The Effects of Maternal Familial Autoimmunity, Gestational Stress
advertisement
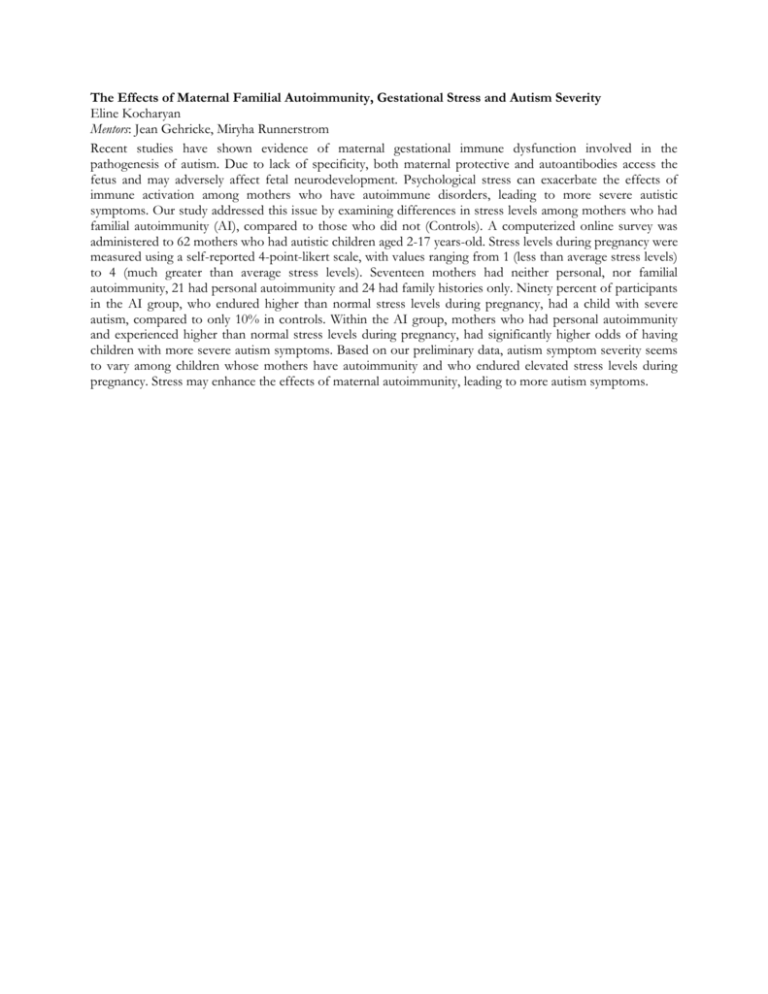
The Effects of Maternal Familial Autoimmunity, Gestational Stress and Autism Severity Eline Kocharyan Mentors: Jean Gehricke, Miryha Runnerstrom Recent studies have shown evidence of maternal gestational immune dysfunction involved in the pathogenesis of autism. Due to lack of specificity, both maternal protective and autoantibodies access the fetus and may adversely affect fetal neurodevelopment. Psychological stress can exacerbate the effects of immune activation among mothers who have autoimmune disorders, leading to more severe autistic symptoms. Our study addressed this issue by examining differences in stress levels among mothers who had familial autoimmunity (AI), compared to those who did not (Controls). A computerized online survey was administered to 62 mothers who had autistic children aged 2-17 years-old. Stress levels during pregnancy were measured using a self-reported 4-point-likert scale, with values ranging from 1 (less than average stress levels) to 4 (much greater than average stress levels). Seventeen mothers had neither personal, nor familial autoimmunity, 21 had personal autoimmunity and 24 had family histories only. Ninety percent of participants in the AI group, who endured higher than normal stress levels during pregnancy, had a child with severe autism, compared to only 10% in controls. Within the AI group, mothers who had personal autoimmunity and experienced higher than normal stress levels during pregnancy, had significantly higher odds of having children with more severe autism symptoms. Based on our preliminary data, autism symptom severity seems to vary among children whose mothers have autoimmunity and who endured elevated stress levels during pregnancy. Stress may enhance the effects of maternal autoimmunity, leading to more autism symptoms.