Pyelonephritis (P)
advertisement

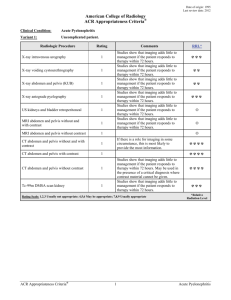
Pyelonephritis (P). Simple complement : 1.Which clinical syndrome in the evolution of pyelonephritis is characteristic for little children? A. Astenic syndrome B. Dysuric syndrome C. Dyspeptic syndrome D. Lombar pains E. Neurovegetative syndrome 2.Which is the screening method in the diagnosis of pyelonephritis? A. Cystography and urography B. Ultrasonography of kidneys and urinary bladder C. Renal scintigraphy and renal urography D. CT-scan E. Cystoureteroscopy 3.Which is the more frequent causal pathogene agent in the development of pyelonephritis in children? A. Staphylococcus B. Proteus C. Clebsiella D. Escherichia coli E. Mycoplasma 4.The pathologies which lead to urine passage disorders are the follows, except: A. Vesico-ureteral reflux B. Cystitis C. Nephroptosis D. Neurogene urinary bladder E. Nephrolithiasis 5.The chronic inflammatory process in urinary bladder is influenced by the following factors, except: A. Vulvitis B. Gastritis C. Helminths infestation D. Constipations E. Changes of intestinal microflora 6. In a 3 years aged child the diagnosis of urinary tract infection was established; this being the first documented episode. Which examination includes the imagistic evaluation? A. Urography B. Cystography C. Abdominal echography D. Kidneys scintigraphy and urography E. No one from above mentioned 7. A 5 years aged girl, formerly healthy, is diagnosed with acute pyelonephritis. Which laboratory index is not essential for the diagnosis at moment? A. Urea, creatinine B. General analysis of urine C. Serum cholesterol, uric acid D. Uroculture E. Analysis of urine by Neciporenco 8.A 9 years aged girl presents complaints on periodic abdominal pains, dysuria. In general urine analysis the leucocyturia is present. First time she falled ill in 6 years age, when the pains in lombar region, periodically leucocyturia have appeared. Which examination is not obligatory at moment? A. General analysis of urine B. Ultrasonography C. Uroculture D. Renal biopsy E. Clearence of creatinine 9. Which investigation is not indicated in the case of enuresis? A. Familial anamnesis B. Complete physical examination C. Voiding rhythm D. Renal biopsy E. Cystography 10. Which reno-urinary pathology is manifesting with pneumaturia? A. Glomerulonephritis B. Alport syndrome C. Cystitis D. Pyelonephritis E. Vesico-ureteral reflux 11.Which pathology don’t need to perform the differential diagnosis from cystitis ? A. Diabetes mellitus B. Urinary tract infection C. Pelvian tumor D. Ulcerative nonspecific colitis E. Vulvovaginitis 12. Which is not characteristic for chronic cystitis? A. Dysuria B. General state affection C. Leucocyturia, microhematuria D. Hypercholesterolemia E. Thickening of urinary bladder wall on ultrasonography 13. In which case the exacerbation of chronic pyelonephritis has place? A. Phytotherapy administration B. Chronic infection foci exacerbation C. Antirecidivant treatment indication D. The pacient suffers by acute gastritis E. Abundant liquids intake 14.Which medicinal herb have expressed antiinflammatory action? A. Wild rose B. Bear grape C. Milfoil D. St.John’s wort E. Plantain Multiple complement : 1. Which are the indications for cystography in the case of urinary tract infection ? A. Dysuria B. Enuresis C. Renal colic D. Arterial hypertension E. Pollakiuria 2. Which imagistic methods confirm the diagnosis of pyelonephritis in children ? A. Urography B. Renal scintigraphy C. Renal ultrasonography D. X-ray chest E. Cystoscopy 3. Which are the risk factors in the development of pyelonephritis in children? A. Chronic infection foci B. Recurrent infections C. Deficient anemia D. Acute gastroduodenitis E. Vulvovaginites and cystites 4. Which clinical manifestations are characteristic for pyelonephritis in little children ? A. Anemia B. Abdominal pain C. Fever D. Dispeptic disorders E. General signs of intoxication 5. Which are the risk factors for pyelonephritis development in children? A. Hydronephrosis B. Urolithiasis C. Renal tumor D. Alport syndrome E. Polycystic kidney disease 6. Which are the antenatal predisposing factors in the development of pyelonephritis in children? A. Nephropathy during pregnancy B. Chronic pyelonephritis in pregnant women C. Acute atopic dermatitis D. Recurrent viral infection in pregnant women E. Chronic infection foci in pregnant women 7. Which are the contraindications for urography performing? A. Increased sensibility to iodine B. Shock, collapse C. Oliguria, anuria, increased urea values D. Renal colic E. Active tuberculosis process 8. Pyelonephritis must be differentiated from : A. Glomerulonephritis B. Renal tuberculosis C. Cystitis D. Acute bronchitis E. Hepatitis 9. The criteria of pyelonephritis diagnosis are: A. Complex of symptoms (intoxication, fever, pain) B. Leucocyturia C. Bacteriuria 103 D. Bacteriuria 105 E. Hematuria 10. Which is the treatment of acute pyelonephritis slight form? A. Rest in bed 1-2 days after the temperature normalizing B. Increased liquids intake C. Corticosteroids D. Cephalosporins by II and III generation E. Biseptol 11. Pyelonephritis in new-born and suckling babies occurs under the form of: A. Sepsis B. Enterocolitis C. Anemia D. Acute respiratory viral infection E. Alimentary allergy 12. Which are the indications for urography? A. Renal colic B. Arterial hypertension C. Abdominal trauma D. Acute tuberculosis process E. Oliguria 13.What is the treatment of severe form of acute pyelonephritis? A. Antibacterial infusion therapy B. I/v perfusions C. Antioxidant therapy D. Immunosuppressors E. Desaggregants 14. Which are the indications for mictional cystography ? A. Pyeloectasis B. Enuresis C. Abdominal trauma D. Presence of residual urine after voiding in renal echography E. Arterial hypertension 15. Which are the most frequent clinical manifestations of pyelonephritis in over 3 years aged children ? A. Pains in lombar region B. Dysuria C. Diarrhea D. Abdominal pains E. High fever 16. The organic type enuresis is determined by : A. Anomalies of urinary tract B. Vesico-ureteral reflux C. Distal urethral stenosis D. Hereditary predisposition E. Conflicting situations in family 17. Which are the principal clinical symptoms of ,,cystic syndrome’’ ? A. Suprapubian abdominal pains B. Pollakiuria C. Headache D. Pains in lombar region E. Dysuria 18. Which includes the etiologic classification of cystites? A. Infectious cystitis B. Medicamentous cystitis C. Fibrinous cystitis D. Parasitary cystitis E. Catarrhal cystitis 19. Which clinical manifestations are characteristic for cystitis ? A. Vesical tenesms with pollakiuria B. Turbid urine with unpleasant smell C. Pains in the inferior part of abdomen D. Bacteriuria, leucocyturia, microhematuria E. Increased urea 20. The pathogenesis of pyelonephritis is determined by: A. Microbial agent B. Viral infections C. Genetic predisposition D. Immune system state E. Infected urinary passage 21. The following states contribute to chronic occurrence of pyelonephritis: A. Gastroduodenitis B. Renal dysplasia C. Vesico-ureteral reflux D. Bronchitis E. Neurogene urinary dysfunction 22. Which evolutive forms are characteristic for acute pyelonephritis? A. Recurrent B. Slight C. Medium D. Latent E. Severe 23. Which are the risk factors for pyelonephritis in postnatal period in little age infants? A. Prematurity B. Intrauterine infection C. Developmental anomalies of urinary system D. Changes of intestinal microflora E. Bronchitis 24. The differential diagnosis of chronic cystitis in children is performing with the following pathologies: A. Neurogene urinary dysfunction B. Gastroduodenitis C. Pyelonephritis D. Vulvovaginitis E. Urethritis