(El Paso) HCA DSRIP - Psychiatric Telemedicine (00091343
advertisement

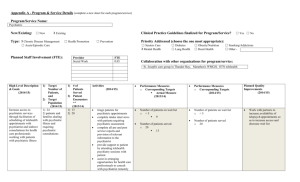
PSYCHIATRIC TELEMEDICINE Identifying Project and Provider Information: Category 1: Introduce, Expand, or Enhance Telemedicine/Telehealth; Project Option 1.7.1: Implement telemedicine program to provide or expand specialist referral services in an area identified as needed to the region; 094109802.1.1; HCA Las Palmas Del Sol (094109802). o Required Core Project Components: Provide patient consultations by medical and surgical specialists as well as other types of health professional using telecommunications. Conduct quality improvement for project using methods such as rapid-cycle improvement. Activities may include, but are not limited to, identifying project impacts, identifying “lessons learned,” opportunities to scale all or part of the project to a broader patient population, and identifying key challenges associated with expansion of the project, including special considerations for safety-net populations. Project Description: This plan would expand coverage through the use of a contracted vendor to provide for the evaluation of acute behavioral health patients in the Emergency Departments. Currently, the process of obtaining a consult can take up to two weeks or more, during which time the patient is in the Emergency Department the entire time. A tele-psychiatric consultation could potentially have a turn-around disposition time of about an hour. The availability of psychiatric consultation in the Emergency Department through the tele-psychiatry model would provide immediate access to psychiatric services currently not available to the patient, provide needed guidance to the Emergency Department physicians, and facilitate the management of psychiatric patients through the ED. We believe this would enhance the quality and appropriateness of patient care, lead to earlier and more appropriate pharmacologic interventions that will expedite the stabilization and disposition of patients. To validate the effectiveness of the program, we will design and conduct process improvement activities for this tele-psychiatry program once it has been implemented to promote higher quality and efficiency standards. Validation processes will include reduction of psychiatric hold hours in the Emergency Departments, improve clinical outcomes, and increase patient satisfaction and safety. o Goals: Establish telemedicine capability in the Emergency Departments to include 24/7 availability of tele-psychiatry to provide for the evaluation of the acute behavioral health patient and provide guidance and support to the Emergency Department physicians. Improve the quality and appropriateness of care provided to behavioral health patients through earlier and more accurate diagnosis. The availability of tele-psychiatry should lead to earlier implementation of the most appropriate therapy. Earlier and more appropriate psychiatric intervention may result in some behavioral health patients being stabilized in the Emergency Department and not requiring transfer for inpatient psychiatric services. o Challenges: Analyzing impact and benefit from implementing a telemedicine program to address psychiatric needs in El Paso; training physicians and staff on new telemedicine equipment; software and connectivity issues; accurately measuring the change in service availability and patient satisfaction; patient and family perception of psychiatric healthcare delivery via this modality; collaboration of care between the tele-psychiatric professionals and the local psychiatric hospitals. Starting Point/Baseline: Neither facility has inpatient psychiatric beds or services, neither facility is licensed as a psychiatric facility, and neither facility has psychiatric consultation available in its Emergency Department (ED). Rationale: o Behavioral health consumers frequently wait hours or even days in crowded ED’s before receiving psychiatric evaluation and placement. Hospital reports show that patients with behavioral health concerns typically stay longer and yield less reimbursement than medical patients. o One of the greatest challenges facing the U.S. healthcare system is to provide quality care to the large segment of the population which does not have access to specialty physicians because of factors such as geographic limitations or socioeconomic conditions. The use of technology to deliver health care from a distance, or telemedicine, has been demonstrated as an effective way of overcoming certain barriers to care, particularly for communities located in rural and remote areas. In addition, telemedicine can ease the gaps in providing crucial care for those who are underserved, principally because of a shortage of sub‐specialty providers. o The use of telecommunications technologies and connectivity has impacted real‐world patients, particularly for those in remote communities, especially communities such as El Paso. This work has translated into observable outcomes such as: improved access to specialists; increased patient satisfaction with care; improved clinical outcomes; reduction in emergency room utilization; cost savings. o Nowhere are these benefits more evident than in Texas. With a land mass area of 268,820 square miles and a growing population of 25.1 million, Texas is the second largest U.S. state by area and population. Its population growth rose more than 18.8 percent between 2000 to 2009, reflecting an increase that is more than double the national growth in this period. This rapid growth is attributed to a diversity of sources such as natural increases from the total of all births minus all deaths, and to a high rate of net immigration from other states and countries. Along with the increase in population, an ever‐growing aging population has significantly affected the demand on the healthcare workforce as demands for quality care increased. Related Category 3 Outcome Measure(s): OD-2: Potentially Preventable Admissions; IT-2.4: Behavioral Health/Substance Abuse (BH/SA) Admission Rate; (094109802.3.1). Relationship to Other Projects: This project is part of LPDS’s larger plans to expand and develop primary care and specialty care services, while improving access to care and containing the costs of care. Specifically, this project will complement LPDS’s Physician and Mid-Level Recruiting and Training project (094109802.1.4) and Outpatient Women’s Imaging Services Expansion project (094109802.1.2); each of these projects is intended to increase access to important health care services for patient populations with an identified need and an identified lack of timely access. Furthermore, this project will complement LPDS’s Electronic Medical Records project (094109802.2.1) to the extent that both projects will strengthen the technological infrastructure in use at LPDS, and will maximize the benefits of that technology from the standpoint of cost, quality of care, and access to care. Relationship to Other Performing Providers’ Projects in the RHP: TBD Plan for Learning Collaborative: TBD Project Valuation: $7,633,758. The valuation of each LPDS project takes into account the transformational impact of the project, the population served by the project (both number of people and complexity of patient needs), the alignment of the project with community needs, and the magnitude of costs avoided or reduced by the project. In particular, this project has been valued based on the costs that will be incurred to develop the technological infrastructure necessary to the project’s implementation, and the current severe lack of access to appropriate psychiatric care for patients presenting at the emergency department. 094109802.1.1 1.7.1.X HCA Las Palmas Del Sol 094109802.3.1 IT-2.4 Related Category 3 Outcome Measure(s): Year 2 (10/1/2012 – 9/30/2013) Milestone 1: Establish baseline for metrics P-4.2 and I-12.1. Metric 1: Establish baseline for future years. Milestone 1 Estimated Incentive Payment: $1,874,284 1.7.1 PSYCHIATRIC TELEMEDICINE 094109802 Behavioral Health/Substance Abuse (BH/SA) Admission Rate Year 3 (10/1/2013 – 9/30/2014) Milestone 3 [P-4]: Implement or expand telehealth program for targeted health services, based upon regional and local community need. Year 4 (10/1/2014 – 9/30/2015) Milestone 3: Estimated Incentive Payment: $2,050,687 Milestone 2 Estimated Incentive Payment: $2,044,743 Year 2 Estimated Milestone Bundle Amount: $1,874,284 Year 3 Estimated Milestone Bundle Amount: $2,044,743 Milestone 4 Estimated Incentive Payment: $1,694,046 Year 4 Estimated Milestone Bundle Amount: $2,050,687 TOTAL ESTIMATED INCENTIVE PAYMENTS FOR 4-YEAR PERIOD: $7,633,758 91343 Milestone 4 [J-12.1]: Increase number of telemedicine visits for each specialty identified as high need. Metric 4 [J-12.1]: Number of tele-medicine visits. Baseline/Goal: 5% increase over DY4. Data Source: HER encounter records from tele-medicine program Milestone 2: Designate hire personnel of terms to support and/or manage the project/intervention Metric 1 [P-4.2]: Documentation of the quantity of actual telehealth services delivered after implementation. Baseline/Goal: Provide services to 10% of all BH/SA patients in ED. Data Source: Log of tele-services by type of health care professionals and type of service. Year 5 (10/1/2015 – 9/30/2016) Year 5 Estimated Milestone Bundle Amount: $1,694,046