AHHSP Final_AU_52710
advertisement

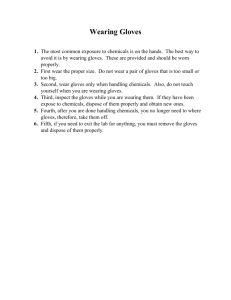
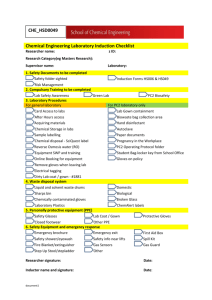
University of Maryland College Park Occupational Health Animal Handler Health and Safety Program Revised Purpose The purpose of the Animal Handler Health and Safety Program (AHHSP) is to protect the health of personnel and laboratory animals by providing: 1. Health and safety information related to the use and care of animals. 2. Occupationally indicated immunizations. 3. Clinical care for individuals with animal related injuries and illnesses. General 1. The AHHSP is part of the University’s Occupational Health Program. Occupational Health is located in the Health Center in Room 0106. Hours of operation are 8:00 AM to 4:30 PM Monday through Wednesday. Appointments may be made by calling (301) 314-8184. 2. University groups responsible for this program are: University Health Center (UHC) Urgent Care: (301) 314-9144 Occupational Health: (301) 314-8172 http://www.health.umd.edu/ Department of Environmental Safety (DES) (301) 405-3960 http://www.des.umd.edu/ Institutional Animal Care and Use Office (IACUC) Amanda Underwood, IACUC Manager (301) 405-5037 http://www.umresearch.umd.edu/IACUC/ Department of Laboratory Animal Resources (DLAR) Dr. Doug Powell, Attending Veterinarian (301) 405-4921 http://www.umresearch.umd.edu/IACUC/carf.htm Eligibility 1. Faculty, staff and students who have direct animal contact are required to enroll in the AHHSP prior to working with any species of vertebrate animals. This Animal Handler Health and Safety Program includes personnel who handle live animals, unpreserved tissues or body fluids, animal cages, cage accessories, animal waste or carcasses (direct contact). 2. Faculty, staff and students with indirect animal contact work in areas where animals are used or housed, but do not handle or touch the animals. Participation in the AHHSP is optional for these individuals. The PI or facility manager is responsible for notifying these individuals that they should consider enrollment. 3. Laboratory, maintenance, housekeeping, security, and other personnel who perform job duties in animal environments. Participation in the AHHSP is optional for these individuals. Each department that could potentially send employees into animal spaces is provided the AHHSP and educated on enrollment policies which are then provided to those working in designated animal zones. 4. Students in course curricula that require the use of vertebrate animals are not required to participate in the AHHSP but are offered enrollment. 5. Visiting scholars and volunteers who handle vertebrate animals are required to participate in the AHHSP if they handle animals for more than 3 months during their visit or work with bats for any amount of time. They are not required to participate in the AHHSP if they already participate in an analogous program at their home institution. 6. Visitors to University sanctioned events (ie. Ag Day) are not covered by this policy. Any event that includes animal activities will provide appropriate hand washing stations and signage to alert visitors of potential hazards from interacting with animals. Procedure The mandatory requirements for enrollment are: 1. Completion of the Animal Handler Risk Assessment form, available at http://www.health.umd.edu/services/occupationalhealth.html. The form must be signed by the Principal Investigator (PI) or supervisor. The Risk Assessment form must be updated any time there is a change in animal related duties, animal species, or the health status of the participant. If species are added or deleted, the Risk Assessment form should be re-submitted listing ALL animals, not just the new species. 2. Completion of the Animal Handler Immunization and Allergy History form, also available at http://www.health.umd.edu/services/occupationalhealth.html. If available, documentation of tetanus vaccination within the last 10 years should accompany this form. 3. Submission of completed Risk Assessment and Immunization/allergy forms to Occupational Health/Health Center, Campus Drive, Bldg. 140, Room 0106, College Park, MD 29742. Review and approval of the completed forms by 2 Animal Handler Health and Safety Program Occupational Health is required before the individual is cleared to work with vertebrate animals. Notification of program enrollment is sent to the individual’s supervisor. Participants can access their clearance records at https://des.umd.edu/training/viewanemp.cfm. 4. Completion of training. A. Participants must complete the Principal Investigator/Animal User (PI/AU) training sponsored by the University Attending Veterinarian. Excerpts of the AHHSP description will be provided to training recipients. B. Individuals who have indirect animal contact and are not enrolled in the program should complete animal-specific training at the discretion of the facility manager where they work. This training is provided by the facility managers and will be documented at the facility level. C. Training for students in course curricula where animals are used is directed by the course syllabus and provided by the instructor. D. Volunteers and visiting scholars must complete animal-specific training depending on their work functions. Conducting and documenting this training is the responsibility of sponsoring faculty or staff. E. Subject matter for training is listed in Appendix A. Program Elements 1. General A. Enrollment in the AHHSP is typically granted for three years, and is tracked in a database maintained by Occupational Health and the Department of Environmental Safety. To maintain enrollment, individuals must update the Immunization and Allergy History form every three years, and immunizations must be kept current. B. Limits: The AHHSP is not meant to cover all the specific concerns that might be encountered in animal facilities, areas or labs, or to limit the requirements of these sites. Nor does this program intend to establish requirements for experiments that have special safety requirements such as the use of infectious disease organisms, hazardous chemicals, lasers or radiation sources, or for individuals with special health needs such as pregnancy or immune deficiency. C. Specific Risks 1. Tetanus vaccination is required every 10 years to work with any vertebrate animal. 3 Animal Handler Health and Safety Program 2. Individuals working with bats, feral animals and sheep are required to schedule an appointment with Occupational Health for further evaluation. 3. Rabies immunization is provided to individuals who have direct contact with research animals potentially infected with rabies; who work with potentially infected body organs or perform post-mortem examinations on selected animals with a history of poorly defined neurological disorders; or who capture or destroy wild animals on campus. Immunization and titer schedules are based on CDC guidelines. Titers will be drawn every two years (Risk Category considered frequent.) 4. Individuals who are at risk for asthma and/or animal allergies based on their Laboratory Animal Handler Immunization and Allergy History form will be notified by Occupational Health to schedule an appointment for further evaluation. Any individual with a history of respiratory problems, animal allergy, or any other related medical problem that the healthcare provider deems appropriate may require a baseline pulmonary function test before working with animals. 5. Individuals at risk of exposure to Q-fever include those who handle or use products of parturition or material contaminated by them (i.e., placenta, amniotic fluid, blood or bedding) from sheep, cattle or cats; and/or individuals with valvular or congenital heart defects, vascular grafts and those who are immunosuppressed. These individuals are advised of the potential risks involved and medical clearance for duty will be determined on a case-by-case basis by the medical provider. 6. Nonhuman primates are not housed at the University. For injuries associated with non-fixed nonhuman primate tissues, CDC guidelines will be followed. D. Injuries and Exposures. Individuals who have an injury or an exposure from working with or around animals need to adhere to the following procedure: 1. Perform the necessary first aid. 2. Report to the Information Desk at the Health Center. If after hours, advice may be obtained from the After Hours Nurse Line at (301) 314-9386. If the injury is potentially severe, individuals should call 911 or report to the nearest emergency room. 3. Employees and supervisors must complete the Report of Work-Related Injury forms. The forms can be found at: http://www.des.umd.edu/riskcomm/wcomp/form/wcomp.pdf 4. Individuals must report the injury as soon as possible to their sponsoring faculty member, instructor or supervisor. 4 Animal Handler Health and Safety Program E. Medical Records. Occupational Health records are maintained by the Health Center. Workers’ compensation records are maintained by the Department of Environmental Safety. 5 Animal Handler Health and Safety Program Appendix A - Training 1. Needle use and disposal. After their use, needles should immediately be placed in an approved sharps disposal container. These containers should always be in the immediate area where needles are used and never be overfilled. Disposal of the containers is through DES. 2. Hand Washing. Even when using gloves, hand washing is important in the prevention of the spread of infectious organisms or other contaminants to both personnel and animals. While the use of exam gloves will greatly decrease the spread of contaminants from a person’s hands, they will not completely eliminate this transfer due to micro- breaks in the glove materials, regardless of type. To be effective, hand washing for 15 to 30 seconds with soap coupled with copious rinsing with free flowing water is required. In situations where hand washing is impractical, or as a supplement to hand washing, alcohol-based hand sanitizing agents are recommended for use. In all situations, hands should be washed after handling any potential source of infection; when exiting any animal facility or laboratory; and prior to consuming any food or drink. 3. Personal Protective Equipment (PPE). A. PPE requirements for working with animals used at the University are listed in the tables found in Appendix A. PPE requirements vary between species, facilities and activities. Open-toed shoes and exposed legs are generally not allowed in animal rooms. B. While masks (surgical or dust/mist respirators) are not required in most situations, their use is permitted if potential exposure to animal allergens is a concern to animal handlers. Dust/mist respirators provide better protection from allergens than surgical masks. If respiratory protection is necessary or requested, the Department of Environmental Safety must be contacted ((301) 405-3960) to evaluate respiratory hazards and recommend appropriate respiratory protection devices. If dust/mist respirators are used on a voluntary basis, contact the Department of Environmental Safety to schedule one-time, required training. C. Non-disposable PPE such as lab coats or scrubs should be laundered on-site in specified laundry rooms or by a professional laundry service aware of potential hazards (not at home). A designated hook/storage area in the lab to hang lab coats should be designated before leaving the laboratory instead of wearing it back to the office or other public areas leading to contamination of those environments. D. In course curricula that require the use of animals, PPE must be used as directed by the course syllabus. 6 Animal Handler Health and Safety Program 4. Food and Drink. Food and drink intended for human consumption are not permitted in animal or laboratory areas. The application of cosmetics or contact lenses is not permitted in animal or laboratory areas. 5. Pregnancy. If an individual plans to become pregnant or finds she is pregnant, she should contact her personal physician to discuss potential hazards in her work environment. 6. Chemical Safety. All hazardous chemicals used in laboratories and animal facilities must be listed on the site’s Chemical Hygiene Plan. The plan must also include work practices, procedures and policies to address potential hazards. Training in the handling of hazardous chemicals is the responsibility of DES and the PI (http://www.des.umd.edu/compliance/factsheet/chemhygiene.html). 7. Biological agents. Training in the handling of biological agents used in animal laboratories and animal facilities is the responsibility of DES and the PI (http://www.des.umd.edu/biosafety/infectious/index.html). 8. Regulated waste. Hazardous and regulated waste must be handled in accordance with the University of Maryland waste disposal guidelines found at http://www.des.umd.edu/hw/rest/manual/index.html. DES must be contacted for pick up of regulated medical waste containers. 9. Physical Injuries. Physical injuries can occur from bites and scratches by bats, ferrets, rabbits, rodents, swine, or any animal with claws and teeth or from their immediate surroundings. Physical strain or trauma from working with animals may occur when lifting the animals improperly or using inadequate/improper restraint techniques. The key to prevention of these types of injuries is proper training of research personnel by qualified individuals who have a background in performing restraint with the species and procedures to be performed. 10. Zoonotic Diseases. Zoonotic diseases are those that can be transmitted from animals to humans. Zoonotic diseases for each species used at the University are described below. Although not common, there is a potential for exposure to such diseases when handling animals and/or tissues. The prevention, detection, and eradication of zoonotic diseases from the animal facility are a primary concern of all who work with the animals. Unfixed animal tissues, animal waste materials, as well as the animals themselves may also transmit zoonotic diseases. The use of proper PPE can reduce this risk. 11. Allergic Hazards. Allergic hazards are associated with breathing or contacting animal hair, dander, or protein allergens. Exposure may cause acute allergies to these (or similar allergens) or the development of allergies later in life. To reduce exposure to allergens, and therefore sensitization, individuals should wear PPE required for the species or procedure to be performed. 12. Rodent and Rabbit Species 7 Animal Handler Health and Safety Program A. Zoonotic Disease: Most zoonotic threats from rodents come from wild caught species used for research, the use of contaminated rodent products or from feral rodents gaining access to research animals. Table 1 lists some prevalent pathogens that are transmissible from rodent and rabbit species to humans that can be of concern. The two most common zoonotic pathogens associated with rodents are Lymphocytic Choriomeningitis virus and Hantavirus. B. Allergy: Allergic skin and respiratory reactions are quite common in personnel working with laboratory animals. Hypersensitivity reactions to animal allergens are serious occupational health problems that develop in many individuals after repeated exposure. Hypersensitivity reactions include nasal congestion, runny nose, sneezing, itching of the eyes, asthma and a variety of skin manifestations such as redness, localized itching and flaking skin, and hives. Of the species used in biomedical research, the guinea pig, rabbit, mouse and rat appear to be the most allergenic. Urinary and salivary proteins from the animal’s fur, bedding, and caging are known sources of allergens. Methods of prevention involve using engineering controls, administrative controls, and PPE. In practice this will include reduction of direct animal contact time, use of biological safety cabinets, filter tops on animal cages, ventilated caging rack systems, HEPA filtered bedding dump stations, and protective clothing, surgical masks, or respirators when working with these species. C. Wounds: Training in proper handling and restraint of rabbits and rodents is the single most effective measure in protecting personnel from bites and scratches from these species. Bite protection gloves can be helpful when working with fractious rodent species, and wearing long sleeves while handling rabbits can help in avoiding scratches D. Protective Measures. Table 2 outlines recommendations for specific activities associated with different risks of exposure from rodent and rabbit species. 13. Carnivore Species A. Zoonoses: The most commonly used carnivore used at University laboratories is the ferret. Rabies is the most significant zoonotic disease associated with carnivores and is typically transmitted through bites and scratches and rarely by fomites (inanimate objects). A number of parasitic organisms are also of concern. Even though research animals go through a specific quarantine process, because they may be from random sources, they can still contract and harbor certain zoonotic diseases. In addition, personnel who work with carnivores must be aware that they can serve as vectors for the transmission of infectious agents between their own animals and the same or similar species that they support at UMCP. Table 3 lists some prevalent pathogens transmissible from carnivores to humans that can be of concern. 8 Animal Handler Health and Safety Program B. Allergies. Allergies to ferrets can occur and may sensitize workers to other lab species such as mice and rats. Allergies are most commonly thought of with regards to cats whose major allergy proteins are in the sebaceous glands of the skin that coat oil on the hair shaft and in their saliva. Allergic reactions to cats can come from contact with the fur or aerosolization/inhalation of the proteins. Methods of prevention include reduction in contact with the fur of cats (i.e. avoidance, or full coverage of arms and hands), and possibly the use of a surgical mask if aerosol contact is a potential (i.e. spraying down cages or runs). C. Wounds. Besides rabies, bites and scratches from all carnivores, but especially cats, are often associated with bacterial infections that can cause significant morbidity, and rarely, mortality. All facilities should have appropriate standard operating procedures for first aid of wounds. D. Protective Measures. Table 4 outlines recommendations for specific activities associated with different risks of exposure from carnivore species. 14. Ungulate Species A. Zoonotic Disease. Zoonotic diseases associated with ungulate holding facilities are usually limited when the animals are kept in closed herds with proper vaccination and herd health programs. However, if they are kept in outdoor housing areas, they can still acquire and harbor certain zoonotic diseases. Of particular concern is the rickettsial disease caused by Coxiella burnetii, commonly known as Q Fever which can be found in sheep, goats and cattle, but is most prevalent in sheep. Q fever has a high infection rate throughout the US. Individuals at risk of exposure to Q-fever include those who handle or use products of parturition or material contaminated by them (i.e., placenta, amniotic fluid, blood or bedding) from sheep, cattle or cats; and/or individuals with valvular or congenital heart defects, vascular grafts and those who are immunosuppressed. These individuals are advised of the potential risks involved and medical clearance for duty will be determined on a case-by-case basis by the medical provider. Characteristics of infection with Coxiella burnettii: 1. The incubation period averages 20 days, with a range of 14-39 days. 2. Signs and symptoms of acute infection include the sudden onset of severe headache, fever of 104o F or greater, chills and myalgias. The patient may present with pneumonitis or clinical hepatitis. Treatment is initiated as soon as diagnosis is suspected. 3. Serologic confirmation of the diagnosis is accomplished three months later using enzyme immunoassay (EIA) testing of serum samples obtained at the time of initial report, at two weeks and every 30 days from that day for three months. Samples are sent to the Maryland state Health Laboratory. The employee’s work status depends upon the severity of the symptoms. 9 Animal Handler Health and Safety Program Although rare in the US, caution should be used when handling non-fixed neural and ocular tissue from cattle because of the possibility of exposure to prions related to Bovine Spongiform Encephalopathy. Table 5 lists some prevalent pathogens transmissible from ungulates to humans that can be of concern. B. Allergies. Allergies to cattle and horses have been reported, but are much less common than those to small laboratory animals. C. Wounds. Because of the size of these species, injuries from being stepped on, kicked or butted can result from improper handling and restraint. Bite wounds may also occur. Training in proper use of halters, ropes and other restraint equipment is recommended. Wounds occurring when handling ungulates should receive proper and immediate disinfection. D. Protective Measures. Table 6 outlines recommendations for specific activities associated with different risks of exposure to ungulate species. 15. Fish, Reptiles and Amphibians A. Zoonotic Disease. Zoonotic diseases associated with fish, reptile and amphibian research holding facilities are infrequent in incidence, but can occur. Table 7 lists some prevalent pathogens transmissible from fish and frog species to humans that can be of concern. B. Allergy. Aerosolized fish proteins can be a source of allergic reactions for people and symptoms can range from allergic rhinitis to asthma. There are also reports of occasional reactions to frog skin and secretions that range from cutaneous to respiratory signs. C. Protective Measures. Table 8 outlines recommendations for activities associated with fish and frog species. 16. Bats A. Zoonoses. Although relatively rare, rabies is the most significant zoonotic disease associated with bats and is typically transmitted through bites and scratches. Aerosolization of the virus in feces is possible, though transmission to humans is rare. When housed indoors, contact with other pathogens is unlikely. Wild- caught animals, however, can still harbor zoonotic pathogens. Vaccination against rabies is common practice, but vaccines are not approved for bats and 100% protection is unlikely. Table 9 lists some prevalent pathogens transmissible from bats to humans that can be of concern. B. Wounds. Besides rabies, bites and scratches from bats may be associated with bacterial infections that can cause significant morbidity. Facilities should have appropriate standard operating procedures for first aid of wounds. 10 Animal Handler Health and Safety Program C. Protective Measures. Table 10 outlines recommendations for specific activities associated with different risks of exposure from bats. 17. Birds A. Zoonotic Disease. Birds housed at the University include chickens, turkeys, quail, ducks, pheasants, pigeons, budgies, lorikeets, canaries, finches and owls. Zoonotic diseases associated with birds are infrequent in incidence, but can occur. Birds are the main reservoir for human infections of Chlamydial disease. Salmonella is also relatively common. Table 11 lists some prevalent pathogens transmissible from avian species to humans that can be of concern. B. Allergy. Aerosolized feather dander can be a source of allergic reactions for people and symptoms can range from allergic rhinitis to asthma. C. Wounds. Training in proper handling and restraint of birds is the single most effective measure in protecting personnel from bites and scratches from these species. Bite protection gloves can be helpful when working with fractious species. D. Protective measures. Table 12 outlines recommendations for activities associated with different risks of exposure from birds. Bite protection gloves are required when handling birds of prey. 11 Animal Handler Health and Safety Program Table 1 - Prevalent Zoonotic Diseases of Rodents and Rabbits Zoonosis Agent Species Routes of Transmission Bites, fecal-oral (S. moniliformis) Bites (S. minus) Aerosol, bites, direct contact, fecal-oral Streptobacillus moniliformes Spririllum minus LCM virus Rodents Hantavirus pulmonary syndrome Hantavirus Rodents Aerosol Cheyletiellosis Cheletiella parasitovorax Trichophyton sp. Misrosporum sp. Hymenolepsis nana Rabbits Direct contact Rodents/Rabbits Direct contact, fomites Fecal-oral Rat Bite Fever Lymphocytic Choriomeningitis Ringworm Tapeworm Rodents Rodents Table 2 – Protective Clothing Requirements for Personnel in Rodent and Rabbit Facilities Activity Enter animal holding room (conventional, microisolator or ventilated rack) for brief visual inspection Enter animal holding room (conventional, microisolator or ventilated rack) for any reason. Animals maintained pathogen free. Contact with primary enclosures Direct contact with animals Cage cleaning or change out Harvesting tissues from animals in procedure room or lab Requirements (Hand washing should be performed upon leaving all animal facilities) Street clothes covering or uniform Uniform covering or street clothing covering; gloves; mask; shoe covers (even when wearing dedicated shoes); head cover Street clothes covering or uniform Street clothes covering or uniform; exam gloves; Masks recommended to minimize allergen exposure as needed. Street clothes covering or uniform; exam gloves; masks and eye protection appropriate for the risk of exposure to allergens and chemical agents Street clothes covering or uniform (scrub top is acceptable); exam gloves 12 Animal Handler Health and Safety Program Table 3 - Prevalent Zoonotic Diseases of Carnivores Zoonosis Agent Species Capnocytophaga canimorsus Bartonella henselae (cat scratch fever) Pasturella multocida Rabies virus (Lyssavirus) Bite and scratch bacterial agents Rabies Dematomycoses (Ringworm) Microsporum sp. Trichophyton sp. Acariasis Sarcoptes scabei Cat, Ferret Cat Car, Ferret Cat, Ferret Cat, Routes of Transmission Direct contact Bite Scratch Bite, scratch, fomite Contact with saliva, brain Direct contact, fomite Ferret Cat, Ferret Direct contact Table 4 – Protective Clothing Requirements for Personnel in Carnivore Facilities Activity Requirements (Hand washing should be performed upon leaving all animal facilities) Street clothes covering or uniform Street clothes covering or uniform; dedicated shoes or shoe covers; exam gloves; and mucous membrane protection as appropriate Street clothes covering or uniform; exam gloves for clinical procedures: exam gloves may not be required for general handling or enrichment Street clothes may be worn; exam gloves when handling prosthetics Enter into animal runs or pens Cleaning procedures for caging Direct contact with animals in animal facilities Direct contact with animals in labs Table 5 - Prevalent Zoonotic Diseases of Ungulates Zoonosis Q Fever Coxiella burnetti Sheep, Cattle, Goats Tuberculosis Mycobacterium bovis, avium or tuberculosis Pox virus Sheep, Cattle, swine Routes of Transmission Aerosol or direct contact; especially when dealing with birth products Aerosol or direct contact Sheep, Goats Direct contact Campylobacter jejuni Cattle, Swine, Sheep Cattle, Sheep, Goats, Swine Fecal/oral Contageous Ecthyma (Orf) Campylobacteriosis Dermatomycoses (Ringworm) Agent Species Trichophyton or Microsporum spp. 13 Direct contact Animal Handler Health and Safety Program Bovine Spongiform Encephalopathy Prion Cattle Direct blood/tissue contact with infected tissue or contaminated material Table 6 – Protective Clothing Requirements for Personnel in Ungulate Facilities Activity Requirements (Hand washing should be performed upon leaving all animal facilities) Street clothes may be worn Entry into indoor or outdoor animal holding areas Direct contact with animals Street clothes covering or uniform; exam gloves for clinical procedures; exam gloves may not be required for socialization or enrichment procedures Uniform or street clothes covering; exam or other protective gloves. Dedicated shoes or rubber work boots are recommended. Mucous membrane protection should be used as is appropriate. Uniform or street clothes covering; exam gloves and mucous membrane protection. Dedicated shoes or rubber work boots are recommended Cleaning animal holding areas (indoor or outdoor) Contact with pregnant sheep\goats\cattle; during parturition, their birth products, bedding and other wastes Table 7 - Prevalent Zoonotic Diseases of Fish, Amphibians & Reptiles Zoonosis Agent Species Mycobacterium xenopi, fortuitum, marinum, chelonei Salmonella spp. Vibrio vulnificus Mycobacteriosis Salmonellosis Vibriosis Fish, Frogs Routes of Transmission Breaks in skin surface Frogs Fish Breaks in skin surface Breaks in skin surface Table 8 – Protective Clothing Requirements for Personnel in Fish, Amphibians & Reptiles Activity Direct handling of fish Direct handling of frogs Placing hands into the water for husbandry, feeding, manipulating, etc. Requirements (Hand washing should be performed upon leaving all animal facilities) Exam gloves suggested; hand sanitizing necessary if gloves are not worn Exam gloves suggested; hand sanitizing necessary if gloves are not worn Exam gloves suggested; hand sanitizing necessary if gloves are not worn 14 Animal Handler Health and Safety Program Table 9 - Prevalent Zoonotic Diseases of Bats Zoonosis Agent Rabies virus (Lyssa virus) Rabies Route of Transmission Bites Scratches Aerosol (rare) Table 10 – Protective Clothing Requirements for Personnel in Bat Facilities Activity Requirements (Hand washing should be performed upon leaving all animal facilities) Street clothes may be worn Enter animal holding room for brief visual inspection Contact with outside of primary enclosures Street clothes covering or uniform; exam gloves Street clothes covering or uniform; shoe covers; exam gloves; head cover and mucous membrane protection Street clothes covering or uniform; exam gloves; bite protective gloves as needed. Cleaning flight cages Direct contact with animals Table 11 - Prevalent Zoonotic Diseases of Birds Zoonosis Agent Species Psitticosis Chlamydia psittaci Salmonellosis Salmonella sp. All Pasteurellosis Listeriosis Pasteurella multocida Listeria monocytogenes All All Budgies Routes of Transmission Aerosol Direct contact Aerosol, bites, direct contact, fecal-oral Aerosol Direct contact Table 12 – Protective Clothing Requirements for Personnel in Bird Facilities Activity Enter animal holding room for brief visual inspection Contact with outside of primary enclosures Requirements (Hand washing should be performed upon leaving all animal facilities) Street clothes may be worn Street clothes or street clothes covering or uniform; exam gloves 15 Animal Handler Health and Safety Program Cleaning flight cages Direct contact with animals Street clothes covering or uniform; shoe covers; exam gloves; head cover; and mucous membrane protection as appropriate Street clothes or street clothes covering or uniform; exam gloves; bite protection gloves for birds of prey 16