea and vomiting of pregnancy has been studied in a randomized, double-blind placebo-controlled trial. Patients in the treatment group received 30 mg/day of pyridoxine hydrochloride for 5 days. A significant decrease in post-therapy nausea in the treatment group was noted (14). Similar results were noted for vomiting in another study over a 3-day duration (15). Acupressure at the P6 point located on the wrist has also been studied in a randomized, double-blind placebocontrolled study and found to reduce nausea, but not vomiting, in pregnant patients (16). Sixty women were assigned to two treatment groups: one to a group receiving P6 acupressure, and a control group receiving pressure at another anatomic location. Symptom scores after 5-7 days of treatment were used to judge efficacy. Nausea scores improved over time in both groups, achieving statistical significance in the acupressure group. In another study, 161 pregnant symptomatic women were assigned to three groups: P6 acupressure treatment, placebo (acupressure band placed in an inappropriate location) or control. Improvement in nausea and vomiting or retching was noted in all three groups, with no statistically significant differences noted in the acupressure group (17). 2.2.2 Vertigo Nausea or vomiting associated with vertigo suggests another set of causes. Vertigo is a sensation of the environment spinning around, often described as dizziness by the patient. Evaluation of the dizzy patient begins with a thorough history, which can identify the cause in many patients. If a characteristic change in head position brings on vertigo, benign positional vertigo is usually the cause, which does not usually lead to nausea and vomiting. Associated aural symptoms such as hearing loss, fullness in the ears and tinnitus should be ascertained. Neurologic symptoms such as headache, visual changes or loss of sensation are important to determine. Loss of consciousness associated with vertigo should be determined. Peripheral causes of vertigo, such as benign positional vertigo, vestibular neuronitis, Meniere's disease and acoustic neuroma need to be distinguished from central causes of vertigo, such as multiple sclerosis, brainstem ischemia and central nervous system tumor. The physical examination is often helpful in determining whether a peripheral or central cause of vertigo is present. A complete head and neck exam including examination of the tympanic membranes is advised. Cranial nerves should be tested, including assessment of extraocular muscle function. Nystagmus can aid in diagnosis. Nystagmus of peripheral origin is rotatory or horizontal. Vertical nystagmus is pathognomonic for brain stem disease, as is nystagmus that is more pronounced in one eye. Nystagmus may be tested by having the patient look ahead, then 30 degrees to the left and to the right. Pausing at each position allows evaluation of nystagmus. Induced nystagmus is done by rapidly changing the position of the head. The Hallpike-Dix (or Nylen-Barany) maneuver is performed by making the patient undergo a rapid change from the erect sitting position to a supine position with the head hanging to the left, right or center. A positive test is present when paroxysmal nystagmus is induced after a brief delay. A positive test is diagnostic for either benign positional vertigo, which is seldom associated with nausea and vomiting; or a central nervous system disorder. In order to distinguish the two, the following characteristics of nystagmus are noted. For benign positional vertigo, a 3-20 second latency, rotatory nystagmus and adaptation (i.e. less response to repeat testing) is seen. For a central nervous system cause, no latency is seen, the nystagmus can be vertical or horizontal and can last longer than 60 seconds and there is no adaptation. Balance testing such as the Romberg test and assessment of the gait should also be performed. Vertigo can also be an early symptom in multiple sclerosis. Lesions in the lower midbrain and pons produce internuclear ophthalmoplegia. This is checked for by having the patient follow the finger of the examiner from side to side horizontally. In this type of nystagmus the eye on the side to which the gaze is directed participates strongly with a horizontal nystagmus, whereas the opposite eye will show less nystagmus and weakness of internal rotation. A careful cardiac examination is also necessary, as arrhythmias can produce symptoms which are confused with vertigo (18). Spontaneous and Induced Nystagmus and their Causes Spontaneous Nystagmus Symptom/Sign Peripheral Central Direction Usually horizontalrotatory Never purely vertical Any direction May be purely vertical Direction of fast component Away from side with disease Toward side with disease (or direction changing) Effect of visual fixation Suppressed Not suppressed Usual anatomical Labyrinth or vestibular Brainstem or location of problem nerve cerebellum Induced Nystagmus Feature Peripheral (BPV) Central Time to onset after quick position change (latency) 3-20 seconds Immediate Duration Less than 1 minute Persists longer than 1 minute Fatigability Marked None Vertigo may be a symptom of a more serious underlying disorder , such as vertebro-basilar vascular insufficiency or a cerebellopontine-angle tumor. In order to determine which vertiginous patient needs further diagnostic testing and possible referral, several items in the history are helpful. Are there associated neurologic symptoms such as headache, visual changes or loss of sensation and strength, suggesting cortical or brain stem disorders? Is there a history of seizures? Has the patient lost consciousness with the episode of vertigo? Is there antecedent cranial or cervical trauma? If the answer is affirmative to any of these questions, then empiric therapy is not advised. Referral to a neurologist and possibly a neurosurgeon may be necessary in patients with CNS symptoms suggestive of a brain stem lesion, vertebro-basilar insufficiency or cortical lesions. Additionally, in patients with vertigo associated with seizures, referral to a neurologist is appropriate. If vertigo is associated with syncope, a thorough cardiac evaluation by a cardiologist may be indicated to rule out arrhythmias or other cardiac causes. 2.2.2.1 Vestibular neuronitis The sudden onset of vertigo with nausea and vomiting, increasing in severity over several hours with resolution over a similar span of time, is characteristic of vestibular neuronitis. Patients may awaken from sleep with vertigo. There is often a history of a recent or concurrent upper respiratory tract infection, and clusters of cases may be seen. The etiology is probably viral, and the condition is often diagnosed in adolescents and young adults. Following the acute episode, prolonged dizziness similar to motion sickness may be noted, lasting weeks to months. No new associated auditory deficits, fullness in the ear, or tinnitus are noted. Persistent nystagmus toward the affected side may be noted. Clinical and histopathologic studies implicate an isolated lesion of the vestibular nerve (19). In cases where there is doubt about the diagnosis based on the signs and symptoms, additional diagnostic tests to consider include audiologic assessment, electronystagmography with caloric testing and head CT. Referral to an otolaryngologist should be considered for refractory or atypical cases. Treatment Treatment for nausea and vomiting is symptomatic, similar to that for motion sickness (Table 11). 2.2.2.2 Acute labyrinthitis Acute labyrinthitis symptomatically is similar to vestibular neuronitis, except hearing loss on the involved side is also noted. The cause may be viral, bacterial or due to a toxin (18). A history of recent or concurrent upper respiratory tract infection is often given. Most patients improve over 1-2 weeks, although recurrent episodes have been described. Most report an upper respiratory tract illness 1-2 weeks prior to the onset of vertigo. Several members of the patient's family may be affected, and it is seen more often in spring and early summer. In most cases a viral etiology is likely. A subgroup of patients may have herpes zoster oticus (Ramsay-Hunt syndrome), with vertigo and periauricular vesicles or facial paralysis. Vesicles may be seen on the pinna and on the face in the distribution of the sensory branch of the seventh cranial nerve. Vertigo may last days to weeks. Treatment No specific therapy is recommended. Symptomatic treatment with anti-vertigo medications as for motion sickness may be used if symptoms are severe (Table 11). If there is suspicion of a bacterial etiology, with fever, chills and a purulent middle ear, then medical therapy with antibiotics and possibly surgical therapy is indicated to prevent meningitis. In this case, referral to an otolaryngologist should be considered. For the Ramsay-Hunt syndrome, acyclovir is effective in the treatment of facial paralysis, but is ineffective for vertigo (18). 2.2.2.3 Meniere's disease Severe nausea and vomiting may be a manifestation of endolymphatic hydrops, or Meniere's disease. Symptoms characteristically include episodic aural fullness, tinnitus, hearing loss and vertigo. If vertigo is associated with hearing loss or tinnitus, an audiogram is needed to diagnose Meniere's disease or acoustic neuroma. The onset is abrupt, and usually no precipitating factors are identified. Attacks of vertigo can last a few hours to 24 hours, and subside gradually. Horizontal or horizonto-rotatory nystagmus may be observed. Treatment Treatment is with restriction of salt intake and anti-vertigo drugs. Symptomatic relief of vertigo can be obtained with anticholinergic agents (e.g. scopolamine orally or by transdermal patch), or antihistamines (e.g. diphenhydramine, meclizine or cyclizine). Diazepam 2-5 mg orally q 6-8h is effective in suppressing the vestibular system (Table 11). In severe cases, referral to an otolaryngologist is appropriate. 2.2.3 Motion sickness Motion sickness is a form of physiologic vertigo. Perspiration, increased salivation, yawning and malaise are described by patients with motion sickness. Hyperventilation can lead to hypocapnia, and venous pooling can predispose to hypotension and syncope. The sight and smell of food can exacerbate nausea. Motion sickness is readily diagnosed by history. This is a common syndrome that can occur in an automobile, airplane or at sea. Exaggerated self-generated movement, in fact, can cause motion sickness by forcing rapid and inappropriate changes of vestibular function (20). Treatment The treatment of vertigo associated with motion sickness is empirical (21). Transdermal scopolamine can prevent motion sickness. The patch must be placed several hours prior to the anticipated onset of motion sickness. Antihistamines such as dymenhydrinate, meclizine, cyclizine, promethazine and diphenhydramine can be used (Table 11) The main side effect of this drug class is drowsiness. Acupressure on the P6 point located on the wrist, which has been used in traditional Chinese medicine to treat nausea and vomiting of pregnancy, has been evaluated in a randomized, placebo-controlled double-blind study. Sixty-four subjects were randomly divided into 4 groups (P6 acupressure, dummy-point acupressure, sham P6 acupressure, and control) and subjected to optokinetic drum rotation which elicits motion sickness in normal volunteers. Subjects in the P6 acupressure group reported significantly less nausea and the incidence of gastric tachyarrhythmia was reduced in this group (22). In another blinded placebo-controlled study on 36 patients, however, acupressure provided no protection (23). 2.2.4 Viral syndrome Acute infections with viruses such as Norwalk agent or other enteric viruses can be accompanied by headache, fever, arthralgias and non-bloody diarrhea as well as nausea and vomiting. These symptoms, suggestive of a viral etiology, are an indication that no specific diagnostic testing is necessary. Treatment Empiric therapy with liberal fluid intake, anti-emetics and antipyretics may suffice. Empiric therapy should only be instituted in immunocompetent patients with symptoms that are mild and typical for a viral syndrome. Signs such as protracted fever with chills, bloody diarrhea and clinically evident fluid depletion should be handled with proper diagnostic studies and appropriate specific therapy. A randomized, double-blind comparison of treatment of uncomplicated nausea and vomiting due to viral gastroenteritis with prochorperazine (Compazine) or promethazine (Phernergan) was published. The results showed that prochoroperazine was significantly better in terms of symptom relief compared to promethazine (119). 2.2.5 Post-operative Post-operative nausea and vomiting is common, but is unlikely to be encountered in the primary care setting. In a prospective evaluation of 101 patients admitted for abdominal surgery, the overall incidence of nausea and vomiting was 42% (24). These symptoms are generally attributed to the general anesthetic agents or analgesics used. In the immediate post-operative setting, these patients are often treated empirically. However, the possibility of other causes of nausea and vomiting must be kept in mind. Vomiting in the post-operative period following laparoscopy may lead to pneumomediastinum and bilateral pneumothoraces (25). Congestion of the eye secondary to phakomorphic glaucoma can lead to intractable nausea and vomiting in the post-operative state (26). Treatment While post-operative nausea and vomiting is unlikely to be encountered in the primary care setting, treatment regimens have been studied in this patient population. Therefore, it is useful to be aware of this literature. For example, the efficacy, safety and cost-effectiveness of ondansetron (4 mg intravenously) was compared to droperidol (0.625 mg or 1.25 mg intravenously) in a randomized, double-blind placebo-controlled trial for the prevention of postoperative nausea and vomiting after outpatient gynecologic surgery in 161 women. Droperidol 0.625 mg iv provided antiemetic prophylaxis comparable to that of ondansetron 4 mg iv without an increased incidence of side effects and in the most costeffective manner (27). In another randomized, double-blind, placebo-controlled trial conducted on patients undergoing laparoscopic cholecystectomy, prophylactic anti-emetic therapy with ondansetron, tropisetron, granisetron or metoclopramide was studied. Ondansetron prophylaxis resulted in a lower incidence of post-operative nausea and vomiting compared to metoclopramide or placebo. There were no statistically significant differences among the three 5HT3 receptor antagonists(28). A review of published controlled trials comparing 5-HT3 receptor antagonists to traditional anti-emetic agents (including metoclopramide, perphenazine, prochlorperazine, cyclizine and droperidol) for prophylaxis of postoperative nausea and vomiting showed the 5-HT3 receptor antagonists to be superior (128). 2.3 Diagnostic workup required Experienced physicians triage patients based on the patients history and presentation as well as on clinical instincts that factor in severity of illness and familiarity with the patient (Table 3). Most causes of acute vomiting are selflimited illnesses, but nausea and vomiting can be symptoms of conditions that require expeditious diagnostic workup and treatment (Table 4). Guidelines for referral are included in each section. 2.3.1 Abdominal or chest pain A history of pain may indicate that nausea and vomiting is a consequence of a pathophysiologic process in the thoracic cavity or abdomen. Abdominal pain preceding nausea and vomiting indicates an organic lesion. Pain following vomiting may be due to tenderness of the abdominal musculature, an abdominal wall or esophageal hematoma, (especially in patients who are anti-coagulated) or esophageal perforation. 2.3.1.1 Coronary artery disease Acute and chronic myocardial ischemia, as well as myocardial infarction, may present with nausea and vomiting. These symptoms may be accompanied by abdominal bloating or fullness. Often, concomitant substernal chest pain is present, or the patient may give a history of angina pectoris. Even in the absence of classic signs and symptoms of myocardial ischemia, the physician must keep an open mind to the possibility of a cardiac source of symptoms. At a minimum, an electrocardiogram should be obtained in such patients. Further diagnostic evaluation and therapy depend on the clinical impression. Cardiac enzymes to rule out myocardial infarction and electrocardiographic monitoring may be necessary. Management in consultation with a cardiologist should be considered. 2.3.1.2 Intra-abdominal inflammation A variety of inflammatory conditions within the abdomen may present with nausea and vomiting including cholecystitis, appendicitis, pancreatitis, inflammatory bowel disease, cholangitis and peritonitis. The duration, location, quality, radiation and pattern of abdominal pain, and factors that exacerbate or ameliorate the pain, may help distinguish between these possibilities. A history of biliary colic or gallstones suggests cholecystitis or gallstone pancreatitis. Pain in the periumbilical area which moves to the right lower quadrant over time classically suggests appendicitis. On physical exam, certain findings are suggestive of a particular diagnosis. Murphy's sign (tenderness and inspiratory arrest with palpation in the right upper quadrant of the abdomen) may be elicited in acute cholecystitis. Rebound tenderness on abdominal exam suggests peritonitis, and in the context of free air on X-ray, warrants laparotomy. In acute pancreatitis, diffuse tenderness to palpation of the abdomen may be elicited, making this diagnosis a difficult one to make on physical findings alone (29). Nausea and vomiting in the context of intra-abdominal inflammation are symptoms that should respond to treatment of the underlying inflammatory process. Referral to a gastroenterologist should be considered in severe cases of pancreatitis, in those whom choledocholithiasis is suspected as a cause of pancreatitis or cholangitis, and in cases where the diagnosis is uncertain. For patients with inflammatory bowel disease (IBD) presenting with nausea and vomiting, symptoms may be due to a flare of IBD or the presence of bowel obstruction (see below). Management of IBD with the aid of a gastroenterologist should be considered. Referral to a general surgeon is warranted in cases of acute cholecystitis, appendicitis or peritonitis. 2.3.1.3 GI tract obstruction Obstruction of the stomach or intestine can present with nausea, vomiting and abdominal pain. When abdominal pain precedes nausea and vomiting, obstruction of the GI tract should be strongly considered. Gastric outlet obstruction may be due to peptic ulcer disease in the pyloric channel or duodenal bulb, or benign or malignant gastric tumor. Patients may complain of early satiety and bloating. Abdominal pain is generally postprandial. Symptoms may be worse after a solid meal compared to a liquid one. These symptoms may be resolved with vomiting as the stomach is decompressed. The volume of gastric contents expelled may be large. The vomitus may be foul-smelling, containing food ingested more than 12 hours previously. Heartburn due to reflux of acidic gastric contents may be a complaint. Physical exam findings include a distended abdomen with tympany and, in some cases, epigastric tenderness. A succussion splash heard with the stethoscope after gently rocking the patient from side to side implicates retention of liquid contents in the stomach. Diagnostic tests include upright abdominal X-rays showing an enlarged gas-filled stomach, contrast radiographs and endoscopy. Water soluble contrast X-rays are helpful when a gastric bezoar is suspected, or when a tight stenosis is present. Endoscopy is in many cases the procedure of choice, as histologic diagnosis and in some cases therapy can be provided. Referral to a gastroenterologist is appropriate in cases of acute nausea and vomiting suspected to be due to gastric outlet obstruction. In the small bowel, a history of prior abdominal surgery may predispose to small bowel obstruction caused by adhesions. Eighty percent of small bowel obstructions are due to post-operative adhesions. Other etiologies include primary or metastatic carcinoma, benign tumor, internal and external hernias and Crohns disease. Less commonly, prior abdominal radiation, intussusception, endometriosis, volvulus and congenital abnormalities can lead to small bowel obstruction. The patient can present with intestinal colic, which may be intermittent initially, progressing to sustained abdominal pain centered in the midline of the abdomen at or cephalad to the umbilicus. Vomiting is a cardinal feature, with complete obstruction leading to vomiting of liquid material which may be feculent if the obstruction is in the distal small intestine. Physical findings include a distended abdomen; dilated, palpable loops of bowel; and high-pitched, intermittent bowel sounds. An important aspect of the diagnostic evaluation is the differentiation of incomplete from complete small bowel obstruction. Complete obstruction should be considered if the patient is not able to pass flatus. Abdominal radiographs (supine and upright views) should be obtained. Complete obstruction is suggested by dilated loops of small bowel with air-fluid levels without gas in the large bowel. In partial obstruction, gas is noted in the colon and rectum, although air-fluid levels and dilated loops of small bowel are present. If the differentiation between partial and complete obstruction is still uncertain, contrast radiography may help differentiate these conditions and rule out a paralytic ileus. If the diagnostic evaluation suggests partial obstruction, nasogastric suction and IV fluids should be instituted. Lack of clinical improvement in 48 hours warrants operative treatment. Complete small bowel obstruction is an indication for laparotomy. Resuscitation pre-operatively includes correction of hypoxemia, replacement of intravascular volume and correction of serum electrolyte abnormalities. Primary small bowel malignant tumors presented with abdominal pain (83%), nausea and/or vomiting (54%) and weight loss (53%) in a retrospective review of 69 patients (30). Lymphoma was the most common tumor (42%), followed by adenocarcinoma (38%), carcinoid (10%) and leiyomyosarcoma (10%). In 41%, the tumor was located in the jejunum, in the ileum in 33%, in the duodenum in 22% and in multiple sites in 4%. Of the 65 symptomatic patients, 43% presented as surgical emergencies. Metastases to the GI tract can present with abdominal pain and nausea and vomiting. Melanoma and breast cancer can metastasize to the small bowel. In a review of 68 patients with metastatic melanoma, sites commonly involved were the small bowel (75%), large intestine (25%) and stomach (16%) (31). 2.3.2 Drug, toxin or environmental exposure 2.3.2.1 Drugs as a Cause of Nausea and Vomiting 2.3.2.1.1 Drugs associated with nausea and vomiting at prescribed dosages Many drugs routinely used in clinical practice can cause nausea and vomiting when taken at the prescribed dose. Therefore a careful drug history, including the use of over-the-counter medications and herbal and non-traditional medications, is mandatory. Establishing a temporal relationship between the institution of a medication and symptoms of nausea and vomiting is highly suggestive. Alternatively, changes in dosing or the addition of a drug to an already lengthy list of medications suggests a drug-related effect. A large number of drugs have nausea and vomiting listed as a potential side effect; indeed, almost any drug can potentially cause these symptoms. However, there are certain drugs for which nausea and vomiting is seen in a significant minority of patients. These agents are listed in (Table 5) and are described below. Narcotic analgesics such as morphine, which dramatically decrease gut motility, can lead to constipation and GI tract obstruction. The incidence of narcoticinduced emesis was as high as 40% in one study (32). Prescription and over the counter non-steroidal anti-inflammatory drugs (NSAIDs) have nausea (and less commonly vomiting) as a side effect. Nausea is also seen in up to 40% of patients taking the non-narcotic analgesic tramadol. Theophylline and digoxin can cause nausea and vomiting, especially when plasma drug levels are elevated. Nausea and occasionally vomiting has been noted with the selective serotonin reuptake inhibitors. Chloroquine causes nausea and vomiting as a side effect both at prescribed doses and in overdose situations. Antibiotics and anti-parasitic agents can cause nausea and vomiting. The most common adverse effect of metronidazole is nausea, seen in 12% of patients. Trimethoprim-sulfamethoxazole is associated with nausea and vomiting. Erythromycin can cause nausea and vomiting; the mechanism may be related to its role as an agonist for the pro-motility hormone motilin. Anti-helminthics such as albendazole and thiabendazole have been associated with nausea and vomiting. The amebicide iodoquinol has nausea and vomiting as a side effect. Other drugs which commonly cause nausea and vomiting include estrogens, levodopa, bromocriptine and potassium and iron salts. For the latter two types of agents, gastric irritation may be the mechanism. Timolol eye drops can cause severe nausea and vomiting (115). 2.3.2.1.2 Drugs associated with nausea and vomiting in overdose situations Some drugs may cause nausea and vomiting when excessive doses are ingested, or when serum levels increase due to renal or hepatic insufficiency. Several prescription drug overdoses presenting with nausea and vomiting have been reported, including isoniazid (33), misoprostol (34), colchicine (35) and metronidazole. Cinchonism secondary to quinine toxicity classically presents with nausea, vomiting, and tinnitus. Prolongation of the Q-T interval is often noted (36). Specific overdose situations which are known to present with nausea and/or vomiting are listed in (Table 6) (37). This list is not comprehensive; communication with a Regional Poison Control Center for up-to-date management recommendations should be considered. 2.3.2.2 Chemotherapeutic agents These drugs are notorious for their emetogenic properties. In the context of chemotherapy regimens, anti-emetic therapy is often prescribed. While this situation is unlikely to be encountered in the primary care setting, it is important to keep this possibility in mind. In particular, anticipatory nausea and vomiting may develop in a patient who has undergone prior chemotherapy. In a study of 16 adult cancer patients with chemotherapy-induced anticipatory nausea and vomiting, hypnosis was shown to be highly effective (130). In all patients studied, anticipatory nausea and vomiting disappeared. The severity of chemotherapy-induced emesis depends on the particular drug used (cisplatin is associated with the highest incidence), the dose of the drug and the method of administration (38). Vomiting may be delayed 2 to 5 days after cisplatin administration and may be difficult to control. Nausea and vomiting may also be encountered in the setting of fractionated radiotherapy for malignancy (39). An overview of the treatment of patients with chemotherapy-induced nausea and vomiting is found in the section on drug therapy. 2.3.2.3 Alcohol (Ethanol) Excessive alcohol intake may cause severe nausea and vomiting. MalloryWeiss tears are directly caused by vomiting or retching and can be encountered in the patient who has been drinking alcohol. Acute pancreatitis may be present and leads to nausea, vomiting and abdominal pain. Intracranial hemorrhage secondary to head trauma from a fall in an inebriated patient can cloud the clinical presentation, as increased intracranial pressure can itself be a cause of nausea and vomiting. Alcoholic hepatitis can also present with nausea and vomiting. Nausea and vomiting in the patient with a history of alcohol use therefore requires vigilance for these associated conditions. A history obtained from family members or witnesses, a careful abdominal exam, head/eyes/ears/nose/throat exam and neurological exam, measurement of blood alcohol levels, hematocrit, coagulation profile, transaminases (AST/ALT) and serum amylase and lipase should be obtained in a patient suspected of heavy alcohol use who presents with severe nausea and vomiting. Ancillary diagnostic tests such as chest and abdominal X-rays and a head CT scan may be necessary to rule out the wide variety of associated conditions that can lead to nausea and vomiting in the patient who presents after heavy alcohol consumption (Table 7). 2.3.2.4 Environmental toxins and exposures Exposure to certain environmental toxins can lead to nausea and vomiting as prominent symptoms. Carbon monoxide intoxication presents in a non-specific manner. Headache, dizziness, fatigue and nausea and vomiting are common (40). In addition, disturbed judgment and diminished visual acuity may be seen. Blood carboxyhemoglobin levels of 40-60% are associated with tachypnea, tachycardia, ataxia, syncope and seizures. The EKG may show ST segment changes, conduction blocks and atrial or ventricular arrhythmias. Cherry-red coloration of the lips or skin is rare. Treatment consists of supportive care and 100% oxygen. Carboxyhemoglobin levels should be measured every two to four hours, and oxygen continued until blood levels are less than 10%. Hyperbaric oxygen (3 atm) is recommended for patients who present with neurologic signs or symptoms, EKG changes consistent with ischemia, shock, severe metabolic acidosis and pulmonary edema. Acute arsenic poisoning can present with nausea and vomiting (41). Acute fluoride poisoning from a public water system produced a clinical syndrome characterized by nausea, vomiting, diarrhea, abdominal pain and paresthesias (42). Pesticide exposure can present with anxiety, vertigo, nausea, vomiting, tearing and weakness (43). Elemental mercury vapor toxicity presented with nausea, headache, lumbar pain and shortness of breath at rest (44). In each of these examples, nausea and vomiting were present in the majority of cases but the presenting symptom complexes were non-specific. Food poisoning due to pre-formed bacterially-derived toxins can present with nausea and vomiting in association with abdominal pain and diarrhea. Staphylococcal food poisoning typically presents with nausea, vomiting, cramping abdominal pain and diarrhea between two and four hours after ingestion of food contaminated by the enterotoxin produced by Staphylococcus aureus . Often, a cluster of cases is identified. Treatment is symptomatic. The illness is short, rarely lasting more than 24 hours. Vibrio parahemolyticus poisoning is associated with the consumption of raw or improperly refrigerated seafood. The incubation period is between 12 and 24 hours, and patients present with explosive watery diarrhea, nausea, vomiting and abdominal cramps. Treatment is supportive, although in protracted cases, antibiotic therapy with tetracycline or ampicillin may be used. Other bacterial causes of food poisoning such as Clostridium perfringens type A and Bacillus cereus cause nausea and vomiting as predominant symptoms in a minority of patients. Toxin exposure can occur by consumption of seafood or exposure to marine toxins. Scombroid poisoning by the consumption of spoiled fish of the dark meat varieties can present with skin rash, diarrhea, palpitations, headache, nausea, abdominal cramps, paresthesias, an unusual taste sensation and breathing difficulties. Patients respond to anti-histamines as the toxin is histamine (45, 46). Cigatuera poisoning, seen predominantly in tropical areas, presents with nausea, abdominal pain, vomiting and diarrhea. Peripheral neuropathic symptoms are also characteristic, including paresthesias, dental discomfort and confusion of peripheral hot and cold sensation. Treatment is symptomatic. Although not toxins, certain foods can cause hypersensitivity reactions which present with nausea, vomiting, abdominal pain and diarrhea (47). Certain envenomations can present as nausea and vomiting. Spider bites, particularly by the female black widow spider or brown recluse spider, can present with nausea and vomiting. Likewise, scorpion stings and snake bites can present with nausea and vomiting. In all of these cases, pain, erythema and swelling at the site of the bite is usually evident. Unusual examples of envenomations which present with nausea and vomiting are those due to the bite of the Gila monster (48) and the sting of the Portuguese man-of-war (49). Certain environmental exposures can lead to nausea and vomiting. Heat exhaustion occurs in an unacclimatized person who exercises on a hot day. It results from loss of salt and water, with the patient complaining of headache, nausea, vomiting, dizziness, weakness, irritability, cramps or diaphoresis. Therapy consists of rest in a cool environment, and volume repletion with saltcontaining solutions. If vomiting is present, IV normal saline may be necessary. High altitude illness can occur in people unacclimatized to altitude who ascend to more than 2000 meters in less than 1-2 days. Acute mountain sickness presents with headache, nausea, vomiting, anorexia, dyspnea, lethargy, sleep disturbance, vertigo, palpitations and difficulty concentrating. Treatment consists of liberal fluids, mild analgesics for headache, prochlorperazine for nausea, and for severe symptoms, oxygen at 2-3 liters /minute and descent of 1000-1500 meters. 2.3.3 Late pregnancy If the patient is pregnant, nausea and vomiting of pregnancy, especially early in gestation, is common and is a self-limited and benign condition. In the third trimester of a normal pregnancy, the incidence of nausea and vomiting decreases (50). If nausea and vomiting in the pregnant woman does not fit this typical pattern, then the following conditions should be considered. If symptoms are severe, or begin in the second or third trimester, then other more serious conditions need to be considered. For each of the conditions described below, management along with an obstetrician should be considered (Table 8). 2.3.3.1 Hyperemesis gravidarum If vomiting is protracted such that fluid and electrolyte disturbances or nutritional deficiency develops, then the condition is termed hyperemesis gravidarum. Onset of symptoms is often soon after the first missed menstrual period. Classically the vomiting disappears during the third month, and rarely persists into the fourth month. Patients with hyperemesis gravidarum do not have an increased incidence of toxemia of pregnancy or spontaneous abortion, and their babies are not underweight or otherwise affected. In one study, however, intrauterine growth retardation in patients with hyperemesis gravidarum was reported (51). Women with twins or with molar pregnancy (hydatidiform mole) have an increased incidence of hyperemesis gravidarum. These women have elevated concentrations of human chorionic gonadotropin (HCG). Abnormalities of thyroid function tests are also common. The metabolic consequences of hyperemesis gravidarum can be severe due to dehydration and muscle wasting, with mortality increased in untreated patients. Gastric emptying is not delayed in patients with hyperemesis gravidarum, suggesting that the disorder is not due to an upper GI tract motility disturbance (122). Treatment Treatment is directed at fluid and electrolyte replacement and supportive psychotherapy (11). Parenteral nutritional therapy may be necessary. Standard anti-emetics are generally not effective. Successful management with intravenous hydrocortisone, followed by oral prednisolone has been described in a series of seven patients (52). The combination of intravenous droperidol and diphenhydramine was shown to improve symptoms (53). A placebo-controlled, randomized single-blind study of manual acupressure for the treatment of hypermesis gravidarum performed in 33 women showed that nausea and vomiting was reduced in the acupressure group compared to the placebo group (121). 2.3.3.2 Acute fatty liver of pregnancy This is a serious condition of unknown etiology, occurring in 1:13,000 deliveries. Symptoms of nausea, vomiting, headache and malaise begin in the third trimester, usually around week 35. Features of pre-eclampsia (hypertension, edema, proteinuria) may be present. The disease often progresses to hepatic failure complicated by disseminated intravascular coagulation. If nausea and vomiting begin in the latter part of pregnancy, serum aminotransferase activity (AST/ALT) should be measured. Elevated aminotransferases in the 200-500 range is an indication for liver biopsy. The characteristic finding on biopsy is microvesicular fat. Maternal morbidity is high, and the condition should be suspected in patients with symptoms of pre-eclampsia with hypoglycemia, low fibrinogen and prolonged prothrombin time (54). Treatment Once this diagnosis is established, early delivery is indicated to prevent maternal and fetal death (55). Management by an obstetrician, and referral to a center specializing in high-risk obstetrics should be considered. 2.3.3.3 HELLP Syndrome A syndrome of hemolysis, elevated liver enzymes and low platelet count can complicate pre-eclamptic/eclamptic patients. Patients typically present in the third trimester with epigastric or right upper quadrant pain and nausea and vomiting. They may present with no signs of pre-eclampsia (hypertension, proteinuria, or edema), and therefore a non-obstetric diagnosis may be entertained (56). Treatment Management in conjunction with an obstetrician is recommended, and referral to a center specializing in high-risk obstetrics should be considered. 2.3.4 CNS symptoms Headache, projectile vomiting often in the morning without antecedent nausea, a history of migraine, transient ischemic attacks, vertigo, photophobia or neck stiffness are elements of the history which should direct the clinician to a CNS explanation for nausea and vomiting. Headache may be due to migraine, increased intracranial pressure or cerebral vascular hemorrhage. The clinical diagnosis of migraine is based on headache characteristics and associated symptoms, particularly nausea and vomiting. The treatment of migraine has been recently reviewed (57). Treatment strategies include 5-hydroxytryptamine agonists, ergotamine tartrate, sumatriptan, dihydroergotamine, NSAIDs and opiates. Sumatriptan, a selective serotonin receptor agonist, is particularly effective and well-tolerated (58) (59). Treatment with oral sumatriptan has been studied in a randomized double-blind placebocontrolled study, and found to be effective (60). Headache in the presence of fever and neck stiffness suggests meningitis (61). Nausea and vomiting may be a feature of meningitis. Cerebral cysticercosis can present with positional headache and nausea and vomiting (62)(116). Primary intraventricular hemorrhage presented with nausea and vomiting in 71% of cases in a review of 14 cases. Headache and mental status changes were noted in an equal number of cases (63). Referral to a neurologist or neurosurgeon may be necessary. Vertebrobasilar vascular insufficiency is a common cause of vertigo in the elderly. Vertigo is abrupt in onset, lasts several minutes and is often associated with nausea and vomiting. Associated symptoms due to ischemia in the territory of the posterior circulation include visual hallucinations, drop attacks, diplopia, headache and visual field defects. CT scans are usually normal, as symptoms are transient. Angiography may be helpful, but carries a risk of arterial spasm and stroke. Referral to a neurologist should be considered. Vertigo with nausea and vomiting may also accompany infarction of the lateral brain stem or cerebellum or both. Key findings are an acute onset of symptoms, clear cerebellar signs such as extremity and gait ataxia and gaze-evoked nystagmus. These patients must be carefully observed for the development of progressive brain stem dysfunction due to edema at the site of infarction. Consultation with a neurologist should be obtained. Cerebellopontine-angle tumors, such as acoustic neuroma, meningioma and epidermal cysts grow slowly, so that acute vertigo with associated nausea and vomiting are rarely presenting symptoms. Occasionally, acute onset of vertigo may be present. Unilateral, progressive hearing loss is present, identified by an abnormal brain-stem auditory evoked response. Evaluation by magnetic resonance imaging (MRI) is the most sensitive study. Every patient with vertigo and a unilateral hearing loss or tinnitus must be assumed to have a retrocochlear lesion until radiographically proven otherwise (18). Treatment is surgical removal, so that referral to an otolaryngologist or neurosurgeon is indicated. 2.3.5 Infections as a Cause of Nausea and Vomiting Infections may present with nausea and vomiting, especially if viral in origin. Nausea and vomiting accompanied by diarrhea and fever suggests viral gastroenteritis. Often, this is self-limited, and patients recover with supportive care. Occasionally, volume depletion is severe, and may require volume replacement. Blood in the stool and fever warrants further investigation and may indicate inflammatory bowel disease or bacterial enteritis or colitis. Certain other infections of the upper GI tract of non-viral etiology, although rare, should be considered. Esophageal infections are more commonly seen in immunocompromised patients, and can present with nausea and vomiting alone, although most patients will develop esophageal symptoms such as dysphagia and odynophagia. For immunocompromised patients, the most common pathogens are Candida, CMV and HSV (64). Gastric syphilis has become an uncommon disease, with only 24 cases reported in the literature in the past 2 decades. The most common symptoms in a review of 7 cases were abdominal pain, nausea, and vomiting, with signs of syphilis present in 5 patients. The diagnosis was established by identification of spirochetes on mucosal biopsy in 6 patients. The diagnosis should be considered in patients at risk for sexually transmitted disease who complain of nausea, vomiting and abdominal pain and in whom unusual gastric lesions or ulcers are refractory to therapy (65). Unusual infections such as Rocky Mountain Spotted Fever can present with nausea and vomiting, along with fever, headache, myalgia and anorexia. These symptoms can be difficult to distinguish from self-limited viral infection. A rash may appear later in the course, but is not pathognomonic (66). Hepatic abscess presented with nausea and vomiting in 40% of cases in a review of 35 patients. Twenty-nine patients had bacterial abscesses, and 6 had amebic abscesses. Fever was present in 95% and right upper quadrant pain in 63% of patients (67). 2.3.6 Systemic disease as a cause of nausea and vomiting Acute nausea and vomiting may be the manifestation of a definable disease process. While diseases such as diabetes mellitus, endometriosis and renal insufficiency are chronic in nature, acute exacerbations may lead to presentations that include nausea and vomiting. Endocrine emergencies can present with nausea and vomiting. Diabetic ketoacidosis can present with vomiting, along with polyuria, polydypsia, abdominal pain and changes in mental status. Ninety percent of patients are known diabetics. The smell of acetone on the patient's breath, and the deepbreathing pattern of Kussmaul's respiration aid in the diagnosis (68). Likewise, severe vomiting and abdominal pain are central clinical features of alcoholic ketoacidosis. As in diabetic ketoacidosis, severe dehydration can lead to Kussmaul's respiration and mental status changes (69). Acute adrenal insufficiency usually presents with nausea, vomiting, severe hypotension and dehydration (70). Nausea and vomiting are common in the uremic patient (71). Intestinal endometriosis can present with abdominal pain and nausea and vomiting. In a review of 26 cases, abdominal pain was the main presenting feature in 20, with associated nausea and vomiting in 12. Establishing the diagnosis preoperatively was difficult in patients without a known history (72). 2.3.7 Immunosuppression The immunosuppressed patient can be considered in a separate category because such patients deserve a thorough diagnostic workup even if signs and symptoms initially point to a benign self-limited condition as the cause. The classic situation is the patient with AIDS, although immunosuppression due to drugs and severe illness need to be considered. While the cause of nausea and vomiting may be similar to those seen in immunocompetent patients, several other etiologies need to be considered. Chiefly, opportunistic infections of the upper GI tract, such as Candida esophagitis, CMV or HSV infection (73) may be present. While nausea and vomiting are rarely the sole symptoms seen in these situations, other more typical symptoms such as odynophagia or dysphagia, hematemesis and weight loss may be accompanied by nausea and vomiting. For these patients, referral to a gastroenterologist for endoscopy to establish the diagnosis should be considered, especially if an empiric trial of therapy (e.g. fluconazole for presumptive Candida esophagitis) is unsuccessful. 2.3.8 Unusual causes and consequences There can be unusual causes or consequences of nausea and vomiting. This question should be asked by the examiner if the patient does not fit a typical profile in terms of symptoms, or if an unusual complaint arises as a consequence of vomiting. There are several consequences of nausea and vomiting which are rare but should be considered. Visual floaters may be due to vitreous hemorrhage and retinal vein rupture caused by emesis (74). Stress fracture of the hyoid bone caused by induced vomiting has been described (75). Tooth surface enamel loss may occur with repeated emesis (76). Benign retropneumoperitoneum can be induced by vomiting (77). Likewise, unusual causes of nausea and vomiting have been described. Systemic mastocytosis can present with nausea due to mast cell infiltration of the gastric mucosa (78). Visually induced paroxysmal nausea and vomiting can be the presenting manifestation of multiple sclerosis (79). Acquired or hereditary angioedema can present with gastrointestinal complaints including episodic nausea (80). Gastric outlet obstruction may occur due to a giant duodenal gallstone. This condition is called Bouveret's syndrome, and often indicates the presence of a cholecystoduodenal fistula (81). Emesis of gallstones has been described, indicative of a fistula between the gallbladder and the stomach or duodenum (82). 3.0 Chronic nausea and vomiting Chronic nausea and vomiting is defined as the presence of symptoms for over a week. The patient may describe intermittent symptoms lasting months or years. A number of different conditions may be responsible for such symptoms, and a thorough history and physical exam are invaluable in pointing to the correct diagnosis. 3.1 The cause is known from prior workup In certain situations of chronic or recurrent nausea and vomiting, the cause has been established on previous diagnostic workup. In these situations, treatment may be instituted without extensive diagnostic workup, although the physician must keep an open mind regarding alternative etiologies. If the patient does not respond to specific therapy, further diagnostic studies should be initiated. 3.2 The cause is not known If no prior diagnosis or underlying etiology is evident, the patient with chronic or recurrent nausea and vomiting requires a diagnostic work-up. Conditions such as the post-gastrectomy state, diabetes mellitus leading to gastroparesis and prior abdominal surgery can predispose to recurrent nausea and vomiting. Knowledge of the underlying condition aids the physician in fashioning a diagnostic and treatment plan. In this situation, a full diagnostic workup may not have been performed in the past despite the chronicity of symptoms. If such is the case, the history, physical examination, screening laboratory tests and abdominal X-rays (supine and upright) are the first steps in the diagnostic workup. Diagnostic tests useful in the evaluation of the patient with chronic nausea and vomiting are outlined in (Table 9). Some of the causes of chronic nausea and vomiting are rare, and referral for specialized diagnostic testing may be necessary. Certain conditions prompt referral to a gastroenterologist (Table 12). 3.2.1 The gastrointestinal tract is involved Chronic nausea, accompanied in a subset of patients by vomiting, can be due to a variety of gastrointestinal causes. Achalasia, esophageal masses, peptic ulcer disease, gastroparesis, occult gastrointestinal cancer, intestinal pseudoobstruction and gastroesophageal reflux disease are examples of gastrointestinal diseases that can present with nausea with or without vomiting. 3.2.1.1 GI tract obstruction GI tract obstruction needs to be ruled out early in the diagnostic workup, and this can be accomplished initially by supine and upright abdominal X-rays, followed by contrast studies if indicated. GI tract obstruction can lead to acute nausea and vomiting. If abdominal pain precedes nausea and vomiting, obstruction of the GI tract should be strongly considered. Gastric outlet obstruction can be caused by peptic ulcer disease, particularly in the pyloric channel or duodenal bulb. Tumor and bezoar formation are less common reasons for gastric outlet obstruction. Other causes of GI tract obstruction such as small bowel obstruction and stricture formation (e.g. with Crohns disease) need to be considered. A history of prior gastric resection is associated with nausea and vomiting, often presenting many years following the surgery date. Vomiting of bile may be noted. Vagotomy with partial gastrectomy with Billroth I or II anatomy can predispose to obstruction. Roux-en-Y gastrojejunostomies can lead to altered gastric emptying rates, manifesting as nausea and vomiting. The Roux stasis syndrome, characterized by abdominal discomfort, nausea, vomiting or bezoar formation was noted in 6% of 20 patients following Roux-en-Y gastrojejunostomy (83). A prior fundoplication can lead to distal esophageal obstruction leading to vomiting with associated dysphagia. Nausea has been described following laparoscopic fundoplication (84). In each of these situations, contrast studies help in defining the altered anatomy, and endoscopic examination allows mucosal lesions to be identified and appropriately treated. Referral to a gastroenterologist, and in some cases to a surgeon, is necessary in many of these patients. Other causes of nausea and vomiting involving the GI tract include esophageal lesions such as achalasia or esophageal masses that may cause obstruction to the passage of food. Regurgitation of undigested food, rather than true vomiting, may be the presenting complaint. Dysphagia, with or without odynophagia, is usually part of the patient's complaints. Referral to a gastroenterologist for endoscopy, biopsy and management is indicated for these disorders. 3.2.1.2 Other GI causes Certain situations where GI causes of nausea and vomiting are present without evidence of mechanical obstruction also need to be considered. Chronic intractable nausea can be the primary symptom of gastroesophageal reflux disease. In a study of 10 outpatients with this symptom, acid reflux was the cause of intractable nausea in all patients. In this group of three men and seven women, the average duration of nausea was 2 years, with a range of 3 months to 6 years. None had responded to empiric therapies for nausea. Either upper endoscopy or 24 hour esophageal pH studies showed gastroesophageal acid reflux in all patients. Esophagitis was documented on upper endoscopy in 5 patients; and in the 6 patients who had esophageal pH testing, abnormally increased acid reflux was documented. Treatment included omeprazole, ranitidine or cisapride; one patient who did not respond to high dose H2 blocker or proton pump inhibitor therapy underwent Nissen fundoplication. Treatment of gastroesophageal reflux led to symptom resolution in all patients (85). With a mean follow-up of 6 months, all patients reported no recurrence of nausea. Chronic peptic inflammation due to peptic ulcer, gastritis or Zollinger-Ellison syndrome can present with nausea and vomiting. Helicobacter pylori infection leads to chronic gastritis and has been associated with gastric and duodenal ulcers. Nausea and vomiting can be associated symptoms of ulcer disease. Patients with recurrent vomiting and suspected peptic ulcer disease should undergo endoscopy to evaluate this possibility. The diagnosis of H pylori infection can be established via several methods. H pylori serology provides evidence of exposure to the organism. Breath testing and a stool antigen test are available to non-invasively determine whether active infection is present. Endoscopy with biopsy of the antrum to demonstrate the organism is the gold standard, and should be considered in cases where peptic ulcer disease is a diagnostic consideration. A rapid urease enzyme test may be used concurrently with biopsy. Once the presence of the organism has been established, and the symptoms and clinical picture are deemed suitable for treatment, several drug combinations are available. Eosinophilic gastroenteritis is characterized by peripheral eosinophilia, eosinophilic infiltration of the GI tract and symptoms referable to the GI tract including abdominal pain, nausea, vomiting, diarrhea, anemia and protein-losing enteropathy. Peripheral eosinophilia is not an invariable finding. In a review of 8 patients, the diagnosis was established by endoscopic mucosal biopsy in 5 and by laparotomy with full-thickness biopsy in the remainder. Patients were treated with prednisone with response in all patients (86, 87). Infiltrative lesions of the stomach (linitis plastica) can present with early satiety and nausea and vomiting. Pancreatic cancer can lead to gastroparesis and nausea and vomiting. Nausea and vomiting may be caused by disorders of gastric motility without obstruction or evidence of inflammation. Gastroparesis is the most common of these motility disorders. In most cases, the diagnosis is made clinically, in the absence of mechanical lesions causing obstruction of the GI tract. Scintigraphic gastric emptying studies are the gold standard (88, 89). In difficult to treat cases, the patient may be referred to a gastroenterologist at a tertiary care center. Esoteric tests such as antroduodenal motility tests and electrogastrography may be used to document slowed gastric muscular activity. Treatment of gastroparesis includes dietary measures, such as maintaining adequate hydration, eating small frequent meals, and avoiding fatty foods and indigestible solids. Pharmacologic therapy includes antiemetics as well as prokinetic agents. Prokinetic agents such as metoclopramide and cisapride have been used to treat this disorder (90). Domperidone has also been shown to enhance gastric emptying. Erythromycin in low, prokinetic doses (250 mg PO TID 30 minutes before meals) may also be tried. Usually prokinetic agents are given 15 to 30 minutes prior to meals to enhance the effect on gastric emptying at mealtime. A bedtime dose may help in emptying the stomach of indigestible solids and thereby prevent bezoar formation. 3.2.2 The nervous system is involved Nervous system causes of chronic nausea and vomiting include organic brain disease, often manifesting with focal neurologic signs; autonomic nervous system diseases; and degenerative neuromuscular diseases of the gut. 3.2.2.1 Focal neurologic signs are present Central nervous system (CNS) causes of vomiting may be due to stimulation of the emetic center in the medulla oblongata. It may be seen in patients with brain lesions, increased intracranial pressure, hydrocephalus, vestibular disorders and posterior cranial fossa lesions. Metabolic-induced and druginduced vomiting are partially mediated by the CNS through stimulation of the chemoreceptor trigger zone in the floor of the fourth ventricle (area postrema). A thorough neurologic exam is critical to rule out CNS lesions, and includes testing of cranial nerves, vestibular function and pupillary function. The presence of peripheral neuropathy and extrapyramidal signs should be ascertained. Imaging studies of the head (CT or MRI) are important diagnostic studies to rule out CNS lesions. For vertiginous symptoms, referral to an otolaryngologist and consideration for electronystagmography is appropriate. Treatment will depend on the diagnosis. Conditions such as increased intracranial pressure, intracranial bleed and intracranial or posterior fossa tumor indicate the need for referral to a neurologist or neurosurgeon. 3.2.2.2 The autonomic nervous system is involved Disorders of autonomic supply may alter gut motility and result in vomiting. Autonomic system degenerations such as idiopathic orthostatic hypotension, as well as diseases causing autonomic neuropathy such as diabetes mellitus, may produce motility disturbances in the gut. Signs of autonomic neuropathy such as orthostatic hypotension, absence of sweating and absence of pulse and blood pressure responses to Valsalva maneuver should be sought. Chronic nausea and vomiting is encountered in the diabetic patient. 3.2.2.3 Degenerative neuromuscular diseases of the gut Motility disturbances in the GI tract can lead to acute presentations mimicking that of GI tract obstruction. Most of the neuromuscular disorders are uncommon. Neuromuscular diseases of the GI tract such as intestinal pseudo-obstruction and hollow visceral neuropathy or myopathy may alter the muscle of the intestinal wall or the nerves of the myenteric plexus or both. Patients can present with chronic unexplained abdominal pain, abdominal distention and bloating, early satiety, nausea, vomiting and alterations in bowel habits (91) (92). Both purely myogenic (familial visceral myopathy, somatovisceral myopathy, scleroderma) and purely neurogenic motility disorders (von Recklinghausens disease or Chagas disease) exist. Mixed conditions also exist. For example, in amyloidosis the lesion may be an infiltration of muscle and nerve. Nausea and vomiting are frequent but not invariable features of gut motility disorders. The area of the gut involved is important in determining the predominant clinical presentation: whereas gastroduodenal motility disorders often cause nausea and vomiting, the predominantly intestinal motility disorders (chronic intestinal pseudo-obstruction syndrome) may present as abdominal distension, pain and disturbances of bowel movement often without recurrent vomiting. Intestinal pseudo-obstruction caused by paraneoplastic syndromes can also present with nausea and vomiting. For the diagnosis of neuromuscular causes of nausea and vomiting, referral for specialized testing may be necessary, especially in those patients with longstanding symptoms who remain undiagnosed and who do not respond to therapeutic trials. Mechanical causes of GI tract obstruction should be ruled out with contrast studies or endoscopy. While radionuclide studies may document delayed gastric emptying, the precise etiology for such an abnormality in the nondiabetic patient will not be known. Esophageal, antro-duodenal or anorectal manometry may be useful to document altered GI tract motility; however, the precise etiology behind such abnormalities will not be known. In these situations, referral for specialized studies is appropriate. Tests such as small bowel manometry and electrogastrography may prove useful. In a small number of cases, laparotomy with full thickness small bowel biopsy may be necessary in order to arrive at a diagnosis. 3.2.3 Endocrine or metabolic cause Endocrine and metabolic causes can lead to chronic nausea and vomiting. The classic situations are the patient with diabetes mellitus, the patient with adrenal insufficiency and the patient with hypercalcemia. 3.2.3.1 Diabetes mellitus Nausea and vomiting, often accompanied by weight loss and early satiety, are common gastrointestinal symptoms in patients with diabetes. Episodes of nausea and vomiting may last days to months or occur in cycles (89). About half of patients with insulin or non-insulin-dependent diabetes have delayed gastric emptying (diabetic gastroparesis). Some complain of epigastric pain, nausea, vomiting or postprandial fullness. Bezoars may form in the stomach, leading to gastric outlet obstruction exacerbating the underlying gastroparesis. Diabetic gastroparesis may contribute to inadequate glycemic control and impaired absorption of orally administered drugs. Although less common, gastric emptying rates may be accelerated in diabetics as well (93). 3.2.3.2 Adrenal insufficiency Adrenal insufficiency presents with nonspecific symptoms such as weakness, fatigue, nausea, vomiting, anorexia and weight loss. It should be suspected if the patient has hyperpigmentation, hyponatremia and/or hyperkalemia; a history of autoimmune disease such as hypothyroidism or diabetes; or recent use of corticosteroids (70). Gastric stasis has been demonstrated in a patient with primary adrenal insufficiency (94), and therefore this diagnosis should be considered in patients presenting with chronic nausea and vomiting. The short cosyntropin (Cortrosyn) stimulation test (250 ug IV or IM, with measurement of plasma cortisol 30 minutes later) is diagnostic, with a normal response being stimulated plasma cortisol greater than 20 ug/dl. With the diagnosis of adrenal failure, therapy with hydrocortisone 100 mg IV q 8h should be given, along with normal saline with 5% dextrose until hypotension is treated. Maintenance therapy with prednisone is required. 3.2.3.3 Hypercalcemia Hypercalcemic states can alter gut motility and present with nausea and vomiting. GI symptoms of severe hypercalcemia (serum calcium > 12 mg/dl) includes nausea and vomiting, as well as anorexia, constipation and abdominal pain. Neurologic symptoms include such as weakness, fatigue, confusion, stupor and coma; renal effects such as polyuria and nephrolithiasis may be seen. Dehydration resulting from nausea and vomiting and anorexia can lead to even more severe hypercalcemia (95). Serum ionized calcium is a better indicator of true hypercalcemia, as total serum calcium levels are linked to serum albumin levels. Primary hyperparathyroidism and malignancy are the two most common causes of hypercalcemia. Treatment of the underlying cause, as well as treatment of the hypercalcemia with extracellular volume restoration, saline diuresis and treatment with bisphosphonates should be instituted when appropriate. 3.2.4 Psychogenic causes Repetitive vomiting may be a conscious and voluntary act as in patients with bulimia who vomit in part to control their weight. In rumination, the patient increases intraabdominal pressure, regurgitates food into the mouth and swallows it again. At a more subconscious level, vomiting may occur in otherwise healthy persons as part of a strong emotional reaction, and in patients as an expression of an underlying psychopathologic condition or as a conversion reaction. In the diagnostic workup of psychogenic vomiting, a thorough history including a family and social history are important. Volume depletion and signs of nutritional deficiencies should be sought on physical examination. A complete neurologic exam should be performed. Depression, weight loss and altered perception of body image suggest anorexia nervosa. Excessive concern with body weight, loss of dental enamel, parotid hypertrophy, electrolyte disturbances and chronic diarrhea indicate bulimia (96). Almost 50% of bulimics report nausea and other gastrointestinal symptoms (97). Formal psychiatric testing including inpatient evaluation and assessments such as the Minnesota Multiphasic Personality Inventory should be considered. These types of tests may be helpful if an abnormality in the hypochondriasis, depression or hysteria scales is found. Referral to a psychiatrist should be considered. Often, psychogenic causes of nausea and vomiting are diagnoses of exclusion. Recently, however, hypomotility in the gastric antrum, abnormal gastric electrical activity and delayed gastric emptying have been reported in patients thought to have psychogenic nausea and vomiting. Psychologic stress may in fact lead to vomiting in otherwise normal people (98). In patients with functional nausea and vomiting, tricyclic antidepressants at low doses may be of benefit. In a retrospective analysis of 37 such patients treated with amitriptyline, desipramine, nortriptyline doxepin or imipramine, symptomatic response was documented in 84% of the patients. Dose at response averaged 50 mg/day, and the outcome was not related to the tricyclic antidepressant used (117). Panic disorder has been associated with nausea (99). Patients with borderline personality disorder can present with episodic vomiting (100). Social phobia may manifest as nausea and fear of eating in public (101). The cyclic vomiting syndrome is characterized by recurrent, self-limited episodes of nausea and vomiting separated by symptom-free intervals. In a report of 71 cases, the length and symptomatology of episodes were stereotyped and characteristic for each patient (102). There was a coincident relationship with migraine and irritable bowel syndrome. Patients could identify conditions that precipitated episodes, commonly heightened emotional states and infections (103). While all patients in the series were children, a case in a 65-year old diabetic woman with a 10 year history of recurrent nausea and vomiting was reported (104). Episodes of vomiting were always characterized by elevations in serum ACTH, serum cortisol and urinary cortisol. However, suppression of these elevations with dexamethasone did not alleviate the clinical symptoms. Intramuscular ketorolac produced prompt and sustained relief. A review of 17 adult patients with cyclic vomiting syndrome who had been treated with tricyclic antidepressants was published (118). Symptoms began at age 35 (range 14-73 years). The average duration of each episode was 6 days (range 121 days). The symptom-free interval averaged 3.1 months (range 0.5 to 6 months). Fewer than a third of the patients reported a prodrome or triggering events. Tricyclic antidepressant therapy led to complete remission of symptoms in 17.6% of patients, and partial response in 58.5% of patients. 3.2.5 No cause found despite thorough investigation Finally, there may be patients in whom no etiology can be determined despite extensive diagnostic testing. In this group of patients, a gastric emptying study should be performed (105). If the emptying study is abnormal, a trial of a prokinetic agent such as metoclopramide may be useful. In cases of intractable gastroparesis, placement of gastrostomy tubes and jejunostomy tubes for decompression and feeding respectively may be effective (106). Prior to the institution of these measures, the patient should be considered for referral to a tertiary care center for further testing, including electrogastrography and small bowel motility studies. If the gastric emptying study is normal, then consideration can be given to laparotomy with full thickness biopsy of the small intestine to rule out a neuropathic or myopathic disorder. Such an invasive approach should be considered in the rare patient in whom vomiting is severe and has led to nutritional compromise or to severe disruption of quality of life. 4.0 Drug Therapy for Nausea and Vomiting 4.1 Classes of Drugs The following is a brief summary of the drugs used to treat nausea and vomiting, including indications, contraindications and potential adverse reactions. For most of these agents, safety for use in pregnancy has not been established. Whenever possible, the potential benefits must be weighed against potential adverse effects. This is not a comprehensive list of potential uses and adverse effects. For detailed information regarding these drugs, the package insert should be consulted prior to prescribing. A summary of anti-emetic agents is provided in (Table 11). 4.1.1 Phenothiazines Prochlorperazine and chlorpromazine are the phenothiazines used most frequently for nausea and vomiting of various causes. They act at the CTZ to block dopamine receptors. Prochlorperazine has good absorption after parenteral and oral administration, with a serum half-life of 7 hours. Side effects include hypotension, autonomic responses, hypersensitivity reactions (e.g. cholestatic jaundice) and hormonal dysfunction. Antidopaminergic effects include dystonia, dyskinesia and tardive dyskinesia. 4.1.1.1 Prochlorperazine (Compazine®) Indications are moderate to severe nausea and vomiting. Contraindications include concomitant use of CNS depressants including alcohol. Extrapyramidal side effects including tardive dyskinesia are related to duration and total cumulative dose of neuroleptics. Neuroleptic malignant syndrome (hyperpyrexia, muscle rigidity, altered mental status, autonomic instability including tachycardia, labile blood pressure and cardiac arrhythmias) can occur. Safety for use in pregnancy has not been unequivocally established, although based on limited information, the drug appears relatively safe. A randomized, double-blind comparison of treatment of uncomplicated nausea and vomiting due to viral gastroenteritis with prochlorperazine (Compazine) or promethazine (Phernergan) was published. The results showed that prochlorperazine was significantly better in terms of symptom relief compared to promethazine (119). Time to complete symptom relief was significantly shorter with prochlorperazine than with promethazine. Prochlorperazine also caused significantly fewer complaints of drowsiness. 4.1.1.2 Promethazine (Phenergan®) This is a phenothiazine derivative which also has anti-H1 histamine receptor effects. Indications are the prevention and control of nausea and vomiting associated with anesthesia and surgery, and active and prophylactic treatment of motion sickness. Side effects include drowsiness, and seizure threshold may be lowered. Use with alcohol and other CNS depressants effects should be avoided. 4.1.1.3. Chlorpromazine (Thorazine®) Indications are nausea and vomiting. As for other phenothiazines, side effects include extrapyramidal reactions and the neuroleptic malignant syndrome. Safety is not established in pregnancy. 4.1.1.4. Thiethylperazine maleate (Torecan®) Indications are nausea and vomiting. Contraindications are CNS depression and comatose states. IV administration is contraindicated due to hypotension. Extrapyramidal side effects can be seen. 4.1.1.5 Perphenazine (Trilafon®) Indications are severe nausea and vomiting. Contraindications are obtunded patients, those receiving large doses of CNS depressants, and when blood dyscrasias, bone marrow suppression or liver damage is present. Tardive dyskinesia and neuroleptic malignant syndrome may occur. 4.1.2 Antihistamines These agents work predominantly at the level of the vestibular afferents and within the brain stem. Their use in antiemesis is limited mainly to motion sickness and postoperative emesis. The drugs most commonly used are cyclizine, diphenhydramine and promethazine. 4.1.2.1 Meclizine (Antivert ®) (Bonine ®). Indications are nausea, vomiting and dizziness associated with motion sickness. It may also be used to treat vertigo associated with diseases affecting the vestibular system. The major side effect is drowsiness. Use with alcohol is to be avoided. Due to its potential anticholinergic actions, it should be used with caution in asthma, glaucoma and prostate gland enlargement. Meclizine appears to be relatively safe for use in pregnancy. 4.1.2.2 Diphenhydramine (Benadryl ®). Indication is primarily for treatment of motion sickness. Side effects include sedation. It should be used with caution with narrow-angle glaucoma, stenosing peptic ulcer, pyloroduodenal obstruction and symptomatic prostatic hypertrophy. Additive effects with alcohol and other CNS depressants occurs. 4.1.3 Prokinetic agents These agents influence GI motility through one or more of the following pathways: 1. Directly or indirectly promoting cholinergic tone; 2. Antagonizing inhibitory neurotransmitters (e.g. serotonin, dopamine); or 3. Mimicking noncholinergic nonadrenergic compounds that increase motility (e.g. motilin). Prokinetic agents have been used in the treatment of gastroparesis. Metoclopramide, domperidone and cisapride are effective both in eliminating the symptoms of gastroparesis and in enhancing the rate of gastric emptying (107). 4.1.3.1 Cholinergic agents Direct cholinergic agents include bethanechol, which is the most commonly prescribed agonist, and acts by enhancing the amplitude of contractions throughout the GI tract, including the lower esophageal sphincter. These agents also stimulate the secretion of saliva and gastric acid. Side effects develop due to enhanced parasympathetic tone, including abdominal cramps, diarrhea, salivation, flushing, bradycardia and blurred vision. 4.1.3.2 Substituted Benzamides This class of drugs promotes GI tract motility and increases antroduodenal coordination by indirectly stimulating cholinergic nerves. They cause the release of acetylcholine from enteric neurons. Side effects include a usually transient increase in stool frequency. Drugs that belong to this class include metoclopramide, cisapride and trimethobenzamide. As metoclopramide exhibits significant anti-dopaminergic effects, it is discussed in the following section. Cisapride (Propulsid®) was used as a prokinetic for conditions in which delayed gastric emptying may be etiologic. Antro-duodenal motility is enhanced by this agent. In contrast to metoclopramide, cisapride exhibits no anti-dopaminergic activity. It is also used for gastroesophageal reflux disease. Cardiac arrhythmias such as ventricular tachycardia, ventricular fibrillation, torsade de pointes and QT prolongation may occur when cisapride is used concurrently with ketoconazole, itraconazole, miconazole, fluconazole, erythromycin, troleandomycin and clarithromycin. Due to these adverse effects, cisapride was withdrawn from the market, and is only available from the manufacturer under a compassionate use protocol. Trimethobenzamide (Tigan®) is used to treat nausea and vomiting. Its side effects include drowsiness. Safety in pregnancy is not established, although based on limited information, the drug appears to be relatively safe. 4.1.3.3 Dopamine receptor antagonists Metoclopramide is the prototype drug of this class, and has both peripheral and central dopamine receptor antagonist effects. Peripherally, it enhances release of acetylcholine from intrinsic cholinergic neurons. It is an effective antiemetic in patients receiving chemotherapy. Side effects limit the use of metoclopramide, with an incidence between 10-20%. The most common are due to CNS effects, ranging from mild anxiety, restlessness, depression, nervousness and insomnia, to marked anxiety, confusion, disorientation and hallucinations. Fatigue and extrapyramidal side effects such as tremor, akathisia, tardive dyskinesia and dystonic reactions that mimic Parkinson's disease are due to its central antidopaminergic properties. Gynecomastia due to enhanced prolactin release has been described (107). Based on limited information, metoclopramide appears to be relatively safe for use in pregnancy. Domperidone (Motilium®) is a benzimidazole derivative with anti-dopamine effects in the upper GI tract. A distinguishing feature compared to other substituted benzimidazole agents is the lack of cholinergic activity. Antroduodenal motility and coordination is enhanced specifically by its peripheral antidopaminergic effects. Because domperidone does not cross the blood-brain barrier, no significant central nervous system anti-dopaminergic effects are seen. Central nervous system side effects as seen with metoclopramide are rare. Female patients may develop galactorrhea due to increased prolactin levels. Domperidone was effective in improving delayed gastric emptying in 17 patients with documented gastroparesis. Furthermore, quality of life was enhanced in more than 80% of these patients. Symptoms such as nausea and vomiting, abdominal pain and bloating were improved significantly in this group of patients (109). A direct comparison of metoclopramide and domperidone in a randomized, double-blind study has been reported. Ninety-five patients with nausea and vomiting due to a variety of gastrointestinal causes were given either metoclopramide (15 mg bid) or domperidone (10 mg or 20 mg tid). While both metoclopramide and low and high dose domperidone reduced nausea and vomiting compared to baseline, there were no significant differences noted between the three treatment groups (110). 4.1.3.4 Motilin agonists Erythromycin acts as a prokinetic agent by binding to receptors for the hormone motilin, which regulates the gastric migrating motor complex. As such, it can be used for delayed gastric emptying. Tachyphylaxis can be a problem, making long-term use of this drug difficult. 4.1.4 Anticholinergics The most commonly used agent is hyoscine hydrobromide (scopolamine hydrobromide). It is one of the best agents for motion sickness, and is useful in postoperative nausea and vomiting. In the palliative care setting, it is used for the management of intractable retching and for the control of nausea, emesis and pain produced by intestinal obstruction. 4.1.4.1 Scopolamine (Transderm Scop®) Indications are nausea and vomiting associated with motion sickness. The patch should be applied to the skin behind the ear. Programmed delivery of 0.5 mg of scopolamine over 3 days is provided. It should be used with caution in elderly patients, and in patients with pyloric obstruction or urinary bladder neck obstruction, or those with intestinal obstruction. It can be used in pregnancy if the anticipated benefit justifies the potential risk to the fetus. Adverse reactions include dry mouth, drowsiness, blurred vision and transient dilation of pupils. 4.1.5 5-HT3 receptor antagonists 5-HT3 receptors are located both centrally and peripherally, with high concentrations in the GI tract. Antagonists for this receptor have been evaluated and found to be effective for a variety of conditions, including cancer chemotherapy-induced emesis, emesis due to total body irradiation (111), GI motility disturbances, carcinoid syndrome and nausea and vomiting related to migraine and anxiety (3). 4.1.5.1 Ondansetron Ondansetron is the prototype drug of this class. It is effective in the control of chemotherapy-induced emesis. The principal site of action is in the area postrema, with some gastric prokinetic activity. Ondansetron is not effective against motion sickness. Given orally, ondansetron can be dosed q8-12 hours. Ondansetron is superior to high-dose metoclopramide in chemotherapy-induced emesis. Side effects are few, and include constipation, headache and a transient rise in transaminases. 4.1.5.2 Other 5-HT3 receptor antagonists Additional 5-HT3 receptor antagonists which have been tested clinically are granisetron and tropisetron. Comparative studies have shown similar efficacy for these two agents (112). Direct costs of the drugs in this class did vary widely (129). Efficacy is more pronounced for cisplatin-containing regimens than for less emetogenic regimens. Effectiveness is greater for acute emesis than for delayed emesis. Nausea is more difficult to control than emesis by these agents. Granisetron (Kytril ®) is indicated for the prevention of nausea and vomiting associated with initial and repeat courses of emetogenic cancer therapy, including high-dose cisplatin. 4.1.6 Miscellaneous agents 4.1.6.1 Corticosteroids These agents can assist in relief of cytotoxic drug-induced emesis, especially when combined with other antiemetics. Dexamethasone alone or in combination with ondansetron were shown to be equally efficacious in preventing delayed chemotherapy-induced nausea and vomiting in patients at low risk for this (131). A meta-analysis of the available randomized evidence of the effectiveness of dexamethasone in the treatment of chemotherapy-induced nausea and vomiting was published. Thirty-two studies met the inclusion critieria. Dexamethasone was superior to placebo or no treatment for complete protection of acute emesis (odds ratio 2.22; 95% confidence interval [Cl], 1.89 to 2.60). Also, dexamethasone was superior to placebo or no treatment for complete protection from delayed emesis (odds ratio 2.04; 95% Cl; 1.63-2.56) (132). In adrenal insufficiency, treatment of the underlying cortisol deficiency with corticosteroids will ameliorate the symptoms of this disorder, including nausea and vomiting. 4.1.6.2 Megestrol Acetate This is a progesterone used in the treatment of advanced breast cancer, which has appetite-stimulating properties and can improve the symptoms of nausea from a variety of causes in cancer patients. 4.1.6.3 Tetrahydrocannabinol (dronabinol) and Nabilone The role of delta-9-tetrahydrocannabinol, the active component of marijuana, and nabilone, a synthetic cannabinoid, is mainly in cytotoxic drug-induced emesis (113). Side effects tend to limit their usefulness. Alterations in mood, motor coordination, cognitive function and memory are common. Nabilone has been used successfully for the management of intractable nausea and vomiting in terminally staged AIDS patients (114). Dronabinol (Marinol®) is an orally active cannabinoid. It is used for prophylaxis of chemotherapy-induced emesis. Combination treatment with prochlorperazine may result in synergistic or additive antiemetic effects and attenuate the toxicities. A potential for abuse exists. 4.1.6.4 Benzodiazepines The anxiolytic and amnesic properties of some benzodiazepines can be beneficial for patients whose nausea and vomiting have a psychological component. This is particularly so for the conditioned emesis of cytotoxic chemotherapy. 4.1.6.5 Bismuth subsalicylate (Pepto-Bismol®) Although usually used for the symptomatic control of diarrhea, associated upper GI complaints such as nausea may be relieved. 4.1.6.6 Tricyclic Antidepressants The tricyclic antidepressant class of drugs (amitriptyline, nortriptyline, doxepin, desipramine, and imipramine) have been used at low doses (average does 50 mg/day for the treatment of fuctional nausea and vomiting (117) and cyclic vomiting syndrome (118), with some efficacy. 4.1.6.7 Ginger (Zingiber officinale) Ginger has been advocated as a treatment for nausea and vomiting. A systematic review, however, of the evidence from six randomized clinical trials did not show a significant difference from placebo. However, individual noncontrolled studies have favored ginger over placebo for the treatment of nausea and vomiting caused by seasickness, early pregnancy and chemotherapy (120). 4.1.6.8 Neurkinin-1 antagonists The tachykinin substance P is localized within both the gastrointestinal vagal afferent nerve fibers and in the neural pathways involved in the emetic response in the brainstem. Therefore, substance P is thought to be a key mediator of nausea and vomiting, and antagonists to its receptor, nuerokinin-1 (NK-1), are now being tested for their anti-emetic properties. Preliminary studies in humans show that NK1 receptor antagonists are effective in controlling both chemotherapy-induced and postoperative nausea and vomiting (133). In a randomized, double-blind comparison with ondansetron in the prevention of postoperative nausea and vomiting, the NK1 receptor antagonist CP-122,721 200 decreased emetic episodes more effectively than ondansetron (134).
![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)

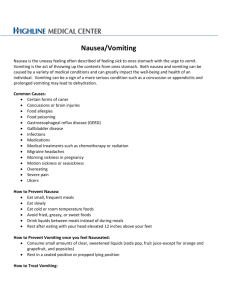
![Questionnaire used in the study Demographics GENDER: M [ ] F](http://s3.studylib.net/store/data/006712173_1-21c851410b04058d524e1b79e54e32b0-300x300.png)