nursing process focus
advertisement

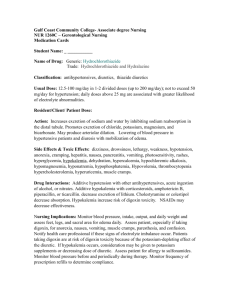
Nursing Process Focus: Patients Receiving Chlorothiazide (Diuril) Assessment Potential Nursing Diagnoses Prior to administration: Comfort, impaired, nausea/vomiting, related to effects Obtain complete health history including allergies, drug history and of chlorothiazide possible drug interactions Falls, risk for, related to orthostatic hypotension secondary to Assess for presence/history of serious kidney dysfunction, hypokalemia, medication decreased liver function, diabetges Knowledge, deficient, related to mellitus, decreased liver function effects of thiazide diuretics Lab values for CBC, BUN, creatinine, Fluid volume, deficient, related to electrolytes, uric acid, blood glucose excessive dose of chlorothiazide Obtain vital signs Noncompliance, recommended medication regime, related to Assess for peripheral edema unpleasant side effects, Obtain body weight misunderstanding of need to take medication exactly as ordered Planning: Patient Goals and Expected Outcomes Patient will Take medication as ordered, without increasing or decreasing unless recommended by health care provider Experience no side effects or adverse reactions Experience increased urinary output, decreased blood pressure Demonstrate knowledge of mechanisms of action of chlorothiazide Demonstrate knowledge of eating potassium-rich diet or of taking potassium supplement, but not both unless specifically recommended by health care provider Implementation Interventions and (Rationales) Patient Education/Discharge Planning Obtain history of drug allergies. Instruct patient to report all allergies to (Chlorothiazide is a sulfonamide, so the health care provider. it patient is sensitive to one sulfa drug, he/she will not be able to take it.) Monitor renal function. Instruct patient to monitor intake and (Chlorothiazide cannot be given to output and report changes in urine patient with severe renal amount to health care provider. dysfunction or anuria.) Instruct patient to: Monitor potassium levels. (Chlorothiazide decreases Recognize signs and symptoms of potassium levels, patient must be hypokalemia, including leg cramps, monitored closely for normal levels nausea, vomiting, cardiac dysrhytmias. throughout therapy.) Report symptoms to health care provider Add potassium rich foods to diet such as citrus fruit and melons Instruct patient to: Monitor blood glucose closely. Report consistent hyperglycemia to the health care provider Monitor blood sugar levels if patient is diabetic or pre-diabetic. (Chlorothiazide may cause hyperglycemia and glycosuria. Patient may need dosage adjustments of hypoglycemic drugs.) Monitor for gout. (Patient with gout Instruct patient to report worsening of may experience hyperuricemia symptoms of gout to the health care without symptoms, secondary to provider. chlorothiazide’s interference with uric acid excretion.) Monitor intake and output for Instruct patient to report either oliguria equality between intake and output or extreme diuresis immediately. in a 24-hour period. (Excessive diuresis, or oliguria, can lead to electrolyte imbalances.) Teach patient/caregivers: Provide safe environment. (Chlorothiazide may cause Measures to decrease falls if Orthostatic hypotension placing orthostatic hypotension occurs patient at risk for falls.) To change position slowly, rise slowly Evaluation of Outcome Criteria Evaluatge the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). Nursing Process Focus: Patients Receiving SPIRONOLACTONE (Aldactone) Assessment Prior to administration: Obtain complete health history including allergies, drug history and possible drug interactions. Vital signs Serum, electrolytes, creatinine, CBC, ABGs, BUN) Obtain body weight Assess for presence/history of decreased liver or kidney function Potential Nursing Diagnoses Body image, disturbed (gynecomastia in males, hirsutism in females) related to anti-estrogen effects of spironolactone Diarrhea, related to side effects of medication Fluid volume, deficient, risk for, related to excessive doses of spironolactone Knowledge, deficient, related to no effects of medication Planning: Patient Goals and Expected Outcomes The patient will: Experience increased diuresis. Exhibit decreased or absent edema or crackles. Demonstrate blood pressure and potassium values within normal limits Demonstrate knowledge of mechanisms of action of spironolactone, side effects and adverse reactions Mainatain absence of diarrhea Implementation Interventions and (Rationales) Patient Education/Discharge Planning Monitor renal function. Instruct patient to report changes in (Spironolactone cannot be used if urinary output to the health care anuria, worsening decreased kidney provider. function, or acute renal insufficiency is present. Use cautiously if BUN is 40 or above.) Monitor serum potassium levels Advise patient regarding signs and results for impending hypokalemia or symptoms of hypokalemia or hyperkalemia. (The patient is at risk hyperkalemia including leg cramps, for cardiac dysrhytmias.) nausea, vomiting, irregular heart rhythm. Monitor daily weight and intake and output (to determine fluid loss). Instruct patient/caregivers to: Weigh daily or on schedule recommended by health care provider, and record, and report changes of >3 pounds if doing daily weights, or >5 pounds if once weekly weights Weigh at same time every day, same scale, and in same amount of clothing, in order to get most accurate weight possible Monitor for symptoms of metabolic Instruct patient caregivers to monitor acidosis. for drowsiness, restlessness. Instruct patient to: Monitor diet for food high in potassium (may lead to Avoid foods with high potassium hyperkalemia). content (bananas, oranges, orange juice, dried apricots, Sanka, etc.) Avoid use of potassium-based salt substitutes, and to get permission of health care provider before using any salt substitute Monitor for side effects/adverse Advise patient/caregiver to be aware of reactions. and report: nausea/vomiting, diarrhea, burning of tongue, lethargy, confusion, headache, dizziness, drowsiness, gout, rash, or urticaria Monitor for sexual changes. (Patient Instruct patient/caregiver to report may experience decreased libido, changes to health care provider hirsutism in females, gynecomastia immediately, but not to abruptly and/or impotence in males, irregular discontinue taking spironolactone menses or possibly amenorrhea, postunless recommended by health care menopausal bleeding, or deepening of provider. the voice in females.) Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). NURSING PROCESS FOCUS: Patients Receiving SODIUM BICARBONATE Assessment Potential Nursing Diagnoses Prior to administration: Gas exchange, impaired, related to acidosis or alkalosis Obtain complete health history including allergies, drug history and possible drug Fluid volume excess, related to interactions bicarbonate Assess for presence/history of metabolic Knowledge, deficient, related to proper acidosis or alkalosis, cardiovascular disease, use of sodium bicarbonate decreased renal function, peptic ulcer disease Obtain vital signs Monitor ABGs Planning: Patient goals and Expected Outcomes Patient will: Demonstrate reversal of symptoms of acidosis or alkalosis Demonstrate pH between 3.5-5.3, and sodium level between 135-145 Demonstrate understanding of proper uses/application of sodium bicarbonate products Implementation Interventions and (Rationales) Patient Teaching/Discharge Planning Monitor for alkalosis. (Indicates drug Advise patient and caregiver regarding effectiveness.) symptoms of alkalosis: irritability, confusion, cyanosis, slow respirations, irregular pulse, muscle twitching. Monitor for metabolic acidosis. (Sodium Advise patient and caregiver regarding bicarbonate is used to neutralize acidosis.) symptoms of acidosis: sleepiness, coma, disorientation, dizziness, headache, seizures, hypoventilation. Monitor respirations, pulse, lung sounds, Advise patient that frequent vital signs fluid balance, pH, ABGs. checks and lab studies will be performed. Monitor for decreased renal function. Advise patient that intake and output (Drug will not be excreted, leading to balance, pH of urine, daily weight will be metabolic alkalosis.) done. Monitor for hyponatremia: elevated blood Advise patient regarding symptoms of pressure, cold, clammy skin, anorexia, hyponatremia and to notify health care vomiting, diarrhea, abdominal cramps provider/health care provider if he/she lethargy, fatigue, confusion, headache, notes any of symptoms listed in previous seizures, coma, tremors column Monitor for hypokalemia. Advise patient regarding symptoms of hypokalemia including muscle cramps, nausea, irregular heart rhythm and to report symptoms to health care provider Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). NURSING PROCESS FOCUS: Patients Receiving POTASSIUM CHLORIDE Assessment Potential Nursing Diagnosis Prior to administration: Falls, risk for, R/T adverse reactions to Obtain complete health history including medication allergies, drug history and possible drug Knowledge, deficient, proper use of interactions. medication, R/T no previous exposure Assess for presence/history of severe renal Skin integrity, impaired, risk for, R/T disease, hypokalemia, hyperkalemia, extravasation at IV site dehydration, acidosis or alkalosis, cardiac Therapeutic regimen management, dysrhythmias ineffective, R/T lack of understanding regarding other medication/food use Urinary elimination, impaired, decreased urinary output, R/T medication use PLANNING: PATIENT GOALS and EXPECTED OUTCOMES Patient will: Remain free of physical injury Demonstrate knowledge of drug therapy, side effects, and adverse reactions Maintain intact skin integrity Demonstrate understanding of possible drug interactions Maintain urinary elimination within normal range Implementation Interventions and (Rationales) Patient Teaching/Discharge Planning Monitor serum potassium levels Instruct patient to be aware of symptoms (indicates effectiveness of therapy) of hyperkalemia: nausea, abdominal cramping, oliguria, weakness, changes in heart rate, numbness or tingling of arms or legs Monitor kidney function. (Damaged Advise patient and caregiver regarding kidneys are unable to excrete normal the importance of kidney function tests amounts of potassium, leading to and of complete disclosure of past hyperkalemia.) medical history. Instruct patient to: Monitor diet for excessive foods containing potassium. (There is a risk for Avoid use of salt substitute without hyperkalemia resulting in cardiac approval of health care provider dysrhythmias. Patient receiving Avoid increasing potassium rich foods potassium supplements should avoid use while taking a potassium supplement, of salt substitute since most use including bananas, oranges, orange juice, potassium in place of sodium.) broccoli, carrots, brussel sprouts, etc. Monitor for overdose. (Patient is at risk Advise patient and caregiver that for cardiac dysrhythmias.) frequent blood studies will be done so early hyperkalemia will be identified. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”).