Nutfah Male
advertisement

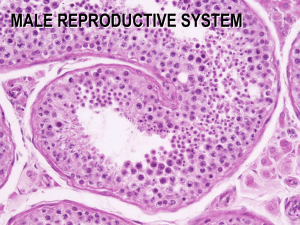
Nutfah • Nutfah is a comprehensive term and includes male and female gametes, zygote, morula, and blastocyst before implantation and part of fluid in their natural environments. • So sperms with seminal fluid, products of ovulation and the state of insan during first 6 to 7 days or 1st week after fertilization in intrauterine life are included in the term Nutfah • • • • • Thus the stages of Nutfah are: Male and female gametes Zygote Morula Blastocyst Male Gametes • • • • • • 1. 2. 3. 4. 5. 6. Spermatogonia Primary spermatocytes Secondary spermatocytes Spermatids Spermatozoa Sperms • • • • structure of a testis can be described as Lobules containing interstitial cells of Leydig Seminiferous tubules embedded in loose CT Lobules containing 10 to 12 seminiferous tubules • Seminiferous tubules lined by stratified cuboidal epithelium • Lobules separated by seminiferous tubules • • • • structure of a testis can be described as Lobules containing interstitial cells of Leydig Seminiferous tubules embedded in loose CT C Lobules containing 10 to 12 seminiferous tubules • Seminiferous tubules lined by stratified cuboidal epithelium • Lobules separated by seminiferous tubules Spermatogenesis • [Gr. Spermato - male seed + Gr. Genesis production] • The formation of male gametes is called spermatogenesis. • The term spermatogenesis refers to the sequence of events by which Spermatogonia are transformed into sperms. • This is the maturation of male gametes in the testes, the primary sex organs of male partner. • The maturation process begins at puberty (about 14 years) and continues until old age. • The process of formation of spermatozoa includes spermatocytogenesis and spermiogenesis. • • • • • • In testis sperms develop from Spermatogonia cells in ductus deferens Sertoli cells of seminiferous tubules Leydig cells of seminiferous tubules Spermatogenic cells Spermatozoa in efferent ductules • • • • • • In testis sperms develop from Spermatogonia cells in ductus deferens Sertoli cells of seminiferous tubules Leydig cells of seminiferous tubules Spermatogenic cells C Spermatozoa in efferent ductules • Spermatocytogenesis: it includes 1. Mitosis in spermatogonia 2. Differentiation of spermatogonia into primary spermatocytes. 3. Meiosis in spermatocytes • Spermiogenesis: It is the transformation of spermatids into spermatozoa. • The formation of primary spermatocytes from spermatogonia is called spermatocytosis. • The whole process of maturation; starting from spermatogonia to the formation of sperms is called spermatogenesis. • Spermatogenesis begins at puberty. Before puberty, the seminiferous tubules are in the form of cords. • These seminiferous cords have sustentacular cells of Sertoli surrounded by basement membrane. • The spermatogonia cells are sandwiched between the Sertoli cells and basement membrane. • The leftover portion of the process vaginalis that covers the testes is the • Gubernaculum testis • Inguinal canal • Tunica vaginalis • Tunica albuginea • Appendix testis • The leftover portion of the process vaginalis that covers the testes is the • Gubernaculum testis • Inguinal canal • Tunica vaginalis C • Tunica albuginea • Appendix testis • Spermatogenesis begins at puberty. • Before puberty, the seminiferous tubules are in the form of cords. These seminiferous cords have sustentacular cells of Sertoli surrounded by basement membrane. • The spermatogonia cells are sandwiched between the Sertoli cells and basement membrane. • At puberty, the seminiferous cords acquire lumen and become seminiferous tubules. • The spermatogonia start dividing mitotically and produce Type A spermatogonia. • These continue to divide by mitosis and produce more and more Type A spermatogonia. • Allah Subhanahu selects some these Type A spermatogonia cells, and differentiate them into Type B spermatogonia. • They continue mitosis and migrate from the base of Sertoli cells to the lateral walls of Sertoli cells and further differentiate into primary spermatocytes. • Each primary spermatocyte through meiosis-I forms two secondary spermatocytes. • Each lobule contains one to three or even more minute highly convoluted tubules, called seminiferous tubules, embedded in loose connective tissue. Diagram showing microscopic picture of testis. • This loose connective tissue contains, in addition to normal constituent cells, groups of interstitial cells of Leydig, containing yellow pigment granules. • These cells are large and polyhedral, with and eccentric nucleus and poorly staining cytoplasm. They secrete testosterone. • There are about 600 seminiferous tubules, and the length of each is 70 to 80 cm. • Their diameter varies from 0.12 to 0.3 mm. • Each tubule is lined by an epithelium called seminiferous epithelium. • It is complex stratified epithelium consisting of two types of cells, sustentacular cells of Sertolli and spermatogenic cells. • Sustentacular cells of Sertolli are supportive cells and spermatogenic cells are germ cells. • Large cells that nourish developing sperm cells and form the blood-testes barrier are • Primary spermatocytes • Interstitial cells • Sustentacular cells of Sertoli • Myoid cells • Spermatids • Large cells that nourish developing sperm cells and form the blood-testes barrier are • Primary spermatocytes • Interstitial cells • Sustentacular cells of Sertoli C • Myoid cells • Spermatids Blood-testis barrier (BTB) • BTB is a l barrier between the blood vessels and seminiferous tubules of testis. Sertoli cell barrier (SCB) • The name "blood-testis barrier" is misleading in that it is not a blood-organ barrier in a strict sense, but is formed between Sertoli cells of the seminiferous tubule and as such isolates the further developed stages of germ cells from the blood. • A more correct term is the "Sertoli cell barrier" (SCB). • The barrier is formed by tight junctions, adherens junctions, gap junctions and desmosomes between the Sertoli cells, which are supporting cells of the seminiferous tubules, and divides the seminiferous tubule in a basal compartment (outer side of the tubule, in contact with blood and lymph) and an adluminal compartment (inner side of the tubule, isolated from blood and lymph). • The presence of the SCB allows Sertoli cells to control the adluminal environment in which germ cells (spermatocytes, spermatids and sperm) develop. • The barrier also prevents passage of cytotoxic agents (bodies or substances that are toxic to cells) into the seminiferous tubules. • Each Sertoli cell possesses an ovoid nucleus, which is often indented; • Cytoplasm contains numerous organelles, including mitochondria, rough and smooth endoplasmic reticulum, ribosomes, Golgi complex, secretory granules, microfilaments and microtubules. • The filaments and tubules probably play a part in bringing about the changes in the Sertoli cells that permit the germ cells to ascend the sides of the cells in their deep recesses, to be released finally as sperms. • The functions of the Sertoli cells include: • 1. The support, protection, and release of the spermatogenic cells. • 2. The nourishment of the spermatocytes, spermatids, and spermatozoa. • 3. The phagocytosis of the residual bodies derived from the spermatids. • 4. The secretion of fluid into the lumen of the seminiferous tubule for the transport of sperms. • 5. The formation of small quantities of estrogens. • From the ejaculatory duct, sperm cells travel directly into the • Vas deferens • Prostatic part of urethra • Seminal vesicle • Membranous part of urethra • Prostate gland • From the ejaculatory duct, sperm cells travel directly into the • Vas deferens • Prostatic part of urethra C • Seminal vesicle • Membranous part of urethra • Prostate gland