Guidance for Home Intravenous Management of Uncomplicated l
advertisement

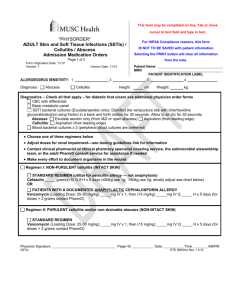
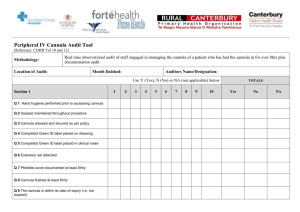
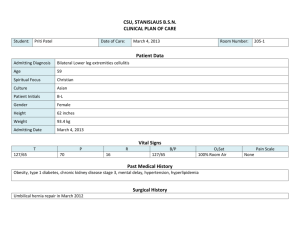
Guidance for Home Intravenous Management of Uncomplicated lower limb cellulitis Introduction: Cellulitis is one of the common problems in patients attending A&E and MAU. Until recently those patients requiring IV antibiotics needed hospital admission. However in the past 10 years increasingly these patients are being treated in the community. A number of studies suggest that IV treatment at home is a safe alternative to in-hospital cellulitis treatment. The benefits of OPAT include admission avoidance and reduced length of stay in hospital, with resulting increases in inpatient capacity, significant cost savings, reduction in health care associated infection and improved patient choice and satisfaction Eligibility Criteria for out patient IV treatment: The patient must fulfil all criteria to be deemed suitable for outpatient treatment of cellulitis 1. Telephone access 2. Responsible adult or responsible adult at home 3. Clinical diagnosis of Class1or 2 cellulitis 4. Rapid response nurse’s acceptability 5. Over 16 yrs age 6. Consent given Exclusion Criteria: If the patient has any criteria listed below they are not suitable for outpatient IV treatment 1. Hypersensitivity to Teicoplanin 2. Pregnancy, lactating 3. Hepatic and/ or renal disease 4. Neutropenia 5. Facial/ Perineal cellulitis 6. Class 3 & 4 cellulitis 1 7. Likelihood of non-compliance 8. Concurrent uncontrolled infection 9. Intravenous Drug use 10. Advanced dementia Final decision on Inclusion or exclusion of patient from Home IV therapy rest on attending clinician Classification of cellulitis Class 1: Patients have no sign of systemic toxicity, have no uncontrolled co-morbidity and can usually be managed with oral antimicrobials on an outpatient basis. Class 2: Patients are either systemically ill or systemically well but with co-morbidity such as peripheral vascular disease, chronic venous insufficiency or morbid obesity which may complicate or delay resolution of their infection Class 3: Patients may have significant systemic upset such as acute, confusion, tachycardia, tachypnoea, and hypotension or may have unstable co-morbidities that may interfere with a response to therapy or have a limb threatening infection due to vascular compromise. Class 4: Patients have sepsis syndrome or severe life threatening infection such as necrotising fasciitis. 2 PATHWAY Attendance with diagnosis of cellulitis Admit to CDU/AMAC, mark cellulitic area. Insert venflon & take blood for FBC/CRP/ U&E/LFT/glucose Assess for suitability for outpatient administration of antibiotics see criteria . Give information to patient regarding outpatient treatment Complete discharge checklist and file it in the patient notes Administer Antibiotics in accordance with the IV protocol Ensure cellulitic area clearly marked Add patient into AMAC/CDU outpatient antibiotic book Discharge the patient with the D1 form, and information leaflet Fax D1 form to the GP 3 Complete D1 Refer patient to Rapid response and confirm acceptance Ensure venflon secure, insertion date is present and VIP score completed Identify first return pointAMAC/CDU if required and also for repeat blood Individual Responsibilities Initial Hospital ResponsibilitiesDay 1 Community Nurse Responsibility on a Daily Basis 1. Full medical assessment and bloods taken for: FBU, U&E’s LFT’s and swab from open wounds for Culture and Sensitivities. 2. Diagnosis made of Class 1or Class 2 Cellulitis 3. Administer Teicoplanin IV 800mg a) Given by 30 minutes infusion b) Patient should remain on AMAC/CDU for a minimum of 1 hour after the completion of infusion to check for any reaction to antibiotics 4. Complete D1 5. Consultant or senior doctor to review the patient before discharge Liaison with AMAC should take place in the following: If the patient’s condition deteriorates at anytime If the patient is still febrile after 3 days of Teicoplanin treatment If no improvement after 5 days of antibiotic treatment If patient is apyrexial for 48 hrs. and has evidence of definite improvement of cellulitis change to oral Daily Checking of cannula: The cannula site should be checked, and the Visual Infusion Phlebitis Score (VIP) recorded on a daily basis. Other Measures where necessary: Leg elevation Look for ports or entry of infection; toe clefts, heels, sites of trauma Dressings and bandages as required Community Nurse Responsibilities – 2nd, 3rd and 4th day 1. Administer IV Teicoplanin 2. Provide appropriate care according to assessment and care plan 3. The cannula must be checked daily, and should be renewed if there is any evidence of infection/extravasation Community Nurse Responsibilities – 5th Day 1. Administer IV Teicoplanin 2. Provide appropriate care according to assessment and care plan. Cellulitis Improving Change to oral therapy based on culture and sensitivities, or empirical Flucloxacillin 1g QDS for 7 days or longer if necessary 1 No Improvement Refer to AMAC Change antibiotics – discuss with microbiology. SUITABILITY FOR OUTPATIENT ADMINISTRATION OF IV ANTIBIOTICS Diagnosis of cellulitis requiring IV antibiotics? Yes Does the patient have ≥2 signs of systemic sepsis? • Temperature >38 or <36oC • Pulse >90/min • Systolic BP <100 • RR >20 No Does the patient have >1 of the following? • WBC >14 or <4 • Severe lymphangitis, blistering or large affected area • Immunosuppression • Pregnant • Poorly controlled diabetes • Peripheral vascular disease Yes Hospital admission required See also other exclusion criteria Final decision rests on the clinician No Patient suitable for outpatient IV administration protocol 2 Yes Hospital admission required ANTIBIOTIC CHOICES FOR THE OUTPATIENT TREATMENT OF CELLULITIS Day 1 Teicoplanin 800mg (as infusion over 30mins) Or if Teicoplanin allergy* Ceftriaxone 2G (Over 30min infusion) *Ceftriaxone is only to be used if the patient is known to either be allergic or they have had previous significant reaction to Teicoplanin. If there is any concern as to the suitability of a patient, please discuss with a doctor. Day 2 onwards Teicoplanin 400mg OD (2nddose as Infusion for 30 min then bolus 3-5 min) Ceftriaxone 1G (bolus over 3-5mins) OR If a patient is on Ceftriaxone and is failing to improve consider increasing dose to 2G (by 30min infusion) Oral conversion: Once patient is apyrexial for 48 hours and has evidence of definite improvement in the appearance of their cellulitis: Flucloxacillin 1 qds (for minimum 7 days) OR if penicillin allergic Clarithromycin 500mg bd (for minimum 7 days) -7 Dose of teicoplanin in renal impairment 3 CrCl>20 Dose as above for all patients CrCl 10-20 Teicoplanin 800mg o.d (DAY 1) Then 200mg every 24hr CrCl<10 Patient not suitable for outpatient IV antibiotic therapy Date: Patient Sticker CHECK LIST FOR A&E/AMAC PRIOR TO INITIAL DISCHARGE (Please circle as appropriate) Attendance with diagnosis of Cellulitis(Class 1or 2) Yes No Suitable for outpatient cellulitis service Yes No Accepted by Rapid response team Yes No Consent documented in notes Yes No Mark cellulitic area with indelible pen Yes No Photograph of area (if possible) Yes No IV cannula inserted Yes No Bloods Taken (FBC, U&E , ESR or CRP) Yes No Patient given information leaflet Yes No IV cannula secure, flushed with saline and dressed with sterile, semipermeable transparent dressing e.g iv 3000 Yes No Insertion date is present and VIP score in completed Yes No Identifying first return point time AMAC if required Yes No Requirement for bloods identified Yes No D1 complete Yes No Book patient into AMAC /CDU outpatient antibiotic book Yes No TTOs completed Including the following Teicoplanin 400mgx 6vials Yes No Complete discharge checklist below (Please circle as appropriate) D1 faxed to the GP All boxes must be ticked and clear for patient to be entered into the pathway. Completed By: Please print the name of the person completing this check list 4 Date: Patient sticker Barnsley Hospital NHS Foundation Trust Discharge Instructions Discharge instructions for patients with Cellulitis You have been treated on the CDU for the cellulitis The medical team have assessed you and have decided that you are well enough to be treated as an outpatient. You should return or contact the AMAC if: You feel generally unwell / dizzy The redness gets worse You have an episode of uncontrolled shaking You have any problems with your cannula / drip o o o o o There is no needle present but it is important you look after it. Keep your cannula dry and covered with the dressing provided. Ensure it does not become caught in clothing or dislodged. If your cannula does come out apply pressure with a clean dressing. A new cannula will be inserted the next day. Sometimes the cannula site becomes infected. If skin around the cannula becomes red or painful call the number below for advice. If you are concerned in anyway feel free to call on the numbers below Yours Sincerely If you have any problems / concerns please call Barnsley AMAC unit Or Rapid response team 5 01226 431345 07747794698 Date: Patient sticker CELLULITIS PATHWAY: RECORD OF TEICOPLANIN ADMINISTRATION BY RAPID RESPONSE To be administered using aseptic technique and as per trust clinical procedure. PATIENT NAME PATIENT NHS NO: DATE & TIME VIP SCORE 1ST DOSE TO BE 6 PERIPHERAL CANNULA INSERTED REMOVED LINE CLEANED (CHLORHEXIDINE GLUCONATE IN 70% ALCOHOL) GIVEN AS INFUSION PRE & POST DOSE FLUSH (5ml 0.9% saline) ANTIBIOTIC GIVEN DOSE BATCH/EXPIRY SIGNATURE OF NURSE Date: Patient sticker CELLULITIS: DAILY RECORD BY RAPID RESPONSE PATIENT NAME DAY AT HOME DATE & TIME PATIENT NHS NO: EFFECT OF ANTIBIOTICS SYSTEMIC SYMPTOMS IMPROVING IF DETERIORATING; SEEK MEDICAL ADVICE FROM AMAC. NIL NOTED IF GI UPSET/ RASH SEEK MEDICAL ADVICE FROM AMAC. SEVERE REACTION; 999 ADMINISTER ADRENALIN AS PER ANAPHYLAXIS POLICY. MARKED CELLULITIC AREA IMPROVING IF UNCHANGED ON 2 VISITS /REMAINS CELLULITIS CLASS2 OR DETERIORATES SEEK MEDICAL REVIEW. TEMPERATURE OUT PATIENT REVIEW SIGNATURE OF NURSE YES/NO 1 2 CHECK SWAB RESULTS IF 3 TAKEN IN HOSPITAL REPEAT BLOODS 4 5 6 7 ONCE PATIENT IS APYREXIAL FOR 48 HOURS AND HAS DEFINITE IMPROVEMENT IN THE APPEARANCE OF CELLULITIS ,THEN COMMENCE ORAL ANTIBIOTICS. IF NO IMPROVEMENT BY DAY 5 SEEK MEDICAL ADVICE FROM AMAC REGARDING FURTHER TREATMENT. 7 Author: Dr J Rao, Consultant Microbiologist/DIPC Issue Date: November 2014 Review Date: November 2016