RAD 264 – Computed Tomography Physics, Instrumentation, and
advertisement

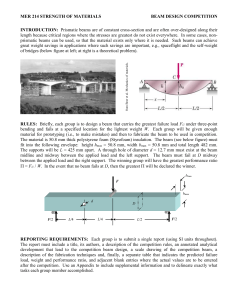
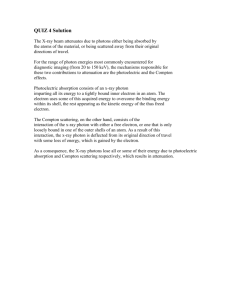
Computed Tomography Physics, Instrumentation, and Imaging Module E Required reading for this module is Chapters 3, and 4 of your text. Seeram, Computed Tomography 2nd edition, Saunders/Elsevier. This module must be prefaced with something that may place the student’s mind at ease. When the physics of CT is discussed, many believe that they are lacking in a basic understanding of these physical principles and therefore must learn something new. That is far from the truth. There really is no “physics of CT.” CT uses ionizing radiation and radiation physics is taught in all radiography programs, so those that have successfully completed these programs have at least a basic understanding of radiation physics and can therefore apply this knowledge to the physical principles surrounding CT. As promised, this module will continue the discussion on attenuation and provide the student with information that allows the logical extension of knowledge learned in the physics of conventional radiography into computed tomography. In conventional radiographic imaging, a uniform x-ray beam is directed at the patient, exiting the opposite side. When the beam exits, it carries with it information about the anatomy through which it traveled. It is encoded with information regarding the variations of the intensity of the beam due to the differential attenuation of the x-rays along their differing paths through the patient. As presented in the preceding module, attenuation is based on the Lambert-Beer Law. It is the reduction in the intensity of a radiographic beam as it travels through matter. It can also be described as the “total reduction in the number of x-rays remaining in an x-ray beam after penetration through a given thickness of tissue.” In conventional radiography the attenuated beam is recorded on a two dimensional surface film-based system; the cassette or image receptor as it is now known. What remains after an x-ray beam is attenuated and strikes the x-ray film emulsion is called remnant radiation. When x-rays penetrate body tissue of any type, they interact with the atoms of the tissue by certain mechanisms as listed below: Coherent (Classical) Scattering Compton Effect Photoelectric Effect Pair Production Triplet Production Photodisintegration Copyright © Southern Union State Community College, 2007. 1 The above mechanisms should have been learned in a previous radiation physics course. Of all of the mechanisms listed, in diagnostic radiology, we are only concerned with two; the Compton and Photoelectric Effects. We know that in conventional radiography, the Compton Effect does not result in any useful diagnostic information reaching the radiograph. It is the x-rays that undergo photoelectric interaction with body tissue that transmit diagnostic information to the cassette (image receptor or IR). Therefore, a radiographic image is primarily the results of the differences between photoelectrically absorbed x-rays and those that were not absorbed at all. This is termed differential absorption and means simply that body tissues absorb radiation differently depending on their thickness or mass densities and the energy of the x-ray photons that travel through them. The Photoelectric effect (absorption) primarily occurs in substances and tissues with high Z numbers, such as bone and contrast media, and to a much lesser degree in some soft tissue and substance having lower Z numbers. In CT, the Compton effect, because it occurs in soft-tissue, and the density differences in soft tissue, result in differences in the Compton interaction. However things re not quite that simple, since the Photoelectric effect also depends on beam energy (kV) and the Compton effect is generally not likely to dominate as the kV increases. In addition, the energy dependence of the Compton effect is not as dramatic as that of the Photoelectric effect, but attenuation can be based on both. As noted in the previous module, attenuation in CT depends on the effective atomic density, in atoms/volume, the Znumber of the absorber (atomic number), and the energy of the x-ray photons. The determination of x-ray attenuation in body tissue and the use of that information to reconstruct images of the anatomy scanned is the basic problem n CT. This is no easy task as it requires the application of physics, complex mathematics, as well as computer science. In initial experiments by Hounsfield involving the invention of the CT scanner, a uniform (homogeneous/monochromatic) pencil beam of radiation from a gamma source was used. This type of beam was used because it fulfills the requirements of the Lambert-Beer Law. Monochromatic beams are composed of photons having the same energy level, while heterogeneous beams are made up of x-ray photons with varying energy levels. As homogeneous beams of radiation pass through body tissue, each section of the absorber (patient anatomy) attenuates the beam equally, resulting in the quantity of the photons being reduced, while the quality or energy of the beam remains the same. The major goal in CT is to calculate the linear attenuation coefficient (μ). By the way, μ is a Greek symbol called mu (pronounced mew), used to denote the linear attenuation coefficient in CT. The symbol can be used to denote almost anything, so if it is used outside of CT it usually does not mean or stand for linear attenuation coefficient. Now back to the discussion at hand. The linear attenuation coefficient denotes how much attenuation has occurred. So, it can be surmised that attenuation “is a quantitative measurement having a unit of per -1 centimeter (cm ) –hence the term linear.” Hounsfield used the equation for the Lambert-Beer Law provided in Module D when conducting early experiments Copyright © Southern Union State Community College, 2007. 2 regarding the determination of the linear attenuation coefficient. For your convenience in recalling the formula, it is: Iin = Iout e -μx In Hounsfield’s early experiments, problems were encountered because of his use of a gamma source and a pencil homogeneous beam of radiation. It took too long to scan an object and to produce an image, so Hounsfield replaced the gamma source with conventional radiographic tube. He also changed the beam geometry to that of a fan-beam. Conventional radiographic tubes produce heterogeneous (polychromatic) beams, meaning these beams are made up of a wide range of energy levels. Obviously, there are differences in the way attenuation occurs when using monochromatic beams versus polychromatic beams of radiation. Because of this, Hounsfield was challenged with having to make several assumptions regarding the use of this type of beam and adjust his invention accordingly. As stated earlier, when monochromatic beams are employed, the quantity of the beam is reduced as the beam travels through body tissue, due to attenuation, but the beam energy or quality remains unchanged. When a polychromatic beam travels through body tissue, the attenuation is not exponential as in the Lambert-Beer Law. In the case of polychromatic beams, as the x-ray photons with various energy levels traverse equal thicknesses of body tissues, both the quantity and the quality of the beam changes. The study of radiation physics and biology tells us that in this case, the lower energy photons will be absorbed, while those with higher energy levels will pass through the object. The following schematic provides a depiction of attenuation through body tissue when a polychromatic beam of radiation in used in CT. Copyright © Southern Union State Community College, 2007. 3 Because of the use of a polychromatic beam in CT, the linear attenuation coefficient must be determined differently than if a monochromatic beam was used. Hounsfield had to find a way for the polychromatic beam used in CT to “approximate a monochromatic beam” in order to satisfy the Lambert-Beer equation. He was challenged with finding a way to incorporate the number of x-ray photons that pass through body tissues during the scanning process, as opposed to the intensity of the bean, in the determination of linear attenuation coefficients. He came up with the following equation: N = Noe -μx N = the number of transmitted x-ray photons No = the number of x-ray photons entering body tissue (incidental photons) μ = equals the linear attenuation coefficients of the tissue (μp +μc) e = the base of the natural logarithm (Euler’s Constant of 2.718) Because the x-ray beam in CT does not travel through a uniform block of tissue, the above equation was modified to: CT is unlike conventional radiographic imaging in that it is a method of acquiring and reconstructing anatomical images cross-section. In addition, because it forms cross-sectional images, it effectively eliminates the superimposition of anatomical structures and it is especially sensitive to subtle variations in x-ray attenuation. In conventional CT (step and shoot), the radiographic tube revolves around the patient emitting x-rays (making exposures). Many measurements are received by the detectors from the plane of a defined slice thickness coming from the patient’s body. The CT system uses this data to reconstruct a digital image of the cross-section (slice); therefore, CT is a digital imaging processing technique. Copyright © Southern Union State Community College, 2007. 4 The digital images are based upon the attenuation of the x-rays through each pixel of the image matrix. The intensity of the transmitted beam is a function of the attenuation coefficient of each pixel through which the beam is transmitted. Thus, the images are produced from topographic maps of the x-ray linear attenuation coefficients. The following is a depiction of a conventional CT image “slice”, as it relates to the CT matrix, pixel, and voxel. Copyright © Southern Union State Community College, 2007. 5 In order for digitization of the CT image to occur, an image matrix size selection is made by the technologists as a part of protocol selection. Normally a 512 x 512 image matrix size is selected, although many of today’s CT scanners allow for the selection of a 1024 x 1024 image matrix also. A matrix is defined as an array of numbers composed of rows and columns. Where the rows and columns intersect, squares called pixels are created. The image matrix in CT is composed at minimum, of thousands of pixels that represent varying shades of gray. In the image above, the matrix size is 7 x 7, meaning that it is composed of seven rows and 7 columns for a total of 49 squares or pixels. The addition or selection of slice-thickness changes the pixels into volume elements or voxels that are representative of the tissue volume irradiated within the slice. In a 512 x 512 image matrix, there are 262, 144 pixels (picture element cells). In a 1024 x 1024 matrix, there are 1, 042,576 pixels. This workforce solution was funded by a grant awarded under the President’s Community-Based Job Training Grants as implemented by the U.S. Department of Labor’s Employment and Training Administration. The solution was created by the grantee and does not necessarily reflect the official position of the U.S. Department of Labor. The Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership. This solution is copyrighted by the institution that created it. Internal use by an organization and/or personal use by an individual for noncommercial purposes is permissible. All other uses require the prior authorization of the copyright owner. 6 Copyright © Southern Union State Community College, 2007. 7 As noted in the above image matrix, there are different tissue types within the matrix overall and within specific pixels. The tissue differences within the pixels are represented by CT numbers or Hounsfield (CT) numbers. The pixel is considered a two-dimensional representation of the corresponding volume element. Pixel size is calculated using the following formula: 2 2 P (mm ) = DFOV (mm )/Matrix Size P = Pixel Size in mm DFOV = Display Field of View Pixels are displayed on the CRT (CT monitor) as shades of gray. The voxel size is determined by multiplying the pixel size by the thickness of the slice. Voxel measurements are made using the formula; 3 2 Voxel Size (mm ) = DFOV (mm ) (slice thickness in mm)/Matrix Size The distribution of the attenuation values of the tissue through which the beam has passed is established using a process called sampling. Sampling can be considered a measurement technique wherein signals coming from the CT detectors are in analog form and must be converted into digital format before being forwarded to the CT computer for image reconstruction. This requires measurement of the brightness of each pixel in the image matrix. The brightness is detected by a photomultiplier tube. Sampling is performed according to the Nyquist Theorem. The theorem states: “Sampling must be performed at least twice the spatial frequency of the object scanned”, meaning at least as often as the occurrence of every peak and valley of the wave defining the frequency of the object. In CT, sampling has two components; angular and ray. Angular sampling is determined by the distance between each view obtained during a CT scan, while ray sampling is determined by the angle between each pair of rays within a view. In order to facilitate an understanding of angular and ray sampling, one must first understand what the terms ray and view mean. Copyright © Southern Union State Community College, 2007. 8 Rays and Views 1. In Third Generation CT scanners, each ray of the fan-beam strikes a single detector. 2. Each set of rays constitutes a view (with the tube in a single position) 3. In Fourth Generation CT scanners, a view is a set of rays that strike a single (specific) detector as the tube rotates around the patient making an exposure. 4. The value of each ray is directly proportional to the transmitted photon measured by each of the detectors and characterized as a CT number. 5. The data measured in each view is called “raw data” The final step in digitization of the image is called quantization. In quantization, the analog signals are changed into a digital array so that they can be sent on to the CT computer. An integer (CT number) is assigned to each of the amplified signals in the form of a positive or negative whole number. The value of the assigned integer is based upon the strength of the signal emanating from the patient’s body. The greater the signal, the greater the numerical value of the integer. The Module contains a lot of information on the physical parameters associated with CT, but there is still more information to come. Module F will begin where Module E left off, and in addition, will further delve into CT instrumentation and how instrumentation affects the CT process. Review this module and make sure that you have a firm grasp of the principles presented. If you need further clarification, please see chapters three and four of the Seeram’s text. Copyright © Southern Union State Community College, 2007. 9