Supplement
advertisement

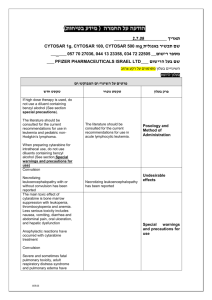
Whitman, et al. -1- Supplement The following CALGB/Alliance institutions participated in this study and contributed at least 1% of patents. For each of these institutions current principal investigators are listed. Wake Forest University School of Medicine, Winston-Salem, NC: David D. Hurd; The Ohio State University Medical Center, Columbus, OH: Clara D. Bloomfield (grant no. U10CA077658); University of Iowa Hospitals, Iowa City, IA: Daniel A. Vaena; North Shore University Hospital, Manhasset, NY: Daniel R. Budman (grant no. U10CA035279); Roswell Park Cancer Institute, Buffalo, NY: Ellis G. Levine (grant no. U10CA059518); Duke University Medical Center, Durham, NC: Jeffrey Crawford (grant no. U10CA047577); University of Chicago Medical Center, Chicago, IL: Hedy L. Kindler (grant no. U10CA041287); Washington University School of Medicine, St. Louis, MO: Nancy L. Bartlett (grant no. U10CA077440); University of Tennessee Cancer Center, Memphis: Harvey B. Niell; Ft. Wayne Medical Oncology/Hematology, Ft. Wayne, IN: Sreenivasa Nattam; University of Massachusetts Medical Center, Worcester, MA: William V. Walsh; Dana Farber Cancer Institute, Boston, MA: Harold J. Burstein (grant no. U10CA032291); Eastern Maine Medical Center, Bangor, ME: Thomas H. Openshaw; Vermont Cancer Center, Burlington, VT: Steven M. Grunberg; University of North Carolina, Chapel Hill, NC: Thomas C. Shea (grant no. U10CA047559); Dartmouth Medical School, Lebanon, NH: Konstantin Dragnev; Weill Medical College of Cornell University, New York, NY: John Leonard; SUNY Upstate Medical University, Syracuse, NY: Stephen L. Graziano; University of Maryland Cancer Center, Baltimore, MD: Martin J. Edelman; Western Pennsylvania Hospital, Pittsburgh, PA: John Lister; Mount Sinai School of Medicine, New York, NY: Lewis R. Silverman; Rhode Island Hospital, Providence, RI: William Sikov; Moores University of California San Diego Cancer Center, San Diego, CA: Barbara A. Parker; Christiana Care Health Services, Inc., Newark, DE: Stephen S. Grubbs. Whitman, et al. -2- Treatment Patients with cytogenetically normal acute myeloid leukemia (CN-AML) younger than 60 years were treated on Cancer and Leukemia Group B (CALGB) trial 19808. Older patients (60 years) were treated on CALGB protocols 8525, 8923, 9420, 9720 and 10201. Patients enrolled on CALGB 19808 (n=71) were randomly assigned to receive induction chemotherapy with cytarabine, daunorubicin, and etoposide with or without PSC-833 (valspodar), a multidrug resistance protein inhibitor.1 On achievement of complete remission (CR), patients were assigned to intensification with high-dose cytarabine and etoposide for stem-cell mobilization followed by myeloablative treatment with busulfan and etoposide supported by autologous peripheral blood stem-cell transplantation. Older patients (≥60 years) were all treated with cytarabine/daunorubicin-based induction therapy followed by cytarabine-based consolidation therapy. Patients on CALGB 8525 (n=18) were treated with induction chemotherapy consisting of cytarabine in combination with daunorubicin and were randomly assigned to consolidation with different doses of cytarabine followed by maintenance treatment.2 Patients on CALGB 8923 (n=15) were treated with induction chemotherapy consisting of cytarabine in combination with daunorubicin and were randomly assigned to receive postremission therapy with cytarabine alone or in combination with mitoxantrone.3 Patients on CALGB 9420 (n=5) and 9720 (n=96) received induction chemotherapy consisting of cytarabine in combination with daunorubicin and etoposide, with (CALGB 9420) or with/without (CALGB 9720) the multidrug resistance protein modulator PSC-833.4,5 Patients on CALGB 9420 received postremission therapy with cytarabine (2 g/m2/d) alone, and patients on CALGB 9720 received a single cytarabine/daunorubicin consolidation course and were then randomly assigned to low-dose recombinant interleukin-2 maintenance therapy or none.6 Patients on CALGB 10201 (n=65) received induction chemotherapy consisting of cytarabine and daunorubicin, with or without the BCL2 antisense oblimersen sodium. The consolidation regimen included two cycles of cytarabine (2 g/m 2/d) with or without oblimersen.7 Whitman, et al. -3- Definition of clinical endpoints Clinical endpoints were defined as follows8: CR required a bone marrow aspirate with cellularity greater than 20% and maturation of all cell lines, less than 5% blasts and no Auer rods; in the peripheral blood, an absolute neutrophil count of ≥1,500/µL, platelet count of >100,000/µL, and no leukemic blasts; and no evidence of extramedullary leukemia, all of which had to persist for at least 1 month.8 Relapse was defined by the presence of ≥5% bone marrow blasts, or circulating leukemic blasts, or the development of extramedullary leukemia. Disease-free survival (DFS) was measured from the date of CR until the date of relapse or death; patients alive and in CR were censored at last follow-up. Overall survival (OS) was measured from the date of study entry until the date of death, and patients alive at last follow-up were censored. Statistical Analyses The “optimal” cutpoint is defined as the value of the continuous MERTK variable that best separates low and high risk patients with respect to DFS and OS using the log rank test.9 All clinical endpoint analyses were age group-adjusted (ie, <60 years vs ≥60 years) when we considered all patients since there were treatment regimen or intensity differences in the treatment protocols for these two age groups. Multivariable age group-adjusted logistic regression models were generated for attainment of CR, and multivariable age group-adjusted proportional hazards models were constructed for DFS and OS using a limited backwards elimination procedure.9 Variables considered for model inclusion and evaluated in univariable models were: GAS6 expression status, TYRO3/AXL dual receptor status, MERTK expression, European LeukemiaNet (ELN) genetic category (based on the presence/absence of FLT3-ITD, and NPM1 and CEBPA mutations), GAS6 mutation-by-TYRO3/AXL dual receptor status Whitman, et al. -4- interaction, mutation status of the TET2, WT1, IDH1, IDH2, RUNX1, ASXL1, and DNMT3A genes, FLT3-tyrosine kinase domain mutation status, MLL partial tandem duplication (MLL PTD) status, age group (≥60 years vs <60 years, retained in all models), sex, race (white vs nonwhite), white blood cell (WBC) count, hemoglobin and platelet counts. RUNX1 was not considered for CR and DFS due to small sample sizes. Variables significant at α=.20 from the univariable analyses were considered for multivariable analyses. For the time-to-event endpoints, the proportional hazards assumption was checked for each variable individually. The specific variables included in outcome modeling are: CR: GAS6 (+ vs –), ELN (Favorable vs Intermediate-I), WT1 (mutated vs wild-type), ASXL1 (mutated vs wild-type), ERG (high vs low), BAALC (high vs low), platelet counts (50x109/L increase), WBC count (50x109/L increase), extramedullary involvement (present vs absent), age group (≥60 years vs <60 years); DFS: GAS6 (+ vs –), TYRO3/AXL dual receptor status (+ vs –), ELN (Favorable vs Intermediate-I), WT1 (mutated vs wild-type), MLL-PTD (present vs absent), DNMT3A (R882 mutated vs nonR882 mutated and wild-type), ERG (high vs low), BAALC (high vs low), age group (≥60 years vs <60 years); OS: GAS6 (+ vs –), TYRO3/AXL dual receptor status (+ vs –), ELN (Favorable vs Intermediate-I), WT1 (mutated vs wild-type), MLL-PTD (present vs absent), RUNX1 (mutated vs wild-type), DNMT3A (R882 mutated vs non-R882 mutated and wild-type), ERG (high vs low), BAALC (high vs low), WBC count (50x109/L increase), age group (≥60 years vs <60 years). Age group was retained regardless of statistical significance. Whitman, et al. -5- REFERENCES 1. Kolitz JE, George SL, Marcucci G, Vij R, Powell BL, Allen SL et al. P-glycoprotein inhibition using valspodar (PSC-833) does not improve outcomes for patients under age 60 years with newly diagnosed acute myeloid leukemia: Cancer and Leukemia Group B study 19808. Blood 2010; 116: 1413-1421. 2. Mayer RJ, Davis RB, Schiffer CA, Berg DT, Powell BL, Schulman P et al. Intensive postremission chemotherapy in adults with acute myeloid leukemia. N Engl J Med 1994; 331: 896-903. 3. Stone RM, Berg DT, George SL, Dodge RK, Paciucci PA, Schulman P et al. Granulocyte-macrophage colony-stimulating factor after initial chemotherapy for elderly patients with primary acute myelogenous leukemia. N Engl J Med 1995; 332: 1671-1677. 4. Lee EJ, George SL, Caligiuri M, Szatrowski TP, Powell BL, Lemke S et al. Parallel phase I studies of daunorubicin given with cytarabine and etoposide with or without the multidrug resistance modulator PSC-833 in previously untreated patients 60 years of age or older with acute myeloid leukemia: results of cancer and leukemia group B study 9420. J Clin Oncol 1999; 17: 2831-2839. 5. Baer MR, George SL, Caligiuri MA, Sanford BL, Bothun SM, Mrózek K et al. Low-dose interleukin-2 immunotherapy does not improve outcome of patients age 60 years and older with acute myeloid leukemia in first complete remission: Cancer and Leukemia Group B study 9720. J Clin Oncol 2008; 26: 4934-4939. 6. Baer MR, George SL, Sanford BL, Mrózek K, Kolitz JE, Moore JO et al. Escalation of daunorubicin and addition of etoposide in the ADE regimen in acute myeloid leukemia patients aged 60 years and older: Cancer and Leukemia Group B study 9720. Leukemia 2011; 25: 800-807. Whitman, et al. 7. -6- Marcucci G, Moser B, Blum W, Stock W, Wetzler M, Kolitz JE et al. A phase III randomized trial of intensive induction and consolidation chemotherapy ± oblimersen, a proapoptotic Bcl-2 antisense oligonucleotide in untreated acute myeloid leukemia patients >60 years old [abstract]. J Clin Oncol 2007; 25(suppl): 360s (abstract #7012). 8. Cheson BD, Cassileth PA, Head DR, Schiffer CA, Bennett JM, Bloomfield CD et al. Report of the National Cancer Institute-sponsored workshop on definitions of diagnosis and response in acute myeloid leukemia. J Clin Oncol 1990; 8: 813-819. 9. Klein JP, Moeschberger ML. Survival Analysis: Techniques for Censored and Truncated Data. New York, NY: Springer; 2003. Whitman, et al. -7- Table S1. Clinical outcomes according to TYRO3/AXL/MERTK receptor tyrosine kinases expression status in de novo cytogenetically normal AML patients Variable CR DFS OS OR (95% CI) P HR (95% CI) P HR (95% CI) P TYRO3+ vs TYRO3– 1.30 (0.69-2.44) 0.41 1.72 (1.18-2.50) 0.005 1.56 (1.14-2.13) 0.005 AXL+ vs AXL– 0.75 (0.30-1.84) 0.52 1.04 (0.66-1.65) 0.86 0.82 (0.54-1.25) 0.36 MERTK+ vs MERTK– 1.09 (0.61-1.92) 0.78 0.88 (0.63-1.22) 0.44 0.89 (0.68-1.17) 0.41 Abbreviations: CR, complete remission, DFS, disease-free survival, OS, overall survival; OR, odds ratio; CI, confidence interval; HR, hazard ratio. All clinical endpoints are age group adjusted. An odds ratio greater than (less than) 1.0 means a higher (lower) CR rate for patients in the first group compared to patients in the second group. A hazard ratio greater than 1 (less than 1) corresponds to a higher (lower) risk of an event for patients in the first group compared to patients in the second group. The median follow-up for those patients alive is 7.2 years, range: 2.3-11.6 years Whitman, et al. -8- Table S2. Genes differentially expressed between GAS6+ and GAS6- CN-AML patients (see separate Excel file)