Presentation - Kuwait Anesthesia & Critical Care Council
advertisement

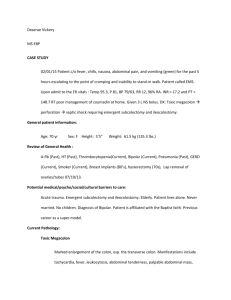
VAP, not on my WATCH !!! France Ellyson ANM, MNH ICU Kuwait 2014 • http://www.youtube.com/watch?v=RueE4 rMU Introduction Mechanical ventilator is one of the most important life saving devices used in conditions like: • Respiratory failure • Protection of airway • Head injury • Postoperative • Shock What is Ventilator Associated Pneumonia? • A nosocomial pneumonia associated with mechanical ventilation (either Endotracheal tube or Tracheostomy) that develops within 48 hours or more of hospital admission and which was not present at time of admission. • Now considered a PREVENTABLE HEALTHCARE ERROR National institute of health excellence (NICE) -2007 center for disease control and prevention What is VAP? • Pneumonia that occurs at least 2 days after a patient is intubated (CDC GUIDELINES) • The presence of the ET-tubes leads to VAP (not the ventilator) • VAP rate increases with the # of days on mechanical ventilation • Mortality varies according to the type of organisms • Multi-resistant organisms have a higher mortality Epidemiology • Hospital acquired pneumonia (HAP) is the second most common hospital infection. • VAP is the most common Intensive Care Unit (ICU) infection. • 90% of all nosocomial infections occuring in ventilated patients are pneumonias. • Causes more death than any of the other healthcare associated infection Incidence • VAP occurs in 10-20% of all ventilated patients Crit Care Clin (2002) • Incidence increases with duration of MV: 3%/day for first 5 days, 2%/day for 6-10 days and 1%/day after 10 days. • The incidence of VAP is highest in the following groups: Trauma, burns, neurosurgical post-op pts • Mortality rate is 37% and 43% with antibiotic resistant organism Critical Care Societies Collaborative (CCSCs) Incidence Cont…. • Increases ventilatory support requirements and ICU stay by 4.3 days • Increases hospital LOS (length of stay) by 4 to 9 days • Increases medical cost ($5,000 to $40,000 per VAP) Critical Care Medicine 2005;33:2184-93 Causative Organisms: Early onset • Hemophilus influenza • Streptococcus pneumoniae • Staphylococcus aureus (methicillin sensitive) • Eschrichia coli • Klebsiella Late onset • Pseudomonas aeruginosa • Acinetobacter • Staphylococcus aureus (methicillin resistant) How is the pneumonia happening? • Most plausible mechanism and source: – Leakage around the ETT cuff (primary route)… aspiration of bacteria – High rate of the oropharyngeal or tracheobronchial colonization (gram neg bacilli) – Bacteria from the tongue – Bacteria from environment: caregivers’ hand, air, water, dust – Contaminated equipment (ventilator tubing, aerosol, etc.) – Suctioning equipment Risk Factors: Host Related • • • • • • Medical / surgical disease Immunosuppression Malnutrition (Alb<2.2g/dl) Advanced age Pt’s position (supine) LOC – impaired LOC, delirium, coma • Medications – sedation, steroids, previous antibiotic use, NM blockers • Number of intubationsreintubations Risk Factors: Device Related • Mechanically ventilated with ETT or Tracheostomy tube • Prolonged MV - MV > 48 hours • Number of intubations, reintubations • NGT or Orogastric tube • Use of humidifier Risk Factors: Health Care Personnel Related • Improper hand washing • Failure to change gloves between contacts with pts • Failure to wear personal protective equipment when required Pathogenesis Bacteria enter the lower respiratory tract via following pathways: • Aspiration of organisms from the oropharynx and GI tract (most common cause) • Direct inoculation • Inhalation of bacteria Aspiration ETT/T • Holds vocal cords open • Predispose pt to micro and macro aspiration of colonized bacteria from oropharynx • Leakage of secretions containing bacteria around ETT cuff NGT/OGT • Interrupts gastroesophageal sphincter leading to GI reflux and aspiration • Increase oropharyngeal colonization and stagnation of oropharyngeal and nasal secretions A New Streamlined Surveillance Definition for VentilatorAssociated Pneumonia Critical Care Med 2012 vol.40, no.1 Any one of the following: • NO CONSENSUS AMONG PHYSICIANS!!! How do we Diagnose? 2-1-2 Radiologic evidence X 2 Consecutive days • New, progressive or persistent infiltrate • Consolidation, opacity or cavitation How do we diagnose? 2-1-2 Clinical Signs: At least 1of the following: • Fever > 38 °C with no other recognized cause • Leukopenia (<4,000 WBC/mm3) or leukocytosis (>12,000 WBC/mm3) How do we Diagnose? 2-1-2 At least 2 of the following: • New onset of purulent sputum or change in character of secretions • New onset or worsening cough, dyspnea or tachypnea • Rales or bronchial sounds • Worsening gas exchange (decreased sats, increased oxygen requirements) Treatment Protocol • Start when VAP is suspected • Do not delay • Individualized to institution – Hospital epidemiologic data, drug cost and availability • Individualized to pt - Early onset vs Late onset of VAP, prior antibiotic use, underlying disease, renal, liver, etc • Surveillance cultures Duration of Treatment • Standard duration 7-14 days • Longer duration > 14-21 days risk of toxicity and resistance • Shorter < 7 days risk of recurrence • Depends on severity • Isolation of microorganism Prevention • Specific practices have been shown to decrease VAP • Strong evidence that a collaborative, multidisciplinary approach incorporating many interventions is paramount • Intensive education directed at nurse and respiratory care practitioners resulted in a 57% decrease in VAO Crit Care Med (2002) The VAP Bundle BUNDLE • “Group of evidence based interventions that whenever implemented together result in better outcomes” Introduction of VAP BUNDLE 1. Elevation of HOB to between 30-45° 2. Daily sedative interruption and daily assessment of readiness to extubate 3. The utilization of endotracheal tubes with subglottic secretion drainage (Not at MNH yet) 4. Stress ulcer disease prophylaxis – including initiation of safe enteral nutrition within 2448 hours of ICU admission 5. IN 2010 5TH COMPONENT of Daily oral care and decontamination with Chlorhexidine Crit.Care 2012 vol.40, no.1 Additional Evidence-Based Component of Care: HANDWASHING • Single most important and ( easiest!!) method for reducing the transmission of pathogens • Use of waterless antiseptic preparations is acceptable and may increase compliance HOB 30-45° • HOB 30-45° unless contraindicated • Especially recommended for Neuro population • To prevent aspiration during enteral feeding Daily sedative interruption and daily assessment of readiness to extubate OVERSEDATION predisposes pts to: • • • • • Thromboemboli Pressure ulcers Gastric regurgitation and aspiration VAP Sepsis Daily sedative interruption and daily assessment of readiness to extubate OVERSEDATION predisposes pts to: • • • • Difficulty in monitoring neuro status Increased use of diagnostic procedures Increased ventilator days Prolonged ICU and Hospital stay Daily Wake-up • Every pt must be awakened daily unless contraindicated • Daily weaning assessments reduce the duration of MV • If pt becomes symptomatic – rebolus and restart infusion at lower dose than original dose • Goal is to decrease sedation Stress Ulcer Prophylaxis • Sucralfate, H2 receptor blocker and proton pump inhibitor – increases gastric ph and minimize bacterial colonization and reduces risk of VAP Enteral Feedings • Initiation of safe enteral nutrition within 24-48 hours of ICU admission • Early initiation decreases bacterial colonization • HOB 30-45° • Routinely + PRN verification tube placement Additional Evidence-Based Component of Care: • Deep venous thrombosis (DVT) prophylaxis (unless contraindicated) – TED stockings – SCD machine – Heparin S/C Deep venous Thrombosis Prophylaxis and early mobility practices • Pt turning Q 2hours increase pulmonary drainage and decreases risk VAP • Early mobilization Daily Oral care • Oral assessment Q shift • Brushing teeth, tongue and gums with a soft toothbrush (minimally twice daily) • Moisturizing agent for mouth • Antiseptic rinse • Swabs are not effective at removing plaques • Chlorhexidine decontamination of mouth • Routine suctioning of mouth to manage oral secretions and minimize risk of aspiration Sage Oral Care Products • http://www.youtube.com/watch?v=MYO_Md dtYNs Mouthcare • Using chlorhexidine gluconate 0.12% (Peridex) solution every 6-12 hours to perform oral care, according to your protocol • solution is used to rinse the patients’ mouth. ET Tube Care • Cuff pressure (between 20-30cm H2O) • Oral intubation preferred • Continuous or intermittent sub-glottic aspiration • Avoid unnecessary disconnection of MV circuit • Open vs close suctioning… benefits is not demonstrated yet Prevent micro-aspiration of secretions • 100-150ml of oral secretion can accumulate in patient mouth in 24hrs • Mouth can colonize as quickly as 24hr after admission • Intermittent and continuous subglottic suctioning • Suctioning of the mouth before position change Suctionning of Oral Secretions • Suction oropharyngeal secretions Q 2hours, before repositionning, before suctionning ETT, before mobilizing patient and PRN • Gently follow tongue to suction back of throat • Use yankauer suction Suctioning Oral suction devices (Yankauer) • Follow policy for use and storage • ?Harbor potentially pathogenic bacteria within 24 hours • Date and change Q day • Rinse with sterile water after each use • Allow to air dry Subglottal Suctioning Should be done using a 14 French sterile suction catheter • Prior to ETT suctionning • Prior to pt change of position • Prior to extubation * Continuous subglottic ETT with dedicated lumen above cuff may reduce risk of VAP Prevent contamination of equipment • Ventilator tubing • Heat and moisture exchangers (green filters) are preferred over humidifiers (CDC B-II) • Sterile suctioning • Be careful with the tubing of the ventilator when you suction patient… • Remove contaminated condensate from ventilator circuit (CDC, A-II) Summary • Nosocomial pneumonia and especially VAP are the most frequent infectious complications in the ICU, and they significantly contribute to morbidity and mortality • VAP is an important determinant of ICU and Hospital lengths of stay and healthcare costs • No standard to diagnose • Several simple preventative measures (VAP bundle) and timely initiation of appropriate antibiotics ensure better outcomes in pts with VAP • http://www.youtube.com/watch?v=Ehi2Vt dRc References National Guideline Clearinghouse (current). Guideline Summary NGC-6634: Prevention of ventilator-associated pneumonia. Retrieved from: http://files.imd.com/medinfo/material/f97/4eb0b88d44aece1112f7bf97/4eb0b8a944 aece1112f7bf9a.pdf Niel-Weise, B. & all. (2011). An evidence-based recommendation on bed head elevation for mechanically ventilated patients. Critical Care 2011, 15:R111. Postma, D.F., Sankatsing, S.U.C., Thijsen, S.F.T. & Enderman, H. (2012). Effetcs of chlorhexidine oral decomtamination on respiratory colonization during mechanical ventilation in intensive care unit patients. Infection Control and Hospital Epidemiology, vol 33 no.5, pp.527-530. Safer Healthcare now (2012). Ventilator associated pneumonia. Retrived from: http://www.saferhealthcarenow.ca/en/interventions/vap/pages/default.as px Safer Healthcare now (2012). Getting Started Kit. Retrieved from http://www.saferhealthcarenow.ca/EN/Interventions/VAP/Documents/VA P%20Getting%20Started%20Kit.pdf References Alhazzani, W. & all. (2013) Tooth brushing for critically ill mechanically ventilated patients: a systematic review and meta-analysis of randomized trials evaluating ventilatorassociated pneumonia. DOI: 10.1097/ccm.0b013e3182742d45 Center for Disease Control and prevention(2011). Improving Surveillance for VentilatorAssociated Events in Adults. Obtain from MUHC Infection Control Departement. Chan, E.Y., Ruest, A., Omeade, M. & Cook, D.J (2007). Oral decontamination for prevention of pneumonia in mechanically ventilated adults: systematic review and meta-analysis. BMJ, doi: 10.1136/bmj.39136.528160.BE Fagon, J-Y. (2011). Biological markers and diagnosis of ventilator-assocaited pneumonia. Critical Care 20111, 15:130. Koenig, S.M. & Truwit, J.D. (2006) Ventilator-assocaited pneumonia: diagnosis, treatment, and prevention. Clinical Microbiology Reviews, doi: 10.1123/CMR.00051-05 Hillier B. Wilson C. Chamberlain D. King L. (2013). Preventing ventilator-associated pneumonia through oral care, product selection, and application method: a literature review. AACN Advanced Critical Care. 24(1):38-58. Insitute for Healthcare Improvement (2011). IHI ventilator bundle: daily oral care with chlorhexidine. Retrieved from http://www.ihi.org/knowledge/pages/changes/dailyoralcarewithchlorhexidine.aspx