USMLE Step 1 Web Prep — Failures of the Immune System
advertisement
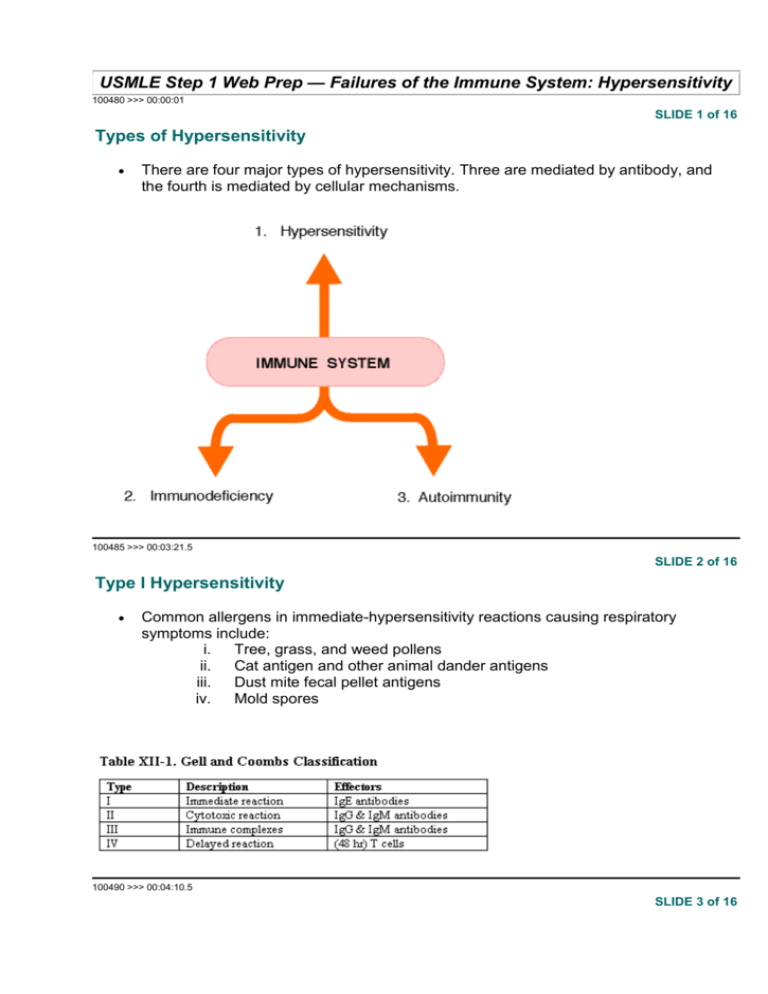
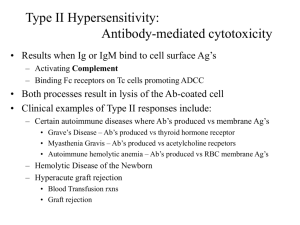
USMLE Step 1 Web Prep — Failures of the Immune System: Hypersensitivity 100480 >>> 00:00:01 SLIDE 1 of 16 Types of Hypersensitivity There are four major types of hypersensitivity. Three are mediated by antibody, and the fourth is mediated by cellular mechanisms. 100485 >>> 00:03:21.5 SLIDE 2 of 16 Type I Hypersensitivity Common allergens in immediate-hypersensitivity reactions causing respiratory symptoms include: i. Tree, grass, and weed pollens ii. Cat antigen and other animal dander antigens iii. Dust mite fecal pellet antigens iv. Mold spores 100490 >>> 00:04:10.5 SLIDE 3 of 16 In a Nutshell: Type I Immediate Reaction Hypersensitivity First exposure sensitizes host Macrophages and B cells present epitopes to Th2 cells, which produce interleukin (IL)-4 IL-4 causes class switch to IgE Mast cells and basophils bind IgE to high-affinity receptors IgE cross-linking initiates granule release These granules contain histamine, heparin, and proteases that induce edema, increased mucus secretion, and smooth muscle contraction; this is the immediate reaction that occurs The cells also synthesize prostaglandins and leukotrienes LTC4 and LTD4, which mediate the late-phase (4-6 hours later) inflammatory response 100500 >>> 00:07:06.5 SLIDE 4 of 16 100505 >>> 00:08:31.5 SLIDE 5 of 16 Clinical Correlate: Diagnosis of Atopic Disease In vivo skin testing with batteries of allergens In vitro RAST test (quantitate specific IgE levels) 100510 >>> 00:11:44.5 SLIDE 6 of 16 Therapies for immediate hypersensitivities Avoidance Antihistamine (Benadryl) Cromolyn sodium Epinephrine Theophylline (xanthines) Immunotherapy by injecting small amounts of allergen Corticosteroids -Adrenergic agonists 100515 >>> 00:16:12.5 SLIDE 7 of 16 Cytotoxic Type II Hypersensitivity Antibody-mediated hypersensitivity against our own cells or receptors or membranes Type II or cytotoxic hypersensitivity is mediated by IgG or IgM antibodies against tissue antigens. The result is organ-specific antibody production. Antibody binds to cells or tissues and causes local complement activation, influx of leukocytes, and tissue destruction because of ADCC, degranulation by phagocytes, and production of oxygen radicals. An example is hemolytic disease of the newborn. 100520 >>> 00:20:06.5 SLIDE 8 of 16 Noncytotoxic Type II Hypersensitivity Also due to the production of tissue-specific IgG autoantibody. Instead of causing cytotoxic tissue destruction, the antibody in these cases alters cellular structure or function An example is Graves’ disease 100525 >>> 00:21:32.5 SLIDE 9 of 16 Other examples of type II hypersensitivity Myasthenia gravis: An autoantibody against the patient’s own acetylcholine receptors in which the antibody removes and internalizes the receptors. 100530 >>> 00:22:01.5 SLIDE 10 of 16 Clinical Correlate: Cytotoxic Antibody Disease Erythroblastosis fetalis Transfusion reactions Hyperacute graft rejection Acquired hemolytic anemia: autoimmune, drug-induced 100535 >>> 00:22:25.5 SLIDE 11 of 16 Other examples of type II hypersensitivity Goodpasture syndrome: An autoantibody produced against the patient’s own type IV collagen present in basement membranes of kidney and lung. Autoimmune hemolytic anemia: An autoantibody produced against the patient’s own red blood cell antigens (eg. I antigen). Autoimmune thrombocytopenic purpura: An autoantibody produced against the patient’s own platelet integrin. Hyperacute graft rejection: The recipient of a graft already has preformed antibody against the graft; after receiving the graft it is rejected within hours. 100545 >>> 00:23:38.5 SLIDE 12 of 16 Clinical Correlate: Therapy for Type II (and III) Hypersensitivities Withhold allergenic drug Remove antibodies i. Exchange transfusion ii. Plasmapheresis Use immunosuppressive agents: i. Corticosteroids ii. Cytoxan iii. Cyclosporin A 100550 >>> 00:24:08.5 SLIDE 13 of 16 Type III: Immune complex hypersensitivity Caused by high levels of circulating, soluble immune complexes containing IgG or IgM antibody. Circulating immune complexes overwhelm the ability of the mononuclear phagocyte system to remove them and deposit in various tissues (eg. skin, glomeruli, blood vessels, synovium, lungs) and activate complement. 100555 >>> 00:25:16.5 SLIDE 14 of 16 Examples of type III hypersensitivity immune complex diseases Arthus reaction Serum sickness Hypersensitivity pneumonitis Post-streptococcal glomerulonephritis Lupus Rheumatoid arthritis Certain infectious diseases, eg. hepatitis B, HIV, and mycobacterium 100560 >>> 00:26:30.5 SLIDE 15 of 16 Type IV: Delayed-type hypersensitivity (DTH) T-cell-mediated response that gets its name from the long time (48-96 hours) that it takes for a skin reaction against the antigen to develop. Th1 cells recognize the antigenic peptide presented by an antigen-presenting cell and secrete cytokines (interferon-) that activate macrophages. Macrophage mediators then produce the damage in tissues. Antibody and complement play no role in DTH. Antigens may be intracellular bacterial pathogens (Mycobacterium tuberculosis, Mycobacterium leprae), viruses, fungi, or intracellular parasites; they also may be environmental antigens (eg. poison ivy and nickel) that bind to, and alter, host cell surfaces, resulting in contact dermatitis. 100565 >>> 00:28:09.5 SLIDE 16 of 16 Common contact allergens Poison ivy (catechols) Nickel Formaldehyde Latex Chromium Dyes in clothing and cosmetics