Biology 102 Chapter 42
Biology 102 Chapter 42
Animal Reproduction
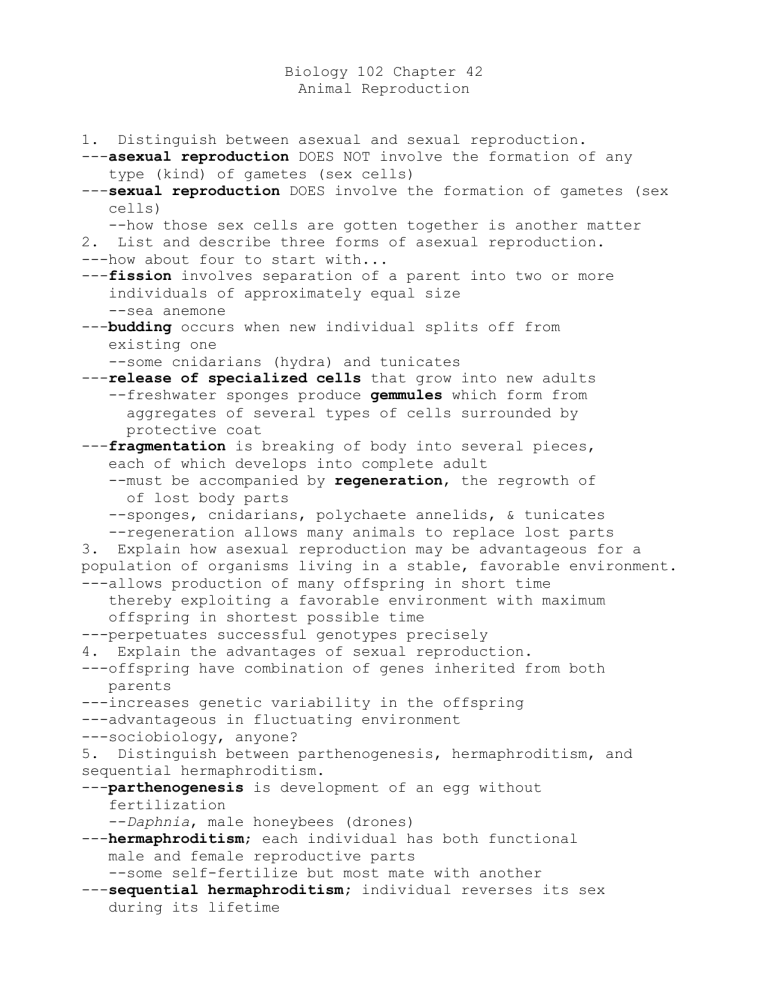
1. Distinguish between asexual and sexual reproduction.
--asexual reproduction DOES NOT involve the formation of any
type (kind) of gametes (sex cells)
--sexual reproduction DOES involve the formation of gametes (sex
cells)
--how those sex cells are gotten together is another matter
2. List and describe three forms of asexual reproduction.
---how about four to start with...
--fission involves separation of a parent into two or more
individuals of approximately equal size
--sea anemone
--budding occurs when new individual splits off from
existing one
--some cnidarians (hydra) and tunicates
--release of specialized cells that grow into new adults
--freshwater sponges produce gemmules which form from aggregates of several types of cells surrounded by protective coat
--fragmentation is breaking of body into several pieces,
each of which develops into complete adult
--must be accompanied by regeneration , the regrowth of
of lost body parts
--sponges, cnidarians, polychaete annelids, & tunicates
--regeneration allows many animals to replace lost parts
3. Explain how asexual reproduction may be advantageous for a population of organisms living in a stable, favorable environment.
---allows production of many offspring in short time
thereby exploiting a favorable environment with maximum
offspring in shortest possible time
---perpetuates successful genotypes precisely
4. Explain the advantages of sexual reproduction.
---offspring have combination of genes inherited from both
parents
---increases genetic variability in the offspring
---advantageous in fluctuating environment
---sociobiology, anyone?
5. Distinguish between parthenogenesis, hermaphroditism, and sequential hermaphroditism.
--parthenogenesis is development of an egg without
fertilization
-Daphnia , male honeybees (drones)
--hermaphroditism ; each individual has both functional
male and female reproductive parts
--some self-fertilize but most mate with another
--sequential hermaphroditism; individual reverses its sex
during its lifetime
--some species are protogynous (female first)
--some are protandrous (male first)
--reversal often associated with age and size
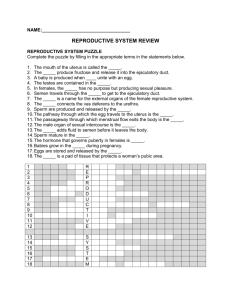
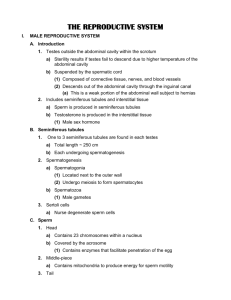
6. Using a diagram, identify and give the function of each component of the reproductive system of the human male.
---external genitalia includes scrotum and penis
(copulatory organ)
---internal reproductive organs consist of gonads ( testes ), accessory glands , and associated ducts
---testes comprised of highly coiled tubules ( seminiferous tubules ) surrounded by layers of connective tissue
--interstitial cells ( Leydig cells ) scattered among tubules and produce testosterone/other androgens
--sperm pass from seminiferous tubules into tubules of
e pididymis
--sperm are stored and mature (gain motility/fertilizing power)
---at ejaculation , sperm forced through vas deferens (a
muscular duct connecting epididymis to ejaculatory duct
---ejaculatory duct forms by joining of the two
vas deferens ducts with duct from seminal vesicles
---ejaculatory duct opens into the urethra (tube that runs
through penis and drains both excretory/reproductive
systems
---are 3 sets of accessory glands associated with male
system
--add their secretions to semen
--pair of seminal vesicles located below and behind
urinary bladder and empty into ejaculatory duct
--secrete fluid containing mucus, amino acids
(for coagulation), fructose, and prostaglandins
--comprises about 60% of total semen volume
--prostate gland is large gland surrounding upper portion
and emptying directly into urethra
--secretes thin, milky alkaline fluid with enzymes
--balances acidity of residual urine in system
--buffers acidity of vagina/activates sperm
--bulbourethral glands are pair of small glands below
prostate that empty into urethra at base of penis
--secrete clear mucus before ejaculation
--neutralize remaining acidic urine in urethra
---head of penis ( glans penis ) covered with foreskin called prepuce
--some male mammals possess a baculum (penis bone)
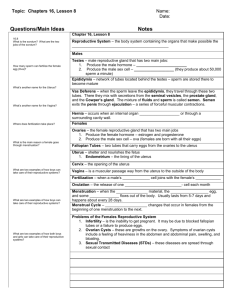
7. Using a diagram, identify and give the function of each component of the human female reproductive system.
---internal reproductive organs are gonads (ovaries) and
associated ducts and chambers
--involved with gamete movement/embryo development
---external genitalia include clitoris/2 sets of labia
--ovaries located in abdominal cavity/enclosed in tough
protective capsule
--mesentery flanks & attaches each ovary to uterus
--each ovary contains follicles (1 egg cell surrounded
by follicle cells which nourish and protect egg cell)
--follicle cells also produce estrogens
---during ovulation , egg expelled from follicle
--remaining tissue forms corpus luteum (secretes progesterone (maintains uterine lining) and additional
estrogen
--egg cell expelled into abdominal cavity near opening of oviduct
-cilia lining oviduct draw egg cell in --> uterus
---uterus (womb) is thick muscular organ that can expand to
accommodate a 4-kg fetus
--inner uterine lining ( endometrium ) is richly supplied with blood vessels
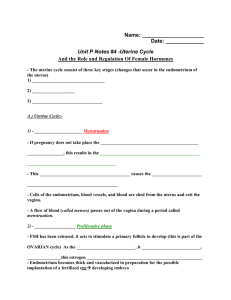
REMAINING FEMALE REPRODUCTIVE STRUCTURES
--cervix; neck of uterus which opens into vagina
--vagina; thin-walled chamber, repository for semen during
copulation, also forms birth canal
--hymen ; vascularized membrane, usually covers vaginal
opening from birth until ruptured by vigorous physical
activity or sexual intercourse
--vestibule ; chamberlike area formed by 2 pairs of skin
folds covering the vaginal orifice/urethral opening
---libia minora ; slender skin folds bordering vestibule
--libia majora; pair of thick, fatty ridges enclosing and
protecting libia minora & vestibule
--clitoris ; bulb of erectile tissue at front edge of
vestibule which is covered by a prepuce (small hood)
--Bartholin’s glands; small glands located near vaginal
opening that secrete mucus into vestibule during
sexual arousal, facilitates intercourse by lubricating
vagina
---mammary glands ; important to reproduction but not part
of reproductive system
8. Discuss the hormonal control of reproduction in male mammals.
--androgens directly responsible for formation of primary
sex characteristics (reproductive organs)& secondary sex
characteristics (deepening of voice, hair growth
patterns, muscle growth)
--steroid hormones produced primarily by Leydig cells of testes
--testosterone most important androgen
---androgens are potent determinants of sexual/aggressive
behaviors
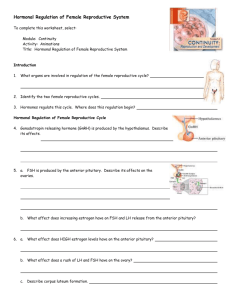
---GnRH from hypothalamus stimulates anterior pituitary to
release LH (stimulates androgen production) and FSH
(acts on seminiferous tubules to > sperm production)
9. Explain the differences between menstrual and estrous cycles.
--menstrual cycle characterized by endometrium break down,
sloughing off of lining, and discharge from the body via the
vagina if fertilization has NOT occurred
--from “menses” which is Latin for “months”
--uterine cycles of mammals other than humans does NOT include menstruation
--uterine lining is reabsorbed into body
--ovarian cycle characterized by state of sexual receptivity
called estrus (correlated with ovulation)
--“heat” or “season”
--female solicits male attention and may be aggressive to other females
---time for some sociobiology
10. Discuss the hormonal control of reproduction in female mammals.
---hormones coordinate menstrual and ovarian cycles
--ovulation synchronized with uterine preparation for possible implantation of embryo
---5 hormones participate in elaborate positive and
negative feedback scheme
--gonadotropin-releasing hormone (GnRH) from hypothalamus
--follicle-stimulating hormone (FSH) and luteinizing
hormone (LH) from anterior pituitary
--estrogens (family of closely related hormones) and progesterone; the female sex hormones secreted by
ovaries
---SEE OVERHEAD TRANSPARENCY
11. Explain how the menstrual cycle and ovarian cycle are synchronized in female mammals.
---cycles coordinated and timed by same hormones that initiate
sexual maturation
---in response to FSH and LH, ovarian tissue grows and produces
estrogen
--estrogen causes development of secondary sexual characteristics
---menstruation marks beginning of uterine/ovarian cycles
---few days before menstruation begins, anterior pituitary >
secretion of FSH and LH
--some follicles begin to mature in ovaries
--generally only one follicle continues the process
---developing follicle secretes > amounts of estrogen which
causes endometrium to grow
---estrogen exerts negative feedback control on gonadotropin
release by anterior pituitary (FSH and LH) during first 12
days of cycle
---on day 12, estrogen exerts POSITIVE feedback on pituitary and
there is surge of LH and slight surge of FSH
--LH triggers mature follicle to rupture, releasing its egg
--also stimulates follicle to become corpus luteum which secretes estrogen and progesterone
---estrogen and progesterone CRITICAL to continued growth and
maintenance of endometrium
---these sex steroids exert – feedback on pituitary inhibiting
gonadotropin release thereby preventing new follicles from
beginning to mature
---egg not fertilized, corpus luteum degenerates on about day 26
of cycle
---without progesterone by corpus luteum, endometrium sloughs off
and menstruation occurs
---decrease in circulating steroids allows hypothalamus/anterior
pituitary to increase GnRH, FSH, and LH and next cycle begins
12. Describe spermatogenesis.
--spermatogonia are the diploid cells that are precursors
of sperm
--located near outer wall of seminiferous tubules, spermatogonia undergo repeated mitoses which produce large populations of potential sperm
---in mature male, about 3 million spermatogonia per day
differentiate into primary spermatocytes
---primary spermatocytes undergo meiosis I to produce
two secondary spermatocytes which are now HAPLOID but
still have duplicated chromosomes
---secondary spermatocytes undergo meiosis II
--separates the sister chromatids
--produces 4 spermatids
---spermatids mature into mature spermatozoa (sperm cells)
--involves association with Sertoli cells which transfer nutrients to spermatids
---during spermatogenesis, developing sperm gradually
pushed toward center of seminiferous tubule
--make their way to epididymis where they acquire motility
---from spermatogonia to motile sperm = 65 to 75 days
13. Describe oogenesis.
--oogenesis is the development of ova (mature,
unfertilized egg cells)
---begins in embryo when primordial germ cells undergo
mitotic divisions to produce diploid oogonia
---each oogonium develops into primary oocyte by time
of birth
--all potential ova present in ovaries at birth
--primary oocytes (diploid) proceed to Prophase I
between 3 rd and 7 th month of fetal development
--then enter state of suspended development until puberty
---after puberty, during each ovarian cycle, FSH stimulates
a follicle to enlarge & primary oocyte within completes
meiosis I to produce haploid secondary oocyte and first
polar body
---meiosis STOPS again
---LH triggers ovulation and secondary oocyte released from
follicle
---if fertilization occurs, meiosis II will occur and
second polar body will separate from ovum
14. Compare and contrast oogenesis and spermatogenesis.
---in spermatogenesis, all 4 products of meiosis I and II
become mature spermatozoa
---in oogenesis, only one daughter cell will become single
ovum, the other cells (polar bodies) will degenerate
---spermatogenesis is a continual process throughout
reproductive life of a male
---all potential ova that can be produced by oogenesis are
present as primary oocytes in ovaries at time of
female’s birth
---spermatogenesis occurs as uninterrupted sequence
---oogenesis has long resting periods between formation
of initial steps and final production of ovum
15. Describe the changes that occur in the developing embryo and the mother during each trimester of a human pregnancy.
---human gestation divided into 3 trimesters (about 3
months each)
--FIRST TRIMESTER is when most radical changes occur for
both mother and baby
---fertilization occurs in oviduct & cleavage (cell
division) begins in about 24 hours
---zygote develops into ball of cells
---embryo reaches uterus in 3-4 days and develops into
hollow ball of cells called blastocyst (about 1 week
after fertilization
---blastocyst will implant in endometrium in next 5 days
---during implantation , blastocyst bores into endometrium
--endometrium grows over blastocyst
---embryonic tissues begin to mingle with endometrium to
form placenta which functions in respiratory gas
exchange, nutrient transfer, and waste removal from
embryo
---also main period of organogenesis (organ development)
---after 8 weeks, embryo becomes a fetus
--possesses all adult organs in rudimentary form
---fetus is about 5 cm in length by end of 1 st trimester
---embryo secretes hormones that signal its presence and
controls mother’s reproductive system
-human chorionic gonadotropin (HCG) maintains progesterone and estrogen secretion by corpus luteum to prevent menstruation
--high progesterone levels also stimulate formation of protective mucous plug in cervix, growth of maternal part of placenta, uterus enlargement, and cessation of ovulation and menstrual cycling
--SECOND TRIMESTER time of rapid growth and fetal activity
---fetus grows to about 30 cm in length
---mother may feel movement (quickening)
---hormone levels stabilize as HCG declines
--corpus luteum degenerates
--placenta secretes its own progesterone to maintain the pregnancy---uterus grows sufficiently for pregnancy to be obvious
---THIRD TRIMESTER time of rapid growth but decreasing
fetal activity
---fetus grows to about 50 cm in length, and 3 to 3.5 kg in
weight
---maternal abdominal organs become compressed & displaced
---labor is induced & regulated by interplay among
estrogen, oxytocin, and prostaglandins
--high estrogen levels during last weeks of pregnancy trigger formation of oxytocin receptors on uterus
--oxytocin (from fetus/maternal posterior pituitary)
stimulate smooth muscles of uterus to contract
--oxytocin stimulates prostaglandin secretion by placenta (enhance muscle contractions)
--parturition (birth) occurs through series of strong,
rhythmic contractions of uterus (labor)
--3 stages to labor
--1 st stage involves opening and thinning of cervix until completely dilated
--2 nd stage is expulsion of baby from uterus
-contractions strong and continuous
--3 rd stage is expulsion of the placenta from uterus
16. Describe the hormonal control of pregnancy in a human female.
---hormones secreted by embryo necessary to insure
pregnancy continues
---embryo secretes hormones that signal its presence and
control mother’s reproductive system
--human chorionic gonadotropin (HCG) acts like pituitary
LH to maintain secretion of progesterone and estrogens
by corpus luteum through 1 st trimester
---in absence of hormonal override provided by embryo,
decline in maternal LH due to inhibition of pituitary
by progesterone would result in menstruation and
spontaneous abortion of embryo
---EPT (and others) based on HCG hormone
---cervix mucus plug, growth of maternal part of
placenta, enlargement of uterus, cessation of
ovulation and menstruation all result of high
levels of progesterone
17. List the various methods of contraception and explain how they work.
--three major ways to achieve contraception
---(1) prevent fertilization by keeping egg and sperm apart
---(2) prevent implantation of embryo
---(3) prevent release of mature egg and sperm from gonads
--keeping egg and sperm from meeting in the female
reproductive tract prevents fertilization
--abstinence
--rhythm method
--condoms, diaphragms, cervical caps, contraceptive sponges
--coitus interruptus
--tubal ligation and vasectomy
---preventing implantation of blastocyst in uterus can be
accomplished by using intrauterine device (IUD)
--probably works by irritating the endometrium
---chemical contraception prevents release of mature
gametes from gonads
--birth control pills
--minipill