URINARY SYSTEM
advertisement

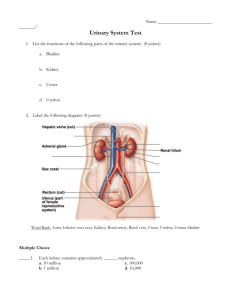
URINARY SYSTEM This is the KIDNEYS, URETERS, URETHRA, and BLADDER. Not many structures, but very important. Functions: 1. Regulate electrolytes (K, Na, etc) in body 2. Regulate pH in blood 3. Regulate blood pressure 4. Regulate blood volume by removing excess water from blood. 5. Removing metabolic wastes (chemicals, such as nitrogen, produced by chemical reactions in the body are excreted). This is the least important of the kidney’s functions. You can survive for a few weeks without excreting waste products in the urine, but hour by hour, the other functions are more important. LOCATION OF THE KIDNEYS They are retroperitoneal and are located in the abdominal cavity. They are at the level of T12 to L3, so they are at the costal margin, and the ribs protect them a little. Even though they are protected by thoracic ribs, they are NOT in the thoracic cavity because they are below the diaphragm. STRUCTURES WITHIN THE KIDNEY The RENAL CAPSULE surrounds the kidney, dense fibrous connective tissue. A layer of adipose tissue surrounds the capsule, called PARARENAL FAT (ADIPOSE). It cushions and protects. Around that is a connective tissue layer = RENAL FASCIA, made of loose connective tissue. It anchors the kidney to the surrounding peritoneum and abdominal wall. Not very strong. Jumping up and down can cause tearing. Watch out for the old gym equipment with the vibrating bands around the waist! Gross Anatomy of the Kidneys The most superficial layer of the kidney is the RENAL CORTEX. The deeper layer is the RENAL MEDULLA. Renal medulla is made up of RENAL PYRAMIDS. The deepest layer is the RENAL PELVIS This layer contains the CALYX where the renal Pyramids drain. The calyx empties into the URETER 1 You can’t understand how the kidney works until you understand how blood flows in the kidney. The RENAL ARTERY supplies the kidney, and goes on to branch between each set of renal pyramids = INTERLOBAR ARTERIES. Interlobar arteries have anastomoses in the renal cortex = ARCUATE ARTERIES (form arcs). These further branch into INTERLOBULAR ARTERIES. AORTA RENAL ARTERY SEGMENTAL ARTERIES INTERLOBAR ARTERIES ARCUATE ARTERIES (form arcs) INTERLOBULAR ARTERIES The veins follow the arteries and have the same names: INTERLOBULAR VEIN ARCUATE VEIN INTERLOBAR VEINS SEGMENTAL VEINS RENAL VEIN INF VENA CAVA. Interlobar artery Interlobular arteries Arcuate arteries MICROSCOPIC ANATOMY OF THE KIDNEY Just like the unit of function of the lungs is the alveolus, the unit of function of the kidney is the NEPHRON. Each kidney has about 1 million nephrons. Each one carries out all of the various functions of the kidneys. Diagram of nephron GLOMERULUS PROXIMAL CONVOLUTED TUBULE LOOP OF HENLE 1. DESCENDING LIMB (thick and thin portions) 2. ASCENDING LIMB (thick and thin portions) DISTAL CONVOLUTED TUBULE COLLECTING DUCT. 2 Where do the nephrons fit into the whole kidney? The upper half is in the renal cortex, and the lower half is in the renal medulla. JUXTAGLOMERULAR APPARATUS The distal end of the renal tubule passes next to the glomerulus to form the juxtaglomerular apparatus (juxta means “next to”). The juxtaglomerular apparatus (JGA) consists of cells located in and around the glomerulus and the glomerular capsule. If blood pressure is too low, the JGA releases adenosine, which causes vasoconstriction of the afferent arteriole. This will slow the filtration rate so less water is lost, and blood pressure increases. if the blood pressure is still too low after adenosine has caused vasoconstriction, the JGA secretes the hormone renin . Renin causes more sodium to be reabsorbed, and water follows, so blood volume increases, so blood pressure increases. GLOMERULUS The glomerulus is the first part of the nephron, where the filtration occurs. The glomeruli are located only in the renal cortex. A glomerulus (“ball of yarn”) is a tuft of capillaries surrounded by a glomerular capsule (Bowman’s capsule) made of simple squamous epithelium. The glomerulus fits in the capsule like a fist punched into an underinflated balloon. The capsule collects the plasma from the arterioles and drains it into the convoluted tubules, which empty into a collecting tubule, which exits the body. The plasma is further filtered along the way. The juxtaglomerular apparatus (JGA) consists of cells located in and around the glomerulus and the glomerular capsule. Normally at the end of the capillary bed you have venuoles. But this is the only part of the body that is different: here we have another arteriole, called the EFFERENT ARTERIOLE, which takes blood away from the glomerulus. 3 The efferent arteriole drops down straight, next to the Loop of Henle. While it is straight, it is called VASA RECTA (straight capillaries). There are capillaries that come off the efferent arteriole which surround the loop of Henle. Here, they are called peritubular capillaries. They then leave the area to become the interlobular vein, which leaves the kidney. FUNCTION OF THE NEPHRON Blood comes in from the AFFERENT ARTERIOLES. Plasma leaks out of the afferent arterioles and enters the glomerular capsule. The plasma contains nutrients, waste products, etc. As the plasma moves through the proximal convoluted tubule, all of the nutrients, and most of the water, and most of the ions are absorbed back out of the nephrons and into the blood. In the Loop of Henle, almost all of the rest of the water and salt are removed blood. Everything that is not reabsorbed (the waste products) goes into the collecting duct and is excreted as urine. This is also how the water-salt balance is maintained, as well as the acid-base balance. In the Loop of Henle, almost all of the rest of the water and salt are removed blood. In the distal convoluted tubule, the rest of the water and salt are removed. The rest of the liquid goes into the collecting duct. The distal convoluted tubule and the collecting duct fine-tune the water and salt absorption and excretion. If you are well hydrated, the water will be allowed to leave urine. If you are thirsty, the water will be absorbed. The purpose of the capillary bed is to absorb these things from the nephron into the blood. Diuretics are medicines that increase the amount of urine that is produced. People who have high blood pressure might be prescribed diuretics to decrease the blood volume. Alcohol is a diuretic and this is what contributes to the symptoms of a hangover. The best way to prevent a hangover after drinking is to consume a lot of water before you go to bed. Caffeine is also a diuretic, so coffee and regular Coca-cola are diuretics. HISTOLOGY OF THE NEPHRON 4 Cells that form the visceral layer have spaces between them to allow the plasma to leak out, called FILTRATION SLITS. A lot of fluid leaks out of the capillaries, so they are what kind? FENESTRATED CAPILLARIES. PROXIMAL AND DISTAL CONVOLUTED TUBULES This area absorbs nutrients, water, and salt. Only about 1% of the fluid filtered by the kidney actually becomes urine. LOOP OF HENLE This is where water is reabsorbed. It is located in the renal medulla. Urine Production Filtration – filtrate of blood leaves kidney capillaries Reabsorption – most nutrients, water, and essential ions reclaimed Secretion – active process of removing undesirable molecules COLLECTING DUCT (COLLECTING TUBULES) Receives urine from distal convoluted tubules, empties into ureter. Things can happen to the kidney: infection, excess proteins, pH change, blood pressure drops, and can lead to kidney failure. Treatment for kidney failure is DIALYSIS, which removes blood, send it through a filter, and return it without the wastes. It is done three times a week, about 6 hours a day. Ideally, they need a kidney transplant because the kidney has other functions as well. The brain, heart, and kidney are the only three organs in the body that have to get oxygen to sustain life. 5 URETERS These are long tubes that connect the renal pelvis to the urinary bladder. HISTOLOGY 1. MUCOSA a. TRANSITIONAL EPITHELIUM lines the mucosa. It can change in thickness so it can stretch. b. LAMINA PROPRIA has lots of elastic tissue, recoils to original size. 2. MUSCULAR LAYER (both layers are smooth muscle) a. INNER CIRCULAR b. OUTER LONGITUDINAL The function of these is peristalsis (you can pee upside down!) 3. ADVENTITIA (dense connective tissue layer which becomes looser connective tissue). This provides protection, strength for organs, and attaches ureters to surrounding structures. URINARY BLADDER The histology here is identical to ureter except mucosal layer has folds called RUGAE which allow for expansion. The mucosal folds in the bladder (rugae) have the same basic function as transitional epithelium—accommodating stretch as the bladder fills. You can hold up to one liter of urine, although at 500 ml, you’ll be dancing. Also, the muscle layer is thicker and is called the DETRUSOR MUSCLE, which contracts to allow emptying of the urinary bladder. The function of the urinary bladder is just to store urine. The URETER enters in at the base of the urinary bladder, not the top. As the bladder fills, it presses down on the ureters to prevent urine from backing up into the kidneys. 6 The TRIGONE is a triangular area where the ureters come in and the urethra goes out. Between the urethra and the urinary bladder are two sphincters: 1. INTERNAL URETHRAL SPHINCTER: smooth muscle 2. EXTERNAL URETHRAL SPHINCTER: skeletal muscle. Although it is primarily under voluntary control, it will contract if the urine volume is too much. If the patient is in a coma or under anesthesia for a long time, the internal sphincter will be closed, like when you are asleep, so a catheter is needed to open it to drain the urine out. The URETHRA drains the urine to the outside. Its histology is the same as the ureter. The length differs from males to females: Females: 4cm Males 20 cm (varies with mood) Therefore, women (esp. little girls) are more susceptible to UTI. URETHRITIS = infection of the urethra CYSTITIS = inflammation (usually from infection) of the urinary bladder. UREA Urea is a waste product of amino acid metabolism. Remember, proteins are made of amino acids, so when you break down proteins, you break down amino acids, and the waste product left over is urea. This is the main waste product in urine. Excessive proteins can cause kidney damage, since they are acidic. COLOR OF URINE When you urinate, it should be clear with almost no yellow color. The more yellow the urine is, the more dehydrated you are. If the urine is very dark yellow, you are burning too much protein (as in food deprivation). This is often seen in diabetes. PROBLEMS WITH THE KIDNEY KIDNEY STONES These develop in the RENAL PELVIS for unknown reasons. Stones are made out of a variety of things: uric acid, calcium, cystine (an amino acid), or cholesterol. They keep growing. They can block the urethra, causing the kidney to enlarge. As the kidney stretches, the capsule stretches, causing excruciating pain in cycles of hours. As pressure builds up around the stone, urine can pass, and the kidney stone moves down the urethra slowly. Symptomatic kidney stones may be pea sized or larger (up to 1 ½ inches). Kidney stones get stuck in three places: 1. Renal pelvis 2. In the ureter as it bends over the common iliac artery 3. In the urinary bladder at the trigone. Treatment is ULTRASOUND LITHOTRIPSY Put a powerful speaker on the outside of the kidney, sends a shock wave which the tissues absorb, but the stones shatter so the pieces can pass easier. Can put a STENT 7 (1 ½ foot long tube) in to keep the vessel open along the entire length of the urethra. Insert under general anesthetic, remove without. To help prevent kidney stones, drink enough fluid so your urine stays clear and light colored. OTHER KIDNEY PROBLEMS Pyelitis is infection of the renal pelvis and calyces Nephritis is inflammation of the nephrons. Hydronephritis is excess fluid in the nephron. Cystitis is inflammation (usually from infection) of the urinary bladder. It is not normal to have glucose in the urine; that indicates diabetes. RENAL FAILURE Things can happen to the kidney: infection, excess proteins, pH change, blood pressure drops, and can lead to kidney failure. Treatment is DIALYSIS, which removes blood, sends it through a filter, and returns it without the wastes. Done three times a week. Ideally, need a kidney transplant because the kidney has other functions as well. The brain, heart, and kidney are the only three organs in the body that have to get oxygen to sustain life. What is Renal Failure? Renal failure occurs when your kidneys stop working. Our kidneys are very important to us because we use them to remove waste from our bodies And our kidneys keep the balance of water and salt in our body. If we are unable to regulate the water and mineral balance in our body, Renal Failure can be life threatening. Causes of Renal Failure 1. Medication / Poison / Infection People with long term health problems are most at risk to have kidney problems from medication. Antibiotics Pain Medication Blood Pressure Medicine Dyes used in X-rays 2. Sudden drop in blood flow. Heavy blood loss from an injury A serious infection (Sepsis) Severe Dehydration 3. Blockage of fluid out of the Kidney Kidney Stones Tumor(s) Enlarged Prostate Gland 8 Who is most likely to get Renal Failure? Kidney or Liver Disease Diabetes High Blood Pressure Heart Failure Obesity Bone Marrow Transplant Heart or Belly Surgery Symptoms of kidney failure Very little or no urine during urination If the body is unable to excrete potassium, the rising of potassium levels is associated with ventricular tachycardia and ventricular fibrillation. Lethal injections are excess potassium. Loss of appetite As waste accumulates, lethargy and fatigue become apparent to the point where mental function can decrease to coma. Body Weakness Because of low levels of erythropoietin produced by failing kidneys they do not stimulate the bone marrow which leads to a decrease in red blood cells. This leads to less oxygen throughout the body which leaves the body unable to do work. High Blood Pressure Because the kidneys can not deal with the rising acid levels in the body, breathing becomes more rapid as the lungs attempt to blow off carbon dioxide to buffer the acid levels. In doing so, fluid can be deposited in the lungs possibly causing congestive heart failure. Swelling of the legs and feet Nausea and or Vomiting Back pain below the rib cage, (Flank Pain) Some people may not have any symptoms (asymptomatic) Diagnosis of kidney failure Patients can be diagnosed by undergoing blood and urine tests: Blood: BUN (Blood Urea Nitrogen), Creatinine (Waste product levels), GFR (Glomerular Filtration Rate) Urine: Protein, Abnormal presence of White and Red blood cells, Electrolytes Patients can also undergo an Ultrasound to see if there are any obstructions. Treatment for kidney failure Treatments are based on the cause: Issue - Blood Loss - Restore blood flow - Medication / Poison - Stop taking the medication or poison - Blockage - Remove or bypass blockage 9 Also, the person treating the patient will attempt to stop the buildup of waste in the body. This may be done by dialysis. And the person treating the patient may also administer other medication to prevent the retention of excess fluid and minerals and prevent any further renal damage. -lowering Phophorus levels -production of Red Blood Cells -blood pressure medication Prevention of kidney failure Regulate Blood Pressure Regulate Sugar Intake Regulate Protein Intake Once the kidney fails the only options are dialysis and transplantation. SAMPLE URINALYSIS Values APPEARANCE BACTERIA BILIRUBIN COLOR EPITHELIAL CELLS ERYTHROCYTES GLUCOSE HEMOGLOBIN HYALINE CASTS KETONES LEUKOCYTE ESTERASE LEUKOCYTES NITRITE PH PROTEIN SPECIFIC GRAVITY UROBILINOGEN Results CLEAR MODERATE NEGATIVE AMBER FEW 3-5/HPF (High) NEGATIVE NEGATIVE 0-4/LPF 1+ 1+ 6-10/HPF (High) NEGATIVE 6.5 TRACE 1.029 0.2 Normal CLEAR NEG NEG Straw FEW 0-2 NEG NEG 0-4 NEG NEG 0-2 NEG 4.5-8.5 NEG 1.003-1.035 <1.0 HPF = high power field LPF = low power field 10 Urinalysis: What Does It All Mean? How to perform test 1. Midstream catch is acceptable 2. Should be examined within 2 hours 3. Should be refrigerated if not read immediately Urine Specific Gravity (USG) Purpose: urine osmolality and represnts patients’ hydration status and concentrating ability of their kidneys Normal: 1.003-1.030 Increased USG: glycosuria, SIADH Decreased USG: diuretic use, DI, adrenal insufficiency, aldosteronism, impaired renal fx NOTE: if intrinsic renal insufficiency, USG fixed at 1.010 Urinary pH Purpose: urinary pH reflects serum pH except in renal tubular acidosis (RTA), useful for diagnosis/management of UTIs and calculi Normal: 4.5-8.0, slightly acidic usually (5.5-6.5) Alkaline urine: suggest urea-splitting organism Acidic urine: uric acid calculi Hematuria Criteria: 3 or more RBC per HPF in 2 of 3 urine samples Testing: for peroxidase activity, will be positive in hematuria, myoglobinuria, hemoglobinuria -if positive: must look at micro to confirm presence of RBCs Types: glomerular, renal, urologic Proteinuria Criteria: >150 mg/day (10-20mg per dL) -microalbuminuria= 30-150 mg/day (sign of early renal disease) Normal urinary proteins: albumin, serum globulins, proteins secreted by the nephron Testing: reagant sensitive to albumin, but can miss low levels of globulins -Positive results: 5-10mg/dL -Dipstick results: 1+ = 30 mg/dL 2+ = 100 mg/dL 3+ = 300 mg/dL 4+ = 1,000 mg/dL 11 -Types: transient and persistent -Transient: temporary change, benign, self-limited (ex: orthostatic proteinuria that results from prolonged standing, but negative U/A after recumbency) -Positive test: Repeat U/A -Persistent has 3 types: glomerular, tubular, overflow -Glomerular: albumin primary urinary protein -Tubular: malfunctioning tubule cells, low-molecular-weight proteins (LMWP) predominate over albumin, rarely exceed 2 g/day -Overflow: LMWP overwhelm ability of tubules to reabsorb -Positive test: Perform 24-hour urinary protein excretion or spot urinary protein-creatinine ratio and micro analysis Glycosuria Normal: almost completely reabsorbed in proximal tubule Criteria: occurs at approximately 180-200 mg/dL Elevated: DM, Cushing’s syndrome, liver and pancreatic disease, Fanconi’s syndrome Ketonuria Normal: not present in urine Testing: presence of acetic acid through a chemical reaction Causes: uncontrolled diabetes, pregnancy, carbohydrate-free diets, starvation Nitrites Normal: Not present in urine Testing: bacteria that reduce urinary nitrates to nitrites -Positive test: can be gram negatives or gram positive organism (neg > pos) -Indicate significant number (>10,000/mL) -Negative test: Can’t R/O UTI because non-nitrate reducing organism cause UTIs -NOTE: nitrite stick sensitive to air exposure: after one week of exposure about 1/3 of strips give false positive Leukocyte Esterase Testing: presence of neutrophils Sterile Pyuria: -Organisms: Chlamydia and Ureaplasma urealyticum 12 -Other causes: balantis, urethritis, TB, bladder tumors, viral infx, nephrolithiasis, foreign body, exercise, glomerulonephritis, corticosteroid, cyclophosphamide use Bilirubin and Urobilinogen Normal Bilirubin: no detectable amounts -Unconjugated bili: not water soluble, doesn’t pass through glomerulus -Conjugated bili: water soluble, indicates possible liver dysfunction or biliary obstruction Normal Urobilinogen: only small amounts -Urobilinogen: end product of conjugated bili after metabolized by intestine, small amount reabsorbed into portal circulation and filtered by glomerulus Increased urobilinogen: hemolysis, haptocellular disease Decreased urobilinogen: antibiotic use, bile duct obstruction FUN URINARY TRACT DISCUSSION QUESTIONS Can you drink your own urine? Although urine is pretty clean, the exit tube (urethra) is not, so as it comes out, it gets contaminated like a garden hose with mud on the tip. Is it more sanitary to be spit on or peed on? If you are stranded on a desert island, should you drink seawater or your own urine? Why do I have to go to the bathroom immediately after a cup of coffee? Why do you have to pee when you hear water dripping? Does cranberry juice cure urinary tract infections? 13