Microbiology 65 [5-11
advertisement
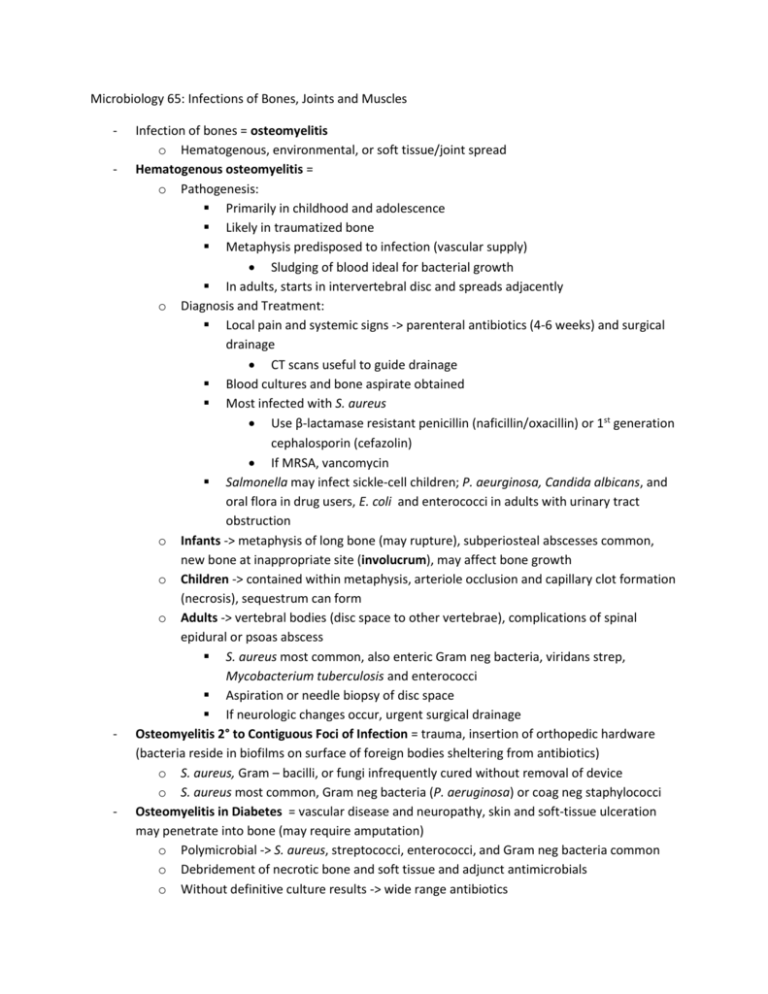
Microbiology 65: Infections of Bones, Joints and Muscles - - - Infection of bones = osteomyelitis o Hematogenous, environmental, or soft tissue/joint spread Hematogenous osteomyelitis = o Pathogenesis: Primarily in childhood and adolescence Likely in traumatized bone Metaphysis predisposed to infection (vascular supply) Sludging of blood ideal for bacterial growth In adults, starts in intervertebral disc and spreads adjacently o Diagnosis and Treatment: Local pain and systemic signs -> parenteral antibiotics (4-6 weeks) and surgical drainage CT scans useful to guide drainage Blood cultures and bone aspirate obtained Most infected with S. aureus Use β-lactamase resistant penicillin (naficillin/oxacillin) or 1st generation cephalosporin (cefazolin) If MRSA, vancomycin Salmonella may infect sickle-cell children; P. aeurginosa, Candida albicans, and oral flora in drug users, E. coli and enterococci in adults with urinary tract obstruction o Infants -> metaphysis of long bone (may rupture), subperiosteal abscesses common, new bone at inappropriate site (involucrum), may affect bone growth o Children -> contained within metaphysis, arteriole occlusion and capillary clot formation (necrosis), sequestrum can form o Adults -> vertebral bodies (disc space to other vertebrae), complications of spinal epidural or psoas abscess S. aureus most common, also enteric Gram neg bacteria, viridans strep, Mycobacterium tuberculosis and enterococci Aspiration or needle biopsy of disc space If neurologic changes occur, urgent surgical drainage Osteomyelitis 2° to Contiguous Foci of Infection = trauma, insertion of orthopedic hardware (bacteria reside in biofilms on surface of foreign bodies sheltering from antibiotics) o S. aureus, Gram – bacilli, or fungi infrequently cured without removal of device o S. aureus most common, Gram neg bacteria (P. aeruginosa) or coag neg staphylococci Osteomyelitis in Diabetes = vascular disease and neuropathy, skin and soft-tissue ulceration may penetrate into bone (may require amputation) o Polymicrobial -> S. aureus, streptococci, enterococci, and Gram neg bacteria common o Debridement of necrotic bone and soft tissue and adjunct antimicrobials o Without definitive culture results -> wide range antibiotics - Chronic Osteomyelitis = can remain dormant, exacerbations from purulent drainage, antibiotic therapy useful, can cause progressive destruction Joint Infections - - Swollen, red, warm, painful joint with fever -> septic arthritis Noninfectious inflamm joint disease from gout, pseudogout, RA, CT disease or viruses Infection supported by high WBC (neutrophils), Gram stain +, absences of other causes Inflammatory reaction in synovial fluid from serum protein, phagocytes, and microorganism interaction Bacterial infections more common and have higher WBCs in fluid (neutrophils) o S. aureus most common in all, H. influenza type B, in kids, Kingella kingae in kids < 2, gonococcus in sexually active adults Treatment: o High dose antibiotic therapy parenterally o Drain synovial fluid (aspiration before surgery) Open drainage in hip joint to prevent necrosis of head of femur o Complete therapy with oral agent o 3-4 treatment Muscle Infections - - - Myalgias prominent in viral illness, rikettsial infections, osteomyelitis, endocarditis Involvement of microorganism is indirect (acute-phase response) -> accelerated catabolism of muscle (by macrophage products monokins, IL1 and TNF) o Symtoms from increase prostaglandin E2 synthesis, IL1 and TNF hypothalamic interaction (fever) Aspirin helps solve fever Specific muscle infections: o Invaded from either contiguous site or hematogenous spread o Crepitus (gas in muscle) suggest gas gangrene from Clostridum perfringens o Generalized muscle pain and peripheral eosinophilia, pork -> trichinosis Treatment: o Directed toward eradication of organism once identified o Drainage of abscesses and surgical debridement may be neccessary