I didn`t know bees could do that! An Anaphylaxis Case Study
advertisement
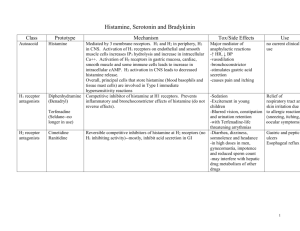
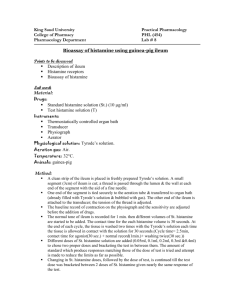
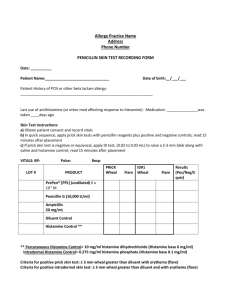
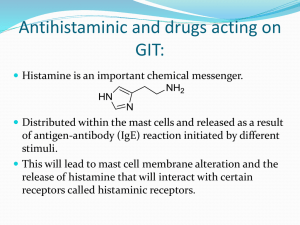
I DIDN’T KNOW BEES COULD DO THAT! AN ANAPHYLAXIS CASE STUDY Megan Brashear, BS, CVT, VTS (ECC) DoveLewis Emergency Animal Hospital Portland, OR An allergic reaction is defined as a systemic reaction in response to an allergen. Inflammation is often the most obvious sign of an allergic reaction as we will see facial swelling and urticaria in minor reactions. More serious reactions will appear as vomiting and diarrhea in addition to the swelling/hives. When an allergic reaction is severe it is deemed an anaphylactic reaction, and if these patients are not treated quickly the reaction can become fatal. Histamine is the main culprit in these allergic reactions. Histamine is complex – it is responsible for at least 23 physiologic functions, and continues to be examined. There are at least four histamine receptors in the body, and the effects seen depend on which receptor is activated. The H1 receptor is most responsible for the clinical signs seen with anaphylactic reactions. Mast cells and basophils are mostly responsible for histamine manufacturing and release and can be activated by any number of allergens. The H1 receptor interacts with the endothelium and will cause vasodilation and an increase in vascular permeability. H1 receptors are found all over the body – in the brain, respiratory tract, the GI tract, heart, and vascular system. H2 receptors regulate the right side of the heart muscle and are also involved in gastric acid secretion. Within the cardiovascular system, histamine is responsible for regulating cardiac function, vascular resistance, and circulating volume. When histamine concentration increases within the vascular system, arterioles dilate causing a sudden drop in both systolic and diastolic blood pressure. Capillary beds become more permeable and contribute to the blood pressure drop. The response is both time and dose dependent. In patients experiencing massive histamine release from an anaphylactic reaction, this drop in blood pressure quickly causes hypoperfusion to major organs and if not treated quickly will cause death. These patients will present collapsed and comatose and need close monitoring of renal values as they recover. Within the respiratory system, histamine release works on the smooth muscles of the airway and causes constriction, while also causing vasodilation. That vasodilation and increased capillary permeability leads to pulmonary edema. With histamine release there is also an increase in mucus secretion. With anaphylactic patients we may see tachypnea that will continue longer than just the initial exam period. These patients should be given supplemental oxygen and monitored for hypoxia. Hypoxia can be a trigger event for more histamine release and must therefore be avoided. Histamine release also stimulates gastric acid secretion which can lead to stomach and duodenal ulceration. With the severe hypotension and hypoperfusion already happening, these patients will often experience hematochezia and hematemesis further complicating their status. Gastroprotectants are important for these patients to prevent eroding gastric ulcers. Bacterial translocation is where the intestinal mucosal barrier breaks down due to poor perfusion, and that can allow gut bacteria to escape into circulation. Sepsis can occur from bacterial translocation so antibiotics should be considered and patients monitored closely for signs of sepsis or declining status. Treatment for simple allergic reactions is aimed at stopping the reaction happening in the body. This is achieved by administering a histamine blocker – most commonly diphenhydramine (2-4mg/kg IM) immediately. A dose of steroids (anti-inflammatory) is also often administered as well (dexamethasone SP 0.125-0.5mg/kg IV). With many of these patients, a reduction in facial swelling and urticaria is often noted after 20-30 min and these patients can continue on oral anti-histamine for 24-48 hours and not see any long term negative effects. When dealing with a more critical anaphylactic reaction, speed and support are vital for patient survival. Within one minute of detecting the insult, the body is flooded with histamine. H1, H2 and H3 receptors are activated; followed by bronchoconstriction, vasodilation, gastric acid secretion, and even inhibited norepinephrine release which compounds the hypovolemic shock the patient is experiencing. In dogs, the hepatic vein quickly becomes congested causing portal hypertension which can lead to GI bleeding, vomiting, and diarrhea. While there is no diagnostic test for anaphylaxis, these patients need symptomatic treatment which involves aggressive fluid therapy to restore and maintain appropriate blood pressure. Crystalloids and most likely colloids will be needed. IV access can be challenging in these patients due to severe hypotension and hypovolemia. Diphenhydramine and gluccocorticoids should be administered to aid in decreasing the reaction, but severe cases may also need epinephrine administered (1:1000; 0.01mg/kg). Blood pressure should be monitored closely and pressors started as needed. Oxygen support will be necessary at least during the resuscitation period and possible ongoing. GI protection is also required, and hematochezia and hematemisis are common. Due to bacterial translocation antibiotics should also be started quickly and the patient monitored closely for sepsis. Disseminated Intravascular Coagulation is a syndrome that can occur with anaphylaxis. DIC is a secondary syndrome known to occur in some cases of severe inflammation. Patients experiencing any systemic inflammation are at risk for developing DIC. The body becomes hypercoagulable due to an inappropriate activation of the clotting system. Micro clots are formed within the vasculature, and can travel/become lodged in capillaries leading to altered blood flow and ischemia. Multiple organ dysfunction and failure can occur as a result. Platelets and clotting factors are used up and soon the patient begins to bleed inappropriately. Usually the bleeding phase is when DIC is noticed in the hospital setting. Diagnosis of DIC is made using the patient’s history and current disease process. A patient with an inflammatory process, elevated clotting times, decreased platelet numbers, inappropriate bleeding (petechia, etc) and declining vital signs (mainly blood pressure) can be diagnosed with DIC. There isn’t one specific test or battery of tests to confirm a DIC diagnosis. The mainstays in treatment of DIC are to attempt to manage the inciting cause. In cases of anaphylaxis, attempting to get the inflammation under control and maintain normal vital sign parameters should continue to be the main goal. Treatment of DIC is aimed at supporting the patient – providing plasma transfusions to replace lost clotting factors, provide red blood cell transfusions if the patient is clinical for blood loss, and consider fresh whole blood transfusions to replace lost platelets. Restoring and maintaining perfusion with crystalloids and colloids is important to in trying to remove inappropriate clotting factors in the early stage of DIC and to ward off ischemic events in the latter stage. Pain management should never be ignored in any critical patient, and DIC is no exception. Pain can lead to vasoconstriction, decreased perfusion, and even hypoxia, so these patients should be kept quiet and comfortable during their hospitalization. Nutrition is also vital to the healing process. Critically ill patients often have low plasma proteins and nutrition is necessary in keeping these levels normal. The rapidly dividing cells of the GI tract also need nutrition, and if possible, it is best to feed these cells directly though trickle feeding via NG or NE tube. Patient vomiting can prevent the placement of these tubes, and in that case IV nutrition should be considered. Gastric and duodenal ulceration is common in anaphylaxis so enteric feeding can be a challenge until that ulceration is treated and the patient feels comfortable enough to eat. While challenging to treat both on emergency admission and as an ongoing critical patient, with aggressive supportive and intensive nursing care these patients can make a full recovery.