WM Introduction Version 1.2
advertisement
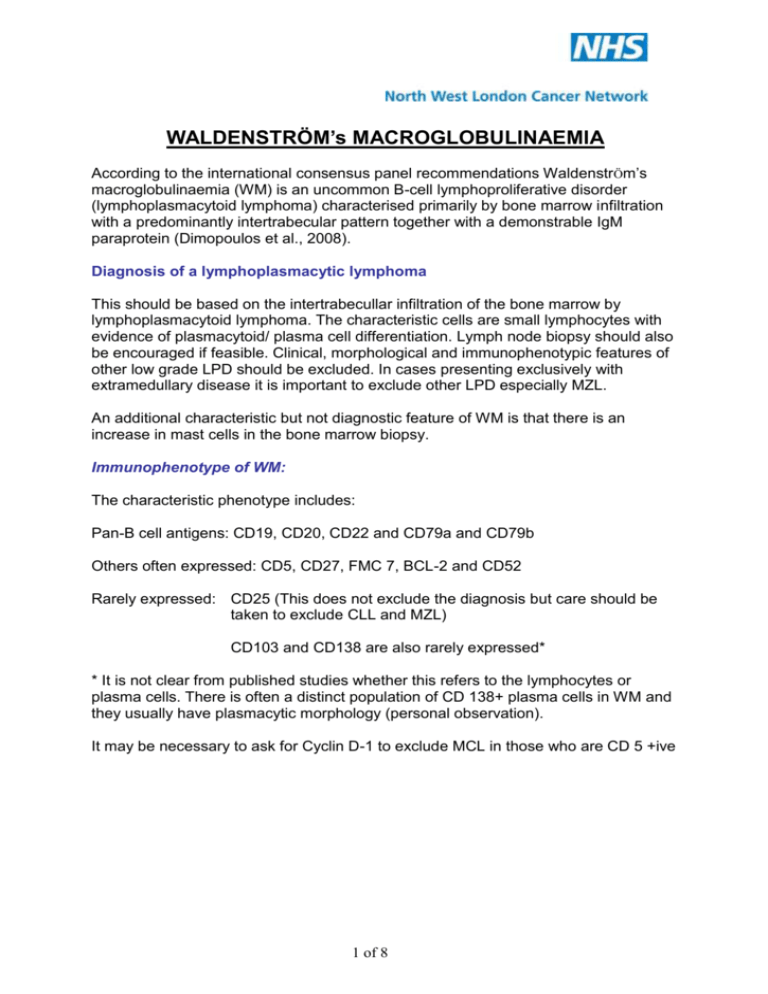
WALDENSTRÖM’s MACROGLOBULINAEMIA According to the international consensus panel recommendations Waldenstr Öm’s macroglobulinaemia (WM) is an uncommon B-cell lymphoproliferative disorder (lymphoplasmacytoid lymphoma) characterised primarily by bone marrow infiltration with a predominantly intertrabecular pattern together with a demonstrable IgM paraprotein (Dimopoulos et al., 2008). Diagnosis of a lymphoplasmacytic lymphoma This should be based on the intertrabecullar infiltration of the bone marrow by lymphoplasmacytoid lymphoma. The characteristic cells are small lymphocytes with evidence of plasmacytoid/ plasma cell differentiation. Lymph node biopsy should also be encouraged if feasible. Clinical, morphological and immunophenotypic features of other low grade LPD should be excluded. In cases presenting exclusively with extramedullary disease it is important to exclude other LPD especially MZL. An additional characteristic but not diagnostic feature of WM is that there is an increase in mast cells in the bone marrow biopsy. Immunophenotype of WM: The characteristic phenotype includes: Pan-B cell antigens: CD19, CD20, CD22 and CD79a and CD79b Others often expressed: CD5, CD27, FMC 7, BCL-2 and CD52 Rarely expressed: CD25 (This does not exclude the diagnosis but care should be taken to exclude CLL and MZL) CD103 and CD138 are also rarely expressed* * It is not clear from published studies whether this refers to the lymphocytes or plasma cells. There is often a distinct population of CD 138+ plasma cells in WM and they usually have plasmacytic morphology (personal observation). It may be necessary to ask for Cyclin D-1 to exclude MCL in those who are CD 5 +ive 1 of 8 Distinction between asymptomatic WM, symptomatic WM, MGUS and other IgM related disorders There are four subtypes of LPL with IgM paraproteinaemias that are proposed by the workshop. These are: Asymptomatic Waldenström’s macroglobulinaemia. These patients have a clear infiltration by LPL, an IgM paraprotein of any level but without symptoms either attributable to BM infiltration or to the IgM paraprotein. Symptomatic WM: These patients have a clear infiltration by LPL, an IgM paraprotein of any level and symptoms either attributable to BM infiltration, organomegaly, constitutional symptoms or to the IgM paraprotein (hyperviscosity, neuropathy, cold agglutinins, amyloidosis or cryoglobulinaemia). IgM MGUS: Those with an IgM paraprotein but without demonstrable confirmed BM infiltration by LPL. The level of PP is not important but is rarely above 30g/L. Other IgM related disorders: this is a proposed category that includes patients with an IgM paraprotein but without a demonstrable LPL, and who have symptoms attributable to the paraproteinaemia. These include symptomatic autoimmune phenomena, neuropathy, cold agglutinins, amyloidosis or cryoglobulinaemia. Differential diagnosis of other lymphoproliferative disorders secreting IgM 1. IgM myeloma: the morphology of the bone marrow infiltrate is predomiantly plasmacytic and there are lytic lesions. 2. Splenic marginal zone lymphoma (SMZL): strong expression of CD 22 and CD11c. CD25 more commonly expressed in WM. Cytogenetics: 7q-, +3q and +5 in SMZL 3. Mantle cell lymphoma: cells have irregular nuclei, involvement of lymph nodes and extranodal sites and spleen. T(11;14) ( q13;q32) 4. B CLL: morphology of cells. Expression of CD5 and CD23 Cytogenetics The deletions of the long arm of chromosome 6 (6q deletions) is the only recurrent abnormality found in approximately 50% of cases. No illegitimate recombinations of the heavy chain locus on chromosome 14 have been found. Investigations at outset: Laboratory tests FBC blood film and reticulocytes LFT, creatinine and electrolytes Immunoglobulin quantitation Paraprotein quantitation BJP Serum free light chains 2 of 8 Beta 2 microglobulin Consider Cryoglobulins Direct antiglobulin test Antibody screen In case of neuropathy anti MAG antibodies. Consider anti ganglioside and sulphatides. Consider plasma viscosity if there is clinical suspicion of hyperviscosity Other tests Imaging: CT scan of chest and abdomen is only needed as a baseline before treatment or only if it will influence decision to treat. Nerve conduction studies in cases of neuropathy. Prognostic factors: The median survival of patients with WM is 5 years but 20% of patients survive more than 10 years and 10-20% may die of unrelated caused. There are few studies that have defined the prognostic factors in WM. The most relevant prognostic factors affecting survival beta 2 microglobulin, Hb, Albumin and age. With these simple parameters, patients were stratified into three groups at low, intermediate and high risk of death, with 5-year survival probabilities of 92%, 63%, and 27%, respectively. In the SWOG study, a serum beta-2 microglobulin level higher than 3 mg/L, a hemoglobin level below 12 g/dL, and a serum IgM level above 40 g/L were significant adverse prognostic factors for survival. A staging system using these variables identified four distinct subsets of patients with estimated 5-year survival rates of 87%, 64%, 53%, and 12%. Response to treatment has also been found to be associated with better survival. The International prognostic scoring system (IPSS) for WM recognised 5 adverse covariates. (Morel et al Blood on Line Feb 5th 2009) Age >65 years Haemoglobin ≤11.5 g/dL Platelet count ≤100 x109/L Beta2-microglobulin >3 mg/L Monoclonal IgM conc. >70 g/L Category % patients No of factors Low risk 27% ≤1 factor Intermediate risk 38% 2 or age >65 High risk 35% ≥2 5 year survival 87% 68 % 36% Initiation of therapy appropriate in patients with: Rising paraproteins and progressive symptoms of disease. Hb <10g/dL, or platelets of <100 x109/L attributable to disease Bulky disease or related constitutional symptoms Hyperviscosity 3 of 8 Evidence of disease transformation Symptoms related to the paraprotein such as symptomatic polyneuropathy, cold agglutinins, amyloidosis, nephropathy, autoimmune phenomena and symptomatic cryoglobulinaemia. Follow up of asymptomatic patients: Asymptomatic WM every 3-6 months MGUS every 6-12 months. Recommendations for treatment (International Working Group) There are a variety of drugs and combinations which have been used successfully for the treatment of WM. However there are no comparative controlled trials of any therapy against others and this will therefore be reflected in the levels of recommendations. The table below taken from Dimopoulous et al 2008 (J Clin Oncol. 27:120-126) sets out the treatment options for first line therapy and the level of evidence and recommendation. The choice of therapy should take into account the individual patient’s circumstances. For example it is advisable to avoid using alkylating agents and probably also nucleoside analogues in younger patients in whom PBSCT may be considered as these drugs may reduce the ability to harvest PBSC. Another consideration is the leukaemogenic potential of these drugs in younger patients. 4 of 8 Recommendations from the international expert panel are that autologous autografts may be used in younger patients after relapse. It is also recommended that allogeneic transplants should only be considered in the context of clinical trials. Addition of rituximab to other agents may produce a more complete and quicker response. However a ‘flare’ reaction may occur whereby there is an increase of paraprotein prior to its reduction. Special conditions: Salvage/ Relapse Therapy The choice of salvage therapy depends on the first-line treatment used, the quality and duration of response, and other variables such as age, tolerance of initial therapy, and suitability for stem-cell transplantation. If the original response was prolonged to more than 12 months unmaintained, the initially effective treatment should be considered if well tolerated. If relapse occurred in a shorter period of time, use of an alternate single agent or combination is recommended. For patients who have short remissions or resistance to a first-line regimen, second-line treatment may include agents of a different class either alone or in combination. In that setting, the R-FC regimen may be appropriate, although it should be avoided in younger patients and patients who are eligible for ASCT in whom stem cells have not previously been collected and stored. Bortezomib-based therapy may also be an appropriate second-line choice. 5 of 8 In view of recent data on the activity of alemtuzumab in pretreated patients, this agent may represent a reasonable third-line therapy. The place of high-dose therapy with ASCT or alloSCT requires further evaluation in the context of prospective trials, which should focus primarily on patients with highrisk disease or on an individual basis in selected young patients with high risk disease. Based on the International Working Group recommendations the following protocols are recommended within NWLCN: Protocols: 2.01 2.03 Chlorambucil Suitable for elderly patients Caution with frail patients and renal impairment Rituximab Suitable for frail patients and patients with co-morbidities Caution in patients with high paraprotein levels 6 of 8 2.05 Fludarabine Suitable for younger or fitter patients Caution: can produce prolonged cytopenias 2.27 Rituximab-Fludarabine 2.06 Fludarabine - Cyclophosphamide 6.01 R-FC 6.02 DRC 2.07 Transplantation candidate: cytopenias and high M-protein Non-transplantation candidate: cytopenias R-CHOP Transplantation candidate: high M-protein or Non-transplantation candidate: cytopenias only 2.24 R-CVP 3.10 Thalidomide ± Dexamethasone 6.03 R-Thalidomide Patients with cytopenias, transplant or non-transplant candidates 7 of 8 Summary of updated response criteria from the 3rd International Workshop on Waldenstöm’s Macroglobulinemia Response Complete response (CR) Partial response (PR) Stable disease (SD) Criteria Disappearance of monoclonal protein by immunofixation; no histologic evidence of bone marrow involvement, resolution of any adenopathy/ organomegaly (confirmed by CT scan), or signs or symptoms attributable to WM. Reconfirmation of the CR status is required at least 6 weeks apart with a second immunofixation. At least 50% reduction of serum monoclonal IgM concentration on protein electrophoresis and at least 50% decrease in adenopathy/organomegaly on physical examination or on CT scan. No new symptoms or signs of active disease. Minor response (MR) At least 25% but less than 50% reduction of serum monoclonal IgM by protein electrophoresis. No new symptoms or signs of active disease. A less-than-25% reduction and less-than-25% increase of serum monoclonal IgM by electrophoresis without progression of adenopathy/organomegaly, cytopenias, or clinically significant symptoms due to disease and/or signs of WM. Progressive disease (PD) At least 25% increase in serum monoclonal IgM by protein electrophoresis confirmed by a second measurement or progression of clinically significant findings due to disease (ie, anemia, thrombocytopenia, leukopenia, bulky adenopathy/organomegaly) or symptoms (unexplained recurrent fever of at least 38.4°C, drenching night sweats, References Dimopoulous MA, Gertz MA, Kastritis E, et al. Update on Treatment Recommendatinos from the fourth International Workshop on Waldenström’s Macroglobulinaemia, J Clin Oncol. 27:120-126, 2008 Written by: Dr Saad Abdalla, Dr Amin Rahemtulla, Dr Stephanie Kirschke, August 2009 Authorised by: NWLCN Haematology TWG , March 2010, Date for review by Haematology TWG: March 2011 8 of 8


![[4-20-14]](http://s3.studylib.net/store/data/007235994_1-0faee5e1e8e40d0ff5b181c9dc01d48d-300x300.png)