Research Proposal
advertisement

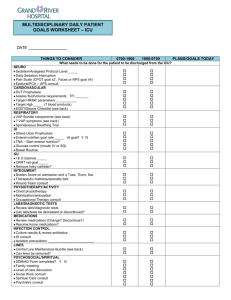
eMETHODS Details of Knowledge Translation Intervention The implementation strategy, consisting of an educational strategy, reminder systems and local implementation teams led by local opinion leaders (eTable 2), was based on the awareness, agreement, adoption and adherence model [1-3] and a framework developed for guideline implementation in the ICU [4]. The framework in these models emphasizes the specific roles of the knowledge translation interventions and considers the perspectives of both providers (i.e. ICU clinician) and healthcare systems (i.e., ICU). Within these models, education raises clinician awareness, local opinion leaders are the enablers, and reminders can reinforce adherence. The 14 guideline recommendations were divided into sections targeting the most appropriate clinician group (e.g., airway management targeted to respiratory therapists, antibiotic recommendations targeted to physicians). Each group was provided a full document and an executive bedside reference guide. The educational strategy was developed by the central study team, which consisted of a multidisciplinary team of 2 physicians (JM, TS), an ICU nurse educator, and a respiratory therapist. A standardized 30-minute slide presentation was developed in 3 formats: (1) electronic version for groupbased teaching, (2) paper-based handout for one-on-one teaching, and (3) a web-based version for individual learning. A document itemizing frequently asked questions (FAQs) was available along with selected key VAP publications, and the published VAP guidelines [5,6]. A web-based self-assessment quiz was developed for all multidisciplinary ICU clinicians to assess their knowledge about VAP and the guideline recommendations. The reminder systems consisted of a bedside patient rounds checklist (incorporating the recommendations) integrated into daily morning bedside patient rounds, and monthly newsletters (each focusing on a specific recommendation) prepared by the central study team, distributed to each ICU. Page 1 of 12 Local opinion leaders assembled a local guideline implementation team consisting of an ICU physician, nurse or nurse educator, respiratory therapist, and a pharmacist. The implementation team was responsible for the educational strategy and reminders. Before study initiation, a one-day workshop was held for all opinion leaders, during which educational materials were distributed, change concepts introduced, and guideline use discussed. The initial implementation strategy was standardized in all ICUs. After baseline data collection, at each site, the local implementation teams presented educational materials (e.g., group or one-on-one presentations to ICU staff, ICU housestaff seminars, email distribution of materials and/or group presentation to ICU attending physicians), distributed educational materials at the bedside (e.g., summary of guidelines, illustrations, FAQs, etc) and introduced the reminder systems. Details of VAP Adjudication Process Patients were screened daily, in consultation with the attending physician, by research coordinators for the development of clinically suspected VAP according to predefined criteria. A clinically suspected VAP was defined as new or persistent infiltrates on a chest x-ray plus 2 of abnormal white blood cell count, presence of fever or hypothermia, purulent sputum, and deterioration in gas exchange [7]. If the attending physician agreed that a clinical suspicion of VAP was present, this was entered into the case report form. Once the patient was discharged from the ICU, the site principle investigator reviewed the case report form to ascertain that the patient’s clinical course, culture results and response to antibiotics was compatible with VAP. Thereafter, once the patient was discharged from the hospital, all cases of suspected VAP were reviewed by the central adjudicators (TS, JGM) again to ascertain that criteria were met for a clinical suspicion of VAP and that the patient’s clinical course, results of any cultures and response to antibiotics were compatible with VAP. For each suspicion of VAP, the appropriateness of empiric therapy and whether empiric therapy was initiated with monotherapy or combination therapy was abstracted. For patients who were adjudicated for as having Page 2 of 12 VAP the duration of antibiotic therapy was determined. For patients who were not adjudicated to not have VAP, appropriate discontinuation of antibiotic therapy was determined. Page 3 of 12 eReferences 1. Abraham C, Sheeran P, Johnston M. From health beliefs to self-regulation: the theoretical advances in the psychology of action control. Psychol Health 1999;13(4): 569-593. 2. Pathman D, Konrad T, Freed G, Freeman V, Koch G.. The awareness-to-adherence model of the steps to clinical guideline compliance: the case of pediatric vaccine recommendations. Med Care 1996; 34 (9): 873-89. 3. Kreuter M, Holt C. How do people process health information? Applications in an age of individualized communication. Current Directions in Psychological Science 2001;10(6): 206-209. 4. Sinuff T, Cook D, Giacomini M, Heyland D, Dodek P. Facilitating guideline adherence in the intensive care unit: A Multicentre Study. Crit Care Med 2007; 35(9): 2083-2089. 5. Muscedere J, Dodek P., Keenan S, et al. for the VAP Guidelines Committee and the Canadian Critical Care Trials Group. Comprehensive Evidence-Based Clinical Practice Guidelines for Ventilator Associated Pneumonia: Prevention. J Crit Care, 2008; 23(1): 126-137. 6. Muscedere J, Dodek P, Keenan S, et al. for the VAP Guidelines Committee and the Canadian Critical Care Trials Group. Comprehensive Evidence-Based Clinical Practice Guidelines for Ventilator Associated Pneumonia: Diagnosis and Treatment. J Crit Care, 2008; 23(1): 138-147. 7. Horan T, Andrus M, Dudeck M. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008; 36(5): 309-332. Page 4 of 12 eFigure 1: Variability in the Incidence of Ventilator Associated Pneumonia Across Sites Legend for eFigure 1: Variability of the incidence of ventilator associated pneumonia across the 11 sites over a 24-month duration. VAP = Ventilator Associated Pneumonia Page 5 of 12 eTable 1: VAP Guideline Prevention, Diagnosis, and Treatment Recommendations Prevention Recommendations Exclusions Route of Intubation We recommend that the orotracheal route of intubation should be used when intubation is necessary. Maxillofacial trauma Head and neck surgery Difficult intubation No exclusions Frequency of Ventilator Circuit Changes We recommend new circuits for each patient, and changes if the circuits become soiled or damaged, but no scheduled ventilator circuit changes. HMEa soiled Excessive moisture on We recommend changes of heat and moisture exchangers HME for each new patient every 5-7 days, and as clinically indicated. Frequency of Change Of Airway Humidification No exclusions Type of Endotracheal Suctioning System We recommend the use of closed endotracheal suctioning system. Frequency of Change of Endotracheal Suctioning System Soiled or tear in outer sleeve Malfunction of system We recommend that closed endotracheal suctioning systems be changed for each new patient and as clinically indicated. Nasally intubated, Tracheostomy tube We recommend the use of subglottic secretion drainage in Difficult endotracheal patients expected to be mechanically ventilated for > 72 intubation hrs. Subglottic Secretion Drainage Page 6 of 12 Patient on vasopressors or undergoing We recommend that the head of the bed be elevated to 45 resuscitation degrees. Where this is not possible, attempts to raise the Spine unstable or not head of the bed as near to 45 degrees as possible should be cleared considered. Pelvic instability or fractures Prone position Intra aortic balloon pump in femoral vessels Obesity Procedures (includes bathing) Semi-Recumbent Positioning Oral Antiseptic: Chlorohexidine The use of the oral antiseptic chlorohexidine should be considered. a Allergy Lack of access to patient’s oral cavity HME = Heat and Moisture Exchangers Diagnosis Recommendation Exclusions Patients known to be colonized or previously We recommend that, if empiric antibiotic therapy is being infected with initiated at the time VAP is suspected that endotracheal Pseudomonas sp. or aspirates with nonquantitative cultures be used as the MDRa organisms, initial diagnostic strategy. Immunocompromised patients Invasive vs. Non-Invasive Techniques a MDR = Multi-drug Resistant Treatment Recommendations Exclusions Empiric vs. Delayed Culture Directed Therapy We recommend empiric therapy when there is a clinical suspicion of VAPa. Page 7 of 12 No exclusions Mono therapy vs. Combined Empiric Antibiotic Therapy We recommend appropriate spectrum effective monotherapy for empiric therapy of VAP. Choice of Antibiotics (e.g., Antibiotic “A” vs. “B”) Patients known to be colonized or previously infected with Pseudomonas sp. or MDRb organisms, Immunocompromised patients No exclusions We recommend that the antibiotic treatment of VAP be based on local resistance patterns and patient factors. Antibiotic Discontinuation Strategy Based on Clinical Criteria No exclusions We recommend that an antibiotic discontinuation strategy be utilized for the empiric treatment of suspected VAP. Duration of Antibiotic Use for Confirmed VAP We recommend a maximum of 8 days of antibiotic therapy for the treatment of VAP, in patients who receive adequate initial antibiotic therapy. a VAP = Ventilator Associated Pneumonia b MDR = Multi-drug Resistant Page 8 of 12 Immunocompromised patients eTable 2: Multifaceted Behavior Change Intervention Intervention Description Education Educational Package Consisting of: Summary of guideline recommendations targeted for each ICUa clinician group Bibliography of evidence based literature to support each recommendation Bedside illustrations and algorithms (included all recommendations) Frequently asked questions and answers Power-point presentation for multi-disciplinary rounds or seminar presentation Electronic version of power-point presentation Educational material for one-on-one teaching Web-based self assessment quiz with answers Bedside daily morning rounds checklist for the following recommendations: Semirecumbent position (head of bed elevation >45 degrees) Use of chlorhexidine for oral care Daily assessment of suspicion of VAPb Daily assessment for discontinuation of antibiotics for VAP treatment Monthly electronic distribution of newsletter highlighting a specific VAP guideline recommendation. Incorporation of guideline recommendations into pre-printed orders. 3-4 local team consisting of a local opinion leader (usually a physician) plus an ICU nurse, ICU nurse educator, ICU respiratory therapist, and/or ICU pharmacist. Guideline implementation team was responsible for provision of education to all ICU clinician groups at baseline and throughout the study. Reminders Local Opinion Leader and Guideline Implementation Team aICU b = Intensive Care Unit VAP = Ventilator Associated Pneumonia Page 9 of 12 eFigure 2: Example of Concordance Rate Calculation for VAP Guideline for a Patient Admitted to the ICU Concordance Rate is Patient days for patients who are eligible for semirecumbency and are semirecumbent PLUS patients who _______________are ineligible for semirecumbency and are not semirecumbent____________________ Total Number of Patient Days For the example depicted in the table below, guideline oncordance rate for semirecumbency is 83%, where eligibility for semi-recumbency recommendation: 1. 2. 3. 4. 5. Patient has been intubated greater than 48 hours Patient is not hypotensive (Mean > 65 mmHg) Patient is not undergoing a procedure at time of assessment Patient is not receiving nursing care at time of assessment Patient has a specific contra-indication for semirecumbency (e.g., Spine fracture) Page 10 of 12 eTable 3: Example of Concordance for VAP Guideline for a Patient Admitted to the ICU Guideline Recommendation Prevention Semirecumbency Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Observation Eligible for Guideline recommendation (Y/N) Received Guideline recommendation (Y/N) Guideline Concordance (Y/N) Patient semirecumbent Hypotension at time of guideline assessment Y Y Y N N Y Central line insertion at time of guideline assessment Patient prone due to ARDS management Patient being bathed Patient supine and no reason found N N Y N N Y N N Y Y N N Does not have tube, ICU ran out of tubes Y N N Endotracheal Aspirate Y Y Y Ceftriaxone Ceftazidime and Ciprofloxacin Y Y Y N Y N Use of Subglottic Secretion Drainage Diagnosis Endotracheal Aspirate for Suspected VAP Treatment Single BroadSpectrum Antibiotic for initial Treatment of VAP Episode 1 Episode 2 Page 11 of 12 eTable 4: Clinical Outcomes for Each Study Period Clinical Outcome Baseline (n = 330) 6 Month (n = 330) 15 Month (n = 330) 24 Month (n = 330) Duration of Mechanical Ventilation (days) median [IQR a] 8.9 [4.6, 45.2] 9.6 [4.7, 28.8] 8.5 [4.7,23.8] 8.1 [4.5, 28.3] 0.43 ICUb LOSc (days) median [IQR] 13.7 [7.4,undefined] 14.1 [7.0,undefined] 13.2 [7.7,69.5] 12.6 [7.4,undefined] 0.20 Hospital LOS (days) median days [IQR] 62.0 [21.2,undefined] 57.1 [21.8,undefined] 48.7 [20.7,undefined] 43.5 [18.6,undefined] 0.02 ICU Mortality No. (%) 94 (28.5) 85 (25.8) 72 (21.8) 84 (25.4) 0.26 Hospital Mortality No. (%) 126 (38.2) 119 (36.1) 98 (29.7) 100 (30.3) 0.03 a IQR = Interquartile Range ICU = Intensive Care Unit c LOS = Length of Stay b Page 12 of 12 P-value