data collection and analysis in the icu
advertisement

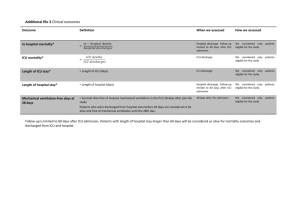
Anesthesiology Clinics of North America Volume 15 • Number 4 • December 1997 Copyright © 1997 W. B. Saunders Company 879 Critical Care Medicine in Transition: The Anesthesiologist's Role DATA COLLECTION AND ANALYSIS IN THE ICU Charles G. Durbin, Jr, MD From the Surgical Intensive Care Unit, University of Virginia Health Sciences Center, Charlottesville, Virginia Address reprint requests to C.G. Durbin, Jr, MD Department of Anesthesiology Box 10010 University of Virginia HCS Charlottesville, VA 22906 ISSUES IMPORTANT TO CRITICAL CARE MEDICINE Two important factors have influenced the development of critical care units: Patients require rapid, specific interventions to prevent physiologic deterioration or death, and hospitals need to effectively and efficiently provide necessary levels of service. The first issue is patient and disease driven; the second is economic and practical. Anesthesiologists have been important contributors to the advancement of critical care because the profession has successfully addressed the same issues in operating rooms (OR) and postanesthesia care units. Among the many attributes of an anesthesiologist, two skills are especially significant for outstanding clinical practice--(1) the ability to lead a team of professionals inconspicuously and (2) the ability to analyze massive amounts of data efficiently and act rapidly on the results. Those are the unique strengths that ensure anesthesiologists a role in the future of critical care medicine (CCM). Major differences between OR and intensive care unit (ICU) practice discourage many anesthesiologists from beginning or continuing practice in the ICU. Long-term patient care issues; inadequate experience with nutritional support, infectious disease, and specific organ therapies; and a lower rate of payment for services have contributed to the lesser interest among anesthesiologists in pursuing careers in CCM. As the balance of financial incentives and career opportunities shifts from the OR toward 880 the ICU, the number of anesthesiologists regularly caring for the critically ill will increase. This article describes the breadth and types of data sources that are encountered in the critical care environment. Some are identical to those observed in the OR and some are unique to the ICU. Mastery of all the areas is not essential for every critical care practitioner, but, understanding the sources of data and how they impact on various decision makers will improve the effectiveness of anyone working in CCM. Changes in the routes of health care delivery will have a major impact on the ICU. Specific sources of information to be considered are physiologic data and monitoring, laboratory data, outcomes information and prediction systems, critical care research, and quality and cost information. This discussion is not meant to be exhaustive but to give the reader an introduction to those important areas. Similarities with OR practice are emphasized. The belief is that anesthesiologists are particularly qualified by personality, training, and experience to integrate multiple data sources and make appropriate decisions in the ICU. In that way, they can uniquely contribute to the continued growth and development of CCM and ensure the persistence of anesthesiology's influence in that vital area. The role of the perioperative physician will include providing care to patients in ICUs, understanding how care is integrated in the ICU, and prudently managing expensive resources. PHYSIOLOGIC DATA AND MONITORING As is the case in the OR, CCM practitioners are bombarded with a huge number of physical and physiologic measurements. Some of them are used as patient or equipment monitors; others are used for diagnosis. In many cases, the same measurement device is used for both monitoring and diagnosis. The distinction between data being used for monitoring and for diagnosis is often blurred. Confusion regarding use of the same device for monitoring and diagnosis has led to inappropriate risk-benefit analysis of particular monitors. Several years ago, Robin [38] called for a ban on the use of the Swan-Ganz catheter because it has never been shown to improve outcome in critically ill patients. Insertion of a pulmonary artery catheter is associated with significant risks, including the possibility of pulmonary artery rupture and death. The extreme position taken by Robin demonstrates a basic misunderstanding of the function of monitors and how effectiveness of monitoring can be assessed. The use of monitors is routine in the OR. "To monitor" means "to observe closely," and a "monitor" is an "advisor, informant, or counselor." Monitors are not active devices; they do not directly provide patient care; they can only advise or inform. In evaluating the effect of monitors on patient care, it is important to remember that fact. Monitoring is only the first step in initiation of action. The clinician selecting and using the monitor is the essential ingredient in quality patient care. Errors in the use of monitors can occur because of inadequate education, 881 inexperience, or inattention by the caregiver. Those sources of problems can result in an undesired patient outcome despite appropriate monitor selection and function. Figure 1 illustrates the process of acquiring data and performing an action in an ICU. The output from a monitor suggests that further testing is needed to confirm a specific diagnosis. After the results are acquired, a diagnosis is established and an action may be taken. For example: A ventilator monitor indicates a low exhaled minute volume (monitor output). The breathing circuit is examined (additional test) and a partial disconnection at the endotracheal tube is identified (diagnosis). The circuit is reconnected to the patient (action) and now the exhaled minute volume monitor shows a normal value (monitoring output). If a caregiver had not noticed (or heard) the monitor, had not found the disconnection, or had not reconnected the patient, harm might have occurred. In evaluating the impact or value of a particular monitor, it is important to recognize the additional steps necessary to affect patient outcome. A monitoring device is no better than the person using it. ALARMS AS MONITORS In life-threatening situations, additional diagnostic or confirmatory tests sometimes are bypassed and action is taken without a firm diagnosis, Figure 1. The output of a monitor often triggers additional tests before an action is taken. 882 as illustrated in Figure 2 . When a particular event is believed to cause an undesired or lethal outcome, action should be empirical, without delaying to more firmly establish the cause (diagnosis). Alarms are a special case of monitoring related to that type of situation. When the parameter being monitored falls outside of the safe range, a visual or auditory "alarm" is issued by the monitoring device. Once again, no change in patient treatment is instituted by the monitoring device; a caregiver must make the decision to act. Caregivers often have control over the limits that trigger the monitor alarm. Given the total system, it is not reasonable to expect that monitors, by themselves, will impact patient care in a positive way. Any time a monitor is evaluated for its impact on patient care, the action scheme discussed here must be taken into account. Because invasive monitors always involve direct patient risks, they can easily be shown to increase morbidity. It is more difficult (if not impossible) to show they improve patient outcome because it is the caregiver using the device who has the major impact on outcome. Several monitors reflecting different, but related, aspects of patient physiology often are used concurrently, and often is difficult to identify the most important monitor in a given situation. Furthermore, an experienced, watchful clinician can often respond appropriately to a critical situation without use of complicated monitors. This further confuses the objective analysis of the impact of specific monitors on patient care. Besides aiding the caregiver in deciding to initiate active interventions, monitors reduce caregivers' anxiety by confirming that the functions being monitored are proceeding appropriately. That allows attention to be directed to other areas or other patients. Monitors are extensions of the caregiver's senses. More than one variable can be watched simultaneously. In a busy ICU, unlike the usual OR, one caregiver often manages two or more patients. Monitors help accomplish that task efficiently. Table 1 lists some of the many purposes for using monitors. The reduction in uncertainty provided by monitoring has affected the frequency of medical malpractice actions. The widespread use of Figure 2. Alarms are a special case of monitoring in which an action may take place before a specific diagnosis is made. 883 TABLE 1 -- PURPOSES OF MONITORING IN INTENSIVE CARE UNIT PATIENTS 1. Reduce uncertainty a. Reduce caregiver anxiety b. Reduce medico-legal risk c. Reduce unnecessary treatments d. Allow attention to be focused elsewhere 2. Identify the need for additional therapy a. Identify and modify undesirable trends b. Identify need for additional diagnostic studies 3. Avoid lethal outcome a. Initiate action without diagnosis b. "Extremes" monitoring c. Alarm functions 4. Guide ongoing therapy a. Titrate therapy b. Discontinue therapy as soon as appropriate 5. Direct the use of intermittent diagnostic studies a. Confirm suspected diagnosis b. Identify false-positive findings c. Reduce additional intermittent tests respiratory monitoring (pulse oximetry and capnography) during surgery and anesthesia has resulted in fewer lawsuits for poor outcome caused by inadequate ventilation and hypoxemia. Lower malpractice insurance rates have been awarded to anesthesiologists routinely using those techniques. [6] [44] Many believe it is not that the number or kind of adverse outcomes from anesthesia has changed greatly because of devices, [22] [24] but their use is strong defense against undetected hypoxia being the cause of an adverse outcome. [23] [41] Anesthesiologists believe that monitoring with pulse oximetry is useful even though no study has shown an improved patient outcome attributable to its use. [34] [35] The clinical detection of hypoxemia (cyanosis) is difficult and inexact. Because irreversible harm from hypoxia occurs rapidly and laboratory evaluation of arterial oxygenation is invasive, delayed, and expensive, oximetry, with its many faults, has been accepted as an advance in monitoring for hypoxia by those practicing in the OR environment. [11] Pulse oximetry's appropriate place in the ICU has not been established, but it is widely used. MONITORING'S EFFECTS ON COST OF CARE The aforementioned purposes for monitoring parameters could improve the quality of ICU care. Some of them may also reduce costs. Titration of expensive drugs to minimum effective levels and discontinuation of unnecessary treatments as early as possible generate obvious cost savings. Avoiding organ system complications such as renal failure 884 by minimizing toxic drug effects would save money and improve outcome. Monitoring's effects on costs are listed in Table 2 . Some monitor use may result in increased costs. Besides the cost of the monitor itself, monitoring may lead to further testing to confirm specific diagnoses. Those tests add costs. Invasive monitors involve patient risks. Treatment costs of complications caused by monitors must be assessed when calculating costs of monitoring. Risks of monitors are related to the user's technical skills and experience. [20] There are several other problems with the collection and interpretation of physiologic data. The accuracy of the measurement is the first concern. Vascular waveforms undergo various alterations in traveling through the patient's vascular tree and the monitoring systems. The problems with damping and resonance are well known. The need to maintain a constant zero reference point and internal or external calibration is understood by most anesthesiologists. Most problems with inaccurate data acquisition relate to those areas. Proper selection and use of the electronic or physical display device are another source of problems. When different monitoring equipment is in use in the OR and ICU, the infrequent visitor may experience difficulty in obtaining the desired display or piece of data. In a critical situation, that may result in fatal delay. This concern leads to the recommendation that equipment and procedures be standardized between locations. In addition, as part of a care team, the occasional visitor will need to depend upon and trust other caregivers to provide technical help. The ICU team, unlike the OR team, is made up of a large number of "interchangeable parts" that must provide a similar level of care and expertise around the clock. ICU TABLE 2 -- THE EFFECTS OF MONITORING ON COSTS AND BENEFITS OF INTENSIVE CARE UNIT CARE Direct costs of monitoring Capital Labor Materials Indirect costs and savings Tests added Tests avoided Treatment costs added Treatment costs avoided Bedside-caregiver impact Time lost to maintain monitor Attention lost to false alarms Time for additional tasks (telephone calls, time to perform additional tests) Tasks reduced Outcome benefits Decrease in morbidity Improved safety Possibility other patients may receive more attention Fewer caregivers needed Side effects and risks specific to device 885 care is much more of a team effort because of the need for constant caregiver presence over a period of days. The usefulness of physiologic data is enhanced by following a trend or change after an intervention. Unlike many specialists, anesthesiologists rarely need a precise diagnosis to proceed with treatment. We titrate depth of anesthesia by following changes in multiple physical signs and physiologic variables. We don't even know what anesthesia actually is, yet we empirically, successfully anesthetize patients daily. That empiric approach is also important in critical care. When a cardiologist suggests "keeping the wedge at 10" he is really saying that the preload should be on the low side of normal. That will reduce myocardial oxygen demand but may compromise stroke volume. To know what the actual wedge pressure number really means requires a fluid challenge to determine the compliance or dose-response curve of the heart (Starling curve). A wedge pressure of 10 mm Hg could mean hypovolemia, euvolemia, or even hypervolemia; only the response to fluid can determine which is the case. Once the significance of a specific pressure number is determined, it may change over time. Measurements of response to repeated infusions are often needed to assess the cardiovascular system. Another important data analysis skill is the ability to evaluate several data sources. If the wedge pressure recording is elevated but the neck veins are flat and the chest examination does not detect rales, the determination that the patient is in pulmonary edema and needs additional diuretic agents is in doubt. Weighing multiple data sources, often with conflicting information, requires taking action despite diagnostic uncertainty. LABORATORY DATA Anesthesiologists generally use a limited number of laboratory examinations that are rapidly available in the operating suite. In recent years, requests for a large number of routine preoperative screening tests have been sharply curtailed. They contribute little to care but increase cost. Symptom- or condition-directed testing has been the most costeffective approach. The ICU is different in several important ways. More tests can be obtained but many take a longer time to perform. Specific diagnoses are sought over that longer period of time. Standard and repeated laboratory test ordering is easy do in an ICU. The clinician often has simply to enter the order and someone else will collect the sample, send it off to the laboratory, and record the result. Standing, repeated laboratory orders are easy to create. With indwelling lines, there is little patient discomfort and the tendency is to "reduce uncertainty" by doing another test, even though the result will not change therapy. Too many laboratory tests are performed routinely on ICU patients, which results in the need for additional blood transfusions, the chance 886 of an erroneous result, and inappropriate care decisions. Optimum laboratory use can be achieved by the use of explicit clinical indicators based on the patient's disease process and therapeutic plans. Routine laboratory evaluations for monitoring should be used infrequently. Civetta and Hudson-Civetta [7] and others identified excessive test ordering as an ICU issue; 61% of all laboratory charges were generated during the ICU portion of the patients' stay whereas only 15% of the total stay was in the ICU. They were able to reduce laboratory use by 45% by altering physician test ordering behavior through education, removal of standing orders, development of structured decision trees for common clinical problems, raising acceptance of pulse oximetry, and decreasing "routines" and arbitrary approaches to care. We introduced an arterial blood gas sampling protocol that reduced the number of blood gas samples from 7.5 to 2.5 per patient per day. [2] [4] Making routine blood sampling more difficult has been suggested as a way to reduce unnecessary laboratory use. The presence of an arterial line correlates with an increased frequency of sampling. [33] This approach is draconian and subjects patients to painful procedures. Better physician and nurse education, patient care algorithms, and guidelines can achieve more rational use of laboratory analyses. Point-of-care testing is becoming more common in the OR and ICU. Modular, reliable, low-maintenance laboratory testing equipment is available for dedicated use in the clinical environment. The touted advantage is that the time between sample acquisition and analysis is reduced markedly and clinical decisions are hastened. Patient duration of stay and laboratory personnel costs may be reduced. The downside is that additional testing probably will be performed because of the convenience of the equipment; the equipment is expensive; and the quality of the results is not validated by a professional laboratory specialist. The cost-benefit analysis of this new approach to ICU testing remains to be performed. ROUTINE CHEST RADIOGRAPHY Is a daily routine chest radiograph justifiable in all critically ill patients? How many unexpected changes will be found? Several studies have attempted to address those questions. Brunel and colleagues [5] compared the ability of clinical examination versus radiographs to correctly identify endotracheal tube position in 219 critically ill adult patients. Fourteen percent required repositioning after reviewing the radiograph despite a normal detailed physical examination; 5% of the intubations resulted in a right mainstem location. The authors concluded that chest radiography was required to confirm endotracheal tube location, especially after an emergency intubation. In pediatric patients, Hauser et al [19] found an even higher percentage of abnormal endotracheal tube location. In reviewing 1003 chest films in a surgical ICU, Fong et al [13] found significant abnormalities in 17% of 887 films obtained with no clinical indication (routine), 26% of which were done for verification of device location, and in 30% of cases in which there was a specific clinical concern. The radiographic findings resulted in many interventions and suggest that chest radiographs are a useful adjunct to the clinical examination. The films in stable patients without invasive devices rarely led to a change in therapy, so "routine" films can be avoided safely in this group. Similar results have been shown in medical ICU (MICU) patients. Greenbaum and Marschall [17] determined the value of 200 daily, morning radiographs in the MICU. Although 37% were technically suboptimal or delivered too late for morning rounds, 43% of the others demonstrated significant, unexpected changes. As a result, the authors [17] recommend continuing the current practice of obtaining at least daily radiographs in the critically ill, and improving systems to allow caregivers access to the films in a more timely manner. It is reasonable to obtain and examine a daily chest radiograph in all patients in the ICU who are on mechanical ventilation, have a central vascular catheter, or are being actively treated for cardiopulmonary disease. Immediate films should be obtained after intubation, line placement, or following significant clinical changes. If a patient has had a film for one of those indications within 24 hours and is stable, then no routine daily film is obtained until the following day. At least half the films can be expected to demonstrate significant findings and about a third, to result in alteration of care. All films must be examined by the clinician caring for the patient. PATIENT ACUITY AND QUALITY ASSESSMENT Anesthesiologists are familiar with patient preoperative risk assessment. The American Society of Anesthesiologist's (ASA) physical status assessment score, with risk classes 1 through 5, is universally used to stratify patients' chances for anesthetic complications. Similar approaches are used to assess the risk of groups of patients admitted to the ICU. Such predictors of outcome can be used to evaluate treatment differences (research), identify outcome outliners, or compare a unit's effectiveness to an internal or external standard (quality measure). Several acuity-adjusted outcome systems have been developed and validated for predicting mortality of ICU patients. One of the best known and most widely used ICU mortality predictive systems is the Acute Physiology and Chronic Health Evaluation (APACHE) scoring system. The APACHE II score is based on the patient's age, presence of chronic disease, the patient's source of referral, and a weighted score based on the worst deviation from normal of 17 physiologic measures during the first 24 hours in the ICU. [26] The system has been validated in many different ICUs and among different countries. It predicts about 90% of the outcome (alive or dead at hospital discharge) of groups of critically ill patients. Differences between predicted and actual outcome in an individual ICU can be used as a measure of quality or potential quality 888 problems relative to the "average" ICU outcome represented in the original APACHE II data set. The predictions are based on data that are more than 15 years old. A newer version of the system, APACHE III, is a commercial product with a larger set of diagnosis-specific outcome predictions with a slightly different physiologic data set. [28] Outcomes can be compared between similar institutions, units within the same region, or with the entire database. Periodic updating and calibrating with current data makes the comparisons more useful over time than the original APACHE II system. Similar to APACHE II, slightly more than 90% of the patient's outcome is determined by the status of the patient on ICU admission during the first 24 hours of treatment. A significant improvement in the APACHE III system is the daily prediction of the probability of death in each individual patient, based on algorithms relating to expected physiologic improvements over time and development of organ system failures. Patients who have less than a 10% chance of needing ICU resources are also identified with the APACHE III system. [29] Those patients are only being monitored and can often be cared for in a less intensive (and expensive) hospital location, with minimal risk of a worsened outcome. That is an important tool for managing critical care resources. Other models predicting ICU patient mortality include the Mortality Prediction Model, [32] the Simplified Acute Physiology Score, [31] the Trauma Score and the Injury Severity Scale [3] the Pediatric Risk of Mortality system, [36] and Project Impact, a growing ICU database initiated by the Society of Critical Care Medicine. These systems can also be used to stratify patients according to risk of death and, when applied across units, identify quality concerns. Other quality measures should be collected in all ICUs. They include monitoring the frequency of complications of critical care treatment. The incidence of unplanned patient extubation, invasive line removal, pneumothorax during central line insertion, cardiac arrest, incorrect drug or drug dosage, unexpected return to the operating room, nosocomial infection, need for reintubation after elective extubation, pressure ulcer formation, and death or return to the ICU after discharge have been used to identify quality issues in the ICU. A recent change in the accreditation process is the requirement that physician-specific quality information be used in issuing and renewing credentials. Patient outcome information, including mortality and complications, can be used to meet those requirements. It is essential that case-mix-severity adjustment be included to improve the accuracy and validity of the measures. Scoring systems help provide the calibration. ICUs with better-than-predicted acuity-adjusted outcomes have been identified. The data suggest there are organizational and care delivery methods that may contribute to improved outcome. From the original APACHE study of 13 ICUs, the best units (those that had better-than-predicted outcomes) had a patient-centered culture, strong medical and nursing leadership, effective communication and coordination, and 889 an open, collaborative approach to solving problems and resolving conflict. [27] In a study of pediatric ICUs, the presence of a certified intensivist as unit director and a senior physician decision maker in the unit correlated with the best patient outcome. [36] Other studies have confirmed the contribution of an intensivist as unit medical director to improved outcome. The complexity and differences in ICU organization, missions, resources, and patient populations make it difficult to state generalities relating to different management strategies. The best ICUs are concerned about the quality of patient care delivered, attempt to measure quality, and change operations when opportunities to improve are identified. Patients undergoing surgical procedures experience a lower acuity-adjusted mortality than medical patients admitted to an ICU with similar physiologic derangements. That is because of the acute, reversible physiologic abnormalities induced by anesthesia and surgery. Surgical patients experience more pain in the ICU than medical patients and are often inadequately treated with analgesics. The advent of novel pain relief strategies (i.e., epidural analgesia, patient-controlled analgesia) has positively impacted critically ill surgical patients and probably has reduced perioperative complications and mortality. [43] Patients are admitted to an ICU for active treatment (such as mechanical ventilation, vasoactive drug infusions, or airway protection) or for "monitoring." Patients being monitored have a low frequency (generally < 10% chance) of needing active treatment and experience a relatively low mortality--usually less than 5%. Between 20% and 40% of ICU admissions to average surgical ICUs are for monitoring. The amount of active treatment a patient is receiving can be quantitated in several ways. The Therapeutic Intervention Scoring System (TISS) is a commonly used method that reflects the quantity of care being received and correlates well with ICU costs. [25] TISS points do not correlate with severity of illness because they are determined by local physician and nursing treatment practices. The relative cost of ICU treatment can be estimated from the TISS points when personnel costs are attached to the coded procedures. The updated TISS point system is shown in Table 3 . Any unit manager interested in identifying and controlling costs will employ some system to calculate expenses gauged against severity of illness. CRITICAL CARE RESEARCH Many of the widely accepted treatment approaches used in the critically ill have never been subjected to critical, scientific proof of effectiveness. [12] The quality of information published about critical care treatments varies. There are few randomized, prospective, blinded, controlled trials in the literature. Most useful information comes from other investigative techniques, including cohort studies with historic or contemporaneous controls, case-control studies, and case series. Often, information from several studies is combined in a meta-analysis. Much of 890 TABLE 3 -- THE COMPONENTS OF THE THERAPEUTIC INTERVENTION SCORING SYSTEM (The TISS Score is the Sum of All Points) Modified from Keene AR, Cullen DJ: Therapeutic intervention scoring system; update 1983. Crit Care Med 11:2, 1983; with permission. Four-point interventions Cardiac arrest or countershock within 48 hours Controlled mechanical ventilation Muscle relaxants Balloon tamponade of variceal bleeding Arterial infusion Pulmonary artery catheter Cardiac pacing Peritoneal or hemodialysis in an unstable patient Induced hypothermia Pressurized blood transfusion Military anti-shock trousers Intracranial pressure monitoring Platelet transfusion Intra-aortic balloon pump Emergency operation in past 24 hours Gastric lavage for gastrointestinal bleeding Emergency endoscopy or bronchoscopy More than one vasoactive drug infusion Three-point interventions Central hyperalimentation Pacemaker on stand-by Chest tubes Intermittent mandatory ventilation Continuous positive airway pressure Potassium bolus Intubation Nasotracheal suctioning Complex metabolic balance Lab studies greater than four per shift Blood products greater than five per day Multiple (not scheduled) boli of drugs Single vasoactive drug infusion Arrhythmia drug infusion Cardioversion Hypothermia blanket Arterial line Digitalization within 48 hours Active diuresis for fluid overload or cerebral edema Active treatment for metabolic alkalosis Active treatment for metabolic acidosis Emergency thora-, para-, or pericardiocentesis Active anticoagulation initiated in past 48 hours Phlebotomy for volume overload Administration of more than two antibiotic agents Initial treatment of seizures or metabolic encephalopathy Complicated orthopedic traction Two-point interventions Central venous pressure monitoring Two peripheral intravenous catheters Hemodialysis-stable patient Tracheostomy in previous 48 hours Spontaneous ventilation through an artificial airway Gastrointestinal tube feedings Replacement of excess fluid loss Parenteral chemotherapy Hourly neurologic checks Multiple dressing changes Pitressin infusion One-point interventions Electrocardiographic monitoring Hourly vital signs Single intravenous catheter Chronic anticoagulation therapy Intake and output recording Emergency blood tests Intermittent scheduled medications Routine dressing changes Standard orthopedic traction Tracheostomy care Decubitus ulcer Urinary catheter Supplemental oxygen by mask or cannula Chest physiotherapy Extensive wound care Gastrointestinal drainage Peripheral hyperalimentation 891 what is done in critical care depends on consensus development conferences in which acknowledged experts share opinions and develop a document that is reduced to the common elements this can be agreed upon. There has been a trend recently to qualify and quantitate the information supporting consensus document statements. This is helpful in separating belief from fact and identifying areas in which additional research is needed. Unlike the case in the OR, where a single clinician decides what is to be done and then does it, the ICU consists of many caregivers, each of whom has his or her role in the delivery of care. As many as 50 different individuals may see an ICU patient during a single day. Each individual brings biases and past experiences to the care process. The ICU care plan often is the result of negotiation. To change from the "routine" is difficult and involves risks. If a physician wants to give a new drug or an old drug through a new route, the system will resist the change. The education and negotiation begin at the bedside while the 892 physician is presenting his plan. After convincing those present that it is a reasonable idea, the plan may fail later, at change of shift, because new caregivers have not heard the arguments supporting the departure from standard procedure or may not understand exactly what was to be done. The system tends to return care to the "usual." True advances in critical care practice are equally difficult to establish. Information relating to critical illness is published in more than 60 weekly and monthly journals. It is impossible to remain current in all areas, and what works in a controlled environment may be worthless in the real world of critical care. Clinical utility is the ability of a device or treatment to achieve its ascribed goals under controlled circumstances. Monitoring devices, for example, have been evaluated for clinical utility. Evaluation of a monitor includes demonstration of accuracy and correlation with other known effective monitors. It also includes demonstrating that the monitor contributes to a desired outcome with a known disease process in prospective, controlled studies performed in carefully selected clinical situations. Some physiologic monitors have been tested in that way and regarding accuracy, predictability, and correlation with expected outcome. Clinical effectiveness, on the other hand, is the ability of the device or treatment to achieve the same desired results under less rigorously controlled use. [21] In general, that level of proof has not been demonstrated with any monitor and with few therapies in the ICU. For monitoring devices and equipment, a middle ground may be clinical usefulness. This concept reflects the balance among accuracy, ease of use, and production of meaningful information. A device is used only if (1) its use is mandated by policy, (2) it is believed to be "worth the trouble" by the user (if given a choice), or (3) it is both mandated and useful. Cost effectiveness of a treatment or device implies that, in addition to being clinically effective (or at least useful), it costs less or incurs less risk than other accepted treatments. New technology and treatments should not be introduced unless they are (1) less costly and at least as effective as the current standard, (2) more costly but more effective and the added benefit is worth the added cost, or (3) less effective and less costly but the benefit of standard treatment is not worth the added cost. [8] [15] [30] Changes in CCM practice will occur in the coming years. Decisions regarding treatment will be modulated by cost considerations. The financial survival of the health care institution may depend upon it. Using data and analyses or cost-effectiveness, providing appropriate care at lower cost is possible. As previously mentioned, standardized treatment approaches under the control of guidelines or algorithms offer promise of quality and cost improvement in the ICU. Protocols for weaning patients from mechanical ventilation are frequently used in critical care units. Most of them were designed to decrease hours of mechanical ventilation and establish acceptable methods of withdrawal of support. They are often based on the techniques 893 preferred by the attending physician or the unit's physician manager, but may be developed in conjunction with the respiratory therapy and nursing staff. They are specific to the unit population and often reflect unit organization and coverage patterns. Extubation after a certain hour (i.e., midnight) may be forbidden, for instance, because of unavailability of personnel skilled in airway management at night. Whether weaning is performed with t-piece trials or reduction in intermittent mandatory ventilation rate or pressure support level, it should be performed in a consistent, gradual, step-wise fashion that can be described by a flow chart or algorithm. A unit-specific, diagnosis-specific plan can be developed and consensus developed to allow weaning to occur predictably. Allowing independent assessments and decisions (within the framework of the algorithm) by nonphysician caregivers (nurses and respiratory therapists) improves consistency and efficiency. The amount of latitude given to therapists and nurses in weaning patients depends upon their skill level, consistency of coverage, and the trust they have developed with the physician staff. Patient-driven protocols (PDPs) for weaning patients from mechanical ventilation may be more efficient than traditional physician-therapist-decided weaning. Wood and others [42] evaluated the effects of initiating a PDP for IMV weaning in a surgical ICU. They compared the incidence of respiratory problems, duration of mechanical ventilation, and duration of weaning when cardiac surgery patients were changed from weaning by physicians to weaning by PDP. They found no change in complications and a slight decrease in total duration of mechanical ventilation with PDP weaning (18.6 versus 16.8 hours). There was an insignificant decrease in weaning time, from 3 hours to 2.2 hours. The PDP they developed was very restrictive, allowing a maximum decrease of six breaths per hour in IMV rate and mandating arterial blood gas analysis after every ventilator change. After safety was demonstrated in stable cardiac patients, physicians were permitted to order PDP weaning for other patients. Over an approximately 7-month period, the percentage of patients weaned by PDP rose progressively to 90%. Entrance criteria were liberalized operationally (but not changed formally) and many less stable patients were weaned and stable patients were entered into weaning earlier. The statistically significant shortening of total time of mechanical ventilation persisted throughout the study periods. Interestingly, even physician-weaned patients had a shortened duration of mechanical ventilation during the later part of the study compared with the control period. The use of a protocol by therapists seemed to increase the efficiency and consistency of weaning by physicians when the PDP was not in use. Although statistically significant, the changes observed in duration of mechanical ventilation (2.1 hours) probably had little economic impact. The significance of the introduction of PDP weaning was the increased confidence that physicians developed in the respiratory therapists' abilities to assess patients and make independent management decisions. Therapists' suggestions become more consistent among 894 practitioners. Only 4% of patients failed PDP weaning in the study. The expanded use of nonphysicians in the ICU is likely to continue. Working as part of a multidisciplinary team is a skill practiced daily by anesthesiologists. Comfort with that arrangement is necessary for ICU survival. Changes in payment and control of health care costs will effect changes in management of critical care units. As integration of individual institutions into cooperative care delivery systems becomes necessary, integration within component organizations must also occur. ICUs no longer can be viewed in isolation from the rest of the hospital. Hospitals must see themselves as part of a system in which groups of patients are provided health care. Institutions are combining resources to reduce unnecessary market competition and achieve savings of scale and reduction of redundancy. Home health care, skilled nursing homes, outpatient clinics, and the hospital must achieve integration, focusing on the patient's (or a population of patients') needs rather than marketing an expensive (unnecessary?) service. The patient's disease takes center stage and care must be provided efficiently in the most appropriate area of the system. [16] Prevention and control of hospital admissions are implicit in the financial strategies of managed care plans. The provision of critical care services is a very costly activity for a hospital. Prevention of avoidable ICU admissions can save institutional resources. Because many patients are admitted to an ICU after respiratory deterioration on a hospital floor, improved pulmonary assessment and care outside the ICU should assume a high priority for the ICU manager. Improvements can be achieved by prospectively identifying patients at risk for respiratory failure and intervening with less invasive techniques, possibly preventing the need for mechanical ventilation. For patients needing ICU care, early identification and treatment of respiratory failure should result in a shorter duration of ICU and hospital stay and better survival. By thinking of the continuum of care sites, each therapist can expand his or her role to one of respiratory disease management, the intent being to avoid preventable, higher cost care, and to improve patient outcome through earlier intervention. One high-risk group comprises patients discharged from an ICU. Many are recovering from respiratory failure and may require ICU readmission, which is expensive and carries a high risk of mortality. Franklin and Jackson [14] examined 36 readmissions to a medical ICU and found a mortality rate of 58%, compared with 12% mortality of all medical ICU patients. Rubins and Moskowitz [39] reported a 16% unexpected readmission rate or death on a hospital floor after discharge from a medical ICU. The mortality rate in the patients was 57%. Respiratory problems were responsible for most of the readmissions in their study. Baigelman, Katz, and Geary [1] studied readmissions to any of four ICUs in a community hospital. They found an 11.7% overall readmission rate and believed that as many as 36% of those patients were discharged prematurely. Included in their study were a significant number of patients with acute myocardial infarction, perhaps accounting for the rather low mortality rate (21%) reported in that group of readmitted 895 patients. In a report of readmissions to a surgical ICU, Snow and others [40] found a mortality rate of 26% in a group of 57 patients readmitted, representing 9.4% of the total ICU admissions. We previously identified respiratory deterioration as the most frequent cause resulting in the need for ICU readmission. In our tertiary care hospital, 54% of patients were readmitted to medical and surgical ICUs for respiratory deterioration. [10] Forty-seven percent of the readmitted patients expired before hospital discharge. Following our initial study, we instituted several changes to address respiratory issues on the hospital floors, including establishment of a dedicated floor therapist assessment team, [18] use of respiratory treatment algorithms, [4] and continuous staff education programs, [2] in an attempt to improve respiratory care after ICU discharge. The goals were to continue aggressive respiratory care after ICU discharge, and, hopefully, reduce readmissions for respiratory failure. We recently restudied the issue. [9] Although acute respiratory deterioration remained the most frequent cause for ICU readmission (45%), the mortality of readmitted patients plummeted to 12% overall and 19% for those with a primary respiratory problem resulting in ICU readmission. With active attention on the floors, definitive treatment more frequently was started prior to arrival at the ICU. Providing frequent respiratory monitoring and appropriate care on leaving the ICU, especially to those at high risk, has improved the outcome in patients readmitted. The change in acute care management strategy had no effect on ICU duration of stay or overall ICU readmission rate. The average number of days spent in the ICU on the first admission was 8.3 in the most recent study versus 6.3 in the previous study ( p=0.165, t test). Readmitted patients in the previous study remained out of the ICU 5.9 days, compared with 6.7 days in the recent study period. Prior to instituting the changes, 4.7% of ICU discharges were readmitted; after the changes, 4.7%. Attention to the potential for respiratory failure in this high-risk population and provision of respiratory care across several care sites have improved quality (reduced mortality) and (probably) reduced costs. The development of step-down care units has had similar effects in other institutions. For cost-effective care in a competitive marketplace, the continuum of care sites must be integrated and patients provided care in a seemless fashion. The traditional borders of the ICU must be lowered and patients' needs met in what ever environment is most appropriate. That requires considerable flexibility on the part of caregivers and managers. Many sources of data are available to the individual working in an ICU. Understanding the meaning, sorting, and weighting of each element is necessary for appropriate decision making in the ICU. Information from laboratory studies, physiologic monitoring, and the patient's physical examination must be integrated to make a clinical decision on care. Information from population studies, comparison with other units, and quality data can improve processes and the unit's functioning in general. The cost of care is everyone's concern and making cost-effective 896 changes is a new idea for many physicians. Seeing oneself as contributing to a team effort rather than controlling patient care is the attitude necessary to the future development of health care delivery. By understanding the many kinds of data, anesthesiologists can be at the forefront of these developments. References 1. Baigelman W, Katz R, Geary G: Patient readmission to critical care units during the same hospitalization at a community teaching hospital. Intensive Care Medicine 9:253-256, 1983 2. Beasley KE, Darin JM, Durbin CG: The effect of respiratory care department management of a blood gas analyzer on the appropriateness of arterial blood gas utilization. Respiratory Care 37:343-347, 1992 3. Boyd CR, Tolson MA, Copes WS: Evaluating trauma care: The TRISS method. J Trauma 27:370-378, 1987 4. Browning JA, Kaiser DL, Durbin CG Jr: The effect of guidelines on the appropriate use of arterial blood gas analysis in the intensive care unit. Respiratory Care 34:269-276, 1989 5. Brunel W, Coleman DL, Schwartz DE, et al: Assessment of routine chest roentgenograms and the physical examination to confirm endotracheal tube position. Chest 96:1043-1045, 1989 6. Caplan RA, Posner KL, Ward RJ, et al: Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology 72:828-833, 1990 7. Civetta JM, Hudson-Civetta JA: Maintaining quality of care while reducing the charges in the ICU: 10 ways. Ann Surg 202:524-532, 1985 8. Detsky AS, Naglie G: A clinician's guide to cost-effective analysis. Ann Intern Med 113:147-154, 1990 9. Durbin CG, Kirby EA: Frequency of respiratory causes for ICU readmission. Respiratory Care 39:1069, 1994 10. Durbin CG, Kopel RF: A case-control study of patients readmitted to the intensive care unit. Crit Care Med 21:1547-1553, 1993 11. Eichorn JH, Cooper JB, Cullen DJ, et al: Standards for patient monitoring during anesthesia at Harvard Medical School. JAMA 256:1017-1020, 1986 12. Fineberg HV, Hiatt HH: Evaluation of medical practices: The case for technology assessment. N Engl J Med 301:1086-1091, 1979 13. Fong Y, Whalen GF, Hariri RJ, et al: Utility of routine chest radiographs in the surgical intensive care unit. A prospective study. Arch Surg 130:764-768, 1995 14. Franklin C, Jackson D: Discharge decision-making in a medical ICU: Characteristics of unexpected readmissions. Crit Care Med 11:61-66, 1983 15. Fuchs VR, Garber AM: The new technology assessment. N Engl J Med 323:673-677, 1990 16. Girotti MJ: Reengineering trauma care; the challenge of the nineties. J Trauma 40:855-859, 1996 17. Greenbaum DM, Marschall KE: The value of routine daily chest x-rays in intubated patients in the medical intensive care unit. Crit Care Med 10:29-30, 1982 18. Hart SK, Dubbs W, Gil A, et al: The effects of therapist evaluation of orders and interaction with physicians on the appropriateness of respiratory care. Respiratory Care 34:185-190, 1989 19. Hauser GJ, Pollack MM, Sivit CJ, et al: Routine chest radiographs in pediatric intensive care: A prospective study. Pediatrics 83:465-470, 1989 20. Iberti TJ, Fischer EP, Leibowitz AB, et al: Physicians' knowledge of the pulmonary artery catheter. JAMA 264:2928-2932, 1990 21. Inman KJ, Sibbald WJ, Rutledge FS, et al: Clinical utility and cost-effectiveness of an air suspension bed in the prevention of pressure ulcers. JAMA 269:1139-1143, 1993 897 22. Keats AS: Anesthesia mortality in perspective. Anesth Analg 71:113-119, 1990 23. Keats AS: The closed claims study. Anesthesiology 73:199-201, 1990 24. Keenan RL, Boyan CP: Decreasing frequency of anesthetic cardiac arrest. J Clin Anesth 3:354-357, 1991 25. Keene AR, Cullen DJ: Therapeutic intervention scoring system; update 1983. Crit Care Med 11:1-3, 1983 26. Knaus WA, Draper EA, Wagner DP, et al: APACHE II: A severity of disease classification system. Crit Care Med 13:818-829, 1985 27. Knaus WA, Draper EA, Wagner DP, et al: Evaluation of outcome of critical care. Ann Intern Med 104:110-118, 1986 28. Knaus WA, Wagner DP, Draper EA, et al: The APACHE III prognostic system: Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100:1619-1936, 1991 29. Knaus WA, Wagner DP, Draper EA: Identification of low-risk monitor admissions to medical-surgical ICUs. Chest 92:423-428, 1987 30. Laupacis A, Feeney D, Detsky AS, et al: How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Can Med Assoc J 146:473-481, 1992 31. Le Gal JR, Loirat P, Alperovitch A, et al: A simplified acute physiology score for ICU patients. Crit Care Med 12:975-977, 1984 32. Lemeshow S, Teres D, Avrunin SJ, et al: A methods for predicting survival and mortality of ICU patients using objectively derived weights. Crit Care Med 13:519-525, 1985 33. Low L, Harrington GR, Stoltzfus DP: The effect of arterial lines on blood-drawing practices and costs in intensive care units. Chest 108:216-219, 1995 34. Moller JT, Penderson T, Rasmussen LS, et al: Randomized evaluation of pulse oximetry in 20,802 patients: I. Design, demography, pulse oximetry failure rate, and overall complication rate. Anesthesiology 78:436-444, 1993 35. Moller JT, Penderson T, Rasmussen LS, et al: Randomized evaluation of pulse oximetry in 20,802 patients: II. Perioperative events and postoperative complications. Anesthesiology 78:445-453, 1993 36. Pollack MM, Cuerdon TC, Getson PR: Pediatric intensive care units: Results of a national survey. Crit Care Med 21:607-614, 1993 37. Pollack MM, Ruttimann UE, Getson PR, et al: Pediatric risk of mortality (PRISM) score. Crit Care Med 16:1110-1116, 1988 38. Robin ED: Death by flow-directed pulmonary artery catheter? Chest 92:727-728, 1987 39. Rubins HB, Moskowitz MA: Discharge decision-making in a medical intensive care unit: Identifying patients at high risk of unexplained death or unit readmission. Am J Med 84:863-869, 1988 40. Snow N, Bergin KT, Horrigan TP: Readmission of patients to the surgical intensive care unit: Patient profiles and possibilities of prevention. Crit Care Med 13:961-964, 1985 41. Tinker JH, Dull DL, Caplan RA, et al: Role of monitoring devices in prevention of anesthetic mishaps: A closed claims analysis. Anesthesiology 71:541-546, 1989 42. Wood G, MacLeod B, Moffat S: Weaning from mechanical ventilation: Physician-directed vs a respiratory-therapist directed protocol. Respiratory Care 40:219-224, 1995 43. Yeager MP, Glass DD, Neff RK, et al: Epidural anesthesia and analgesia in high-risk surgical patients. Anesthesiology 66:729-736, 1987 44. Zeitlin GL: Possible decrease in mortality associated with anaesthesia. A comparison of two time periods in Massachusetts, USA. Closed Claims Study Committee. Anaesthesia 44:432-433, 1989 898 Guest Editor's Commentary Data in the Intensive Care Unit Philip D. Lumb MB, BS Guest Editor "The best ICUs are concerned about the quality of patient care delivered, attempt to measure quality, and change operations when opportunities to improve are identified." Durbin introduces two key driving forces that forced the logical development of critical care units: "Patients required rapid, specific interventions to prevent physiologic deterioration or death, and hospitals needed to effectively and efficiently provide necessary levels of service." That introduction of both patient- and business-driven requirements provides a framework on which discussion of the following topics is placed: physiologic data and monitoring, laboratory data, outcomes information and prediction systems, critical care research, and cost/quality information. He prefaces his remarks by underscoring the characteristics that make anesthesiologists influential practitioners in the difficult clinical environment of CCM: "(1) the ability to lead a team of professionals inconspicuously and (2) the ability to analyze massive amounts of data efficiently and act appropriately and rapidly on sometimes conflicting results." The concepts of predictive analysis and cost-effective resource management are added to this provocative discussion of the developing role of the anesthesiologist intensivist. Indeed, it is in that light that the article must be analyzed. Durbin has taken a routine topic and promoted it to become the platform from which an important new discussion of critical care practitioner responsibility and prerogative must be initiated. That topic is suggested in the statements pertaining to clinical utility and clinical effectiveness. It is highlighted in the discussion regarding decreasing the cost of care with dependent protocols developed between physician and skilled ancillary health care providers and the value of appropriate floor care and triage in decreasing complications, ICU readmission rate, and overall patient mortality. Durbin provides fresh insight into the clinician's responsibility to collect and analyze data correctly; more importantly, he highlights the futility of monitoring without appropriate, indicated intervention. The logic of Durbin's article is inescapable, yet the current practice standard in many ICUs and operating rooms ignores the aforementioned principles and indicates to an observer that data collection is less patient-care driven and more regulatory responsive than appropriate for today's difficult clinical practice environments. The reasons why that is the case are multiple and complex, not the least important of which have to do with tradition and the confusion of roles and prerogatives in the ICU itself. In some instances, data are available, but appropriate action is 899 either impossible or delayed in the face of regulations that proscribe intervention by some practitioners or threaten the therapeutic imperative of others. In addition, and perhaps equally important, the manner in which data are acquired, displayed, and, perhaps therefore, interpreted has not changed significantly in the past 25 years. The automated physiologic profile described by DelGuercio in the 1970s provided the same data in a more useable format than is available in many ICUs today. A completed profile both provided insight into the patient's condition and reminded the clinician of the physiologic principles underlying suggested therapeutic interventions. It was an advocate of early nutritional support, a strangely simple initiative that continues to lack vigorous supporters, and it provided a graphic, temporal snapshot of the patient's condition. That feature permitted rapid evaluation of therapeutic interventions, and rapid therapeutic titration was possible across a range of interventions. Durbin's contention that the anesthesiologist is positioned to work in this environment is well founded. A similar condition has existed in the operating room, in which much of the effort in automated data collection has been to reproduce the anesthetic record electronically rather than to provide the clinician with a more appropriate data set upon which to base therapeutic intervention. The analogous situation does not exist in the profession to which anesthesiology is often compared--piloting an aircraft. There is no doubt that aircraft pilots consider the job of landing an expensive piece of hardware on an unstable platform in all weathers to be a challenge but one for which they are well trained and electronically supported. Indeed, the final approach can be subjected to physical and mathematical interpretation and simulation, and a yardstick has been developed against which the pilot can judge the effectiveness of the approach--the ball. During final approach and landing, the pilot is required to keep alignment of a lighted ball in a heads-up display graticule. The task is not easy, but the payoff is significant. Correct alignment is possible only if numerous characteristics about the plane's attitude, altitude, glide path, speed, angle of descent, and others are appropriate for the specific conditions existing on the flight deck at the time of the expected landing. Responsive to different aircraft and in all weather conditions, the technology has advanced to the point of making it easier for the pilot to concentrate on an output that integrates numerous, complex data sets and translates their interactions into an understandable, useable, and actionable signal. Indeed, with the complexity and speed of modern aircraft, it is unlikely that the carrier-based support wings could have been deployed effectively in the absence of advanced, integrated, and functional technology. Unfortunately, the same care in data processing, integration, analysis, and display has not been a priority in either the operating room or the ICU. Technology's outputs have remained vendor-specific until recently, and integrating different signals has negative financial implications for companies producing proprietary hardware with individual, single-channel printers. One has only to look at the back of an ICU flowsheet to see the individual traces taped to the 900 back of the cart, indicating either a new calibration or an observed dysrhythmia. That has worked reasonably on an individual basis, but recovery of the information for comprehensive risk management and quality analysis is virtually impossible, promoting the myth that we can't expect the outcome of biologic dysfunction to be as predictable as that of a physical object with defined characteristics and a known destination. The argument is persuasive and may be valid; the fact is that we cannot articulate an argument either for or against because the integrated, analyzed, and appropriately displayed data are lacking despite collection of their components. Gene Roddenberry recognized the importance of this concept when he provided Star Trek's Enterprise capabilities that we can but admire today; remember the monitors displaying "brain metabolism," "cellular function," and "life force?" Modern technology may be capable of approaching those outputs cost effectively; it will be up to clinicians to demonstrate the need and the willingness to "fly by the ball," a new sensation for many and one that will require empowerment of new providers on the CCM team. Durbin explores these issues more practically and less fancifully than my comments, and his insightful approach to the subject is to be commended. It is likely that his premise regarding the anesthesiologist's important role in this arena can be supported if the activities of more practitioners extend outside the operating room into the perioperative arena, to include that of the ICU and other high-dependency units. The imperatives to succeed are great; decreased resources, increased clinical demands from increasingly complex diseases and procedures, and a commitment to excellent patient care require a new and more effective clinical armamentarium. Improving data collection, analysis, and display in the ICU is a vitally important requirement in the future paradigm and one in which anesthesiologists provide the human template for the desired electronic outcome.