The newborn baby with a murmur
advertisement
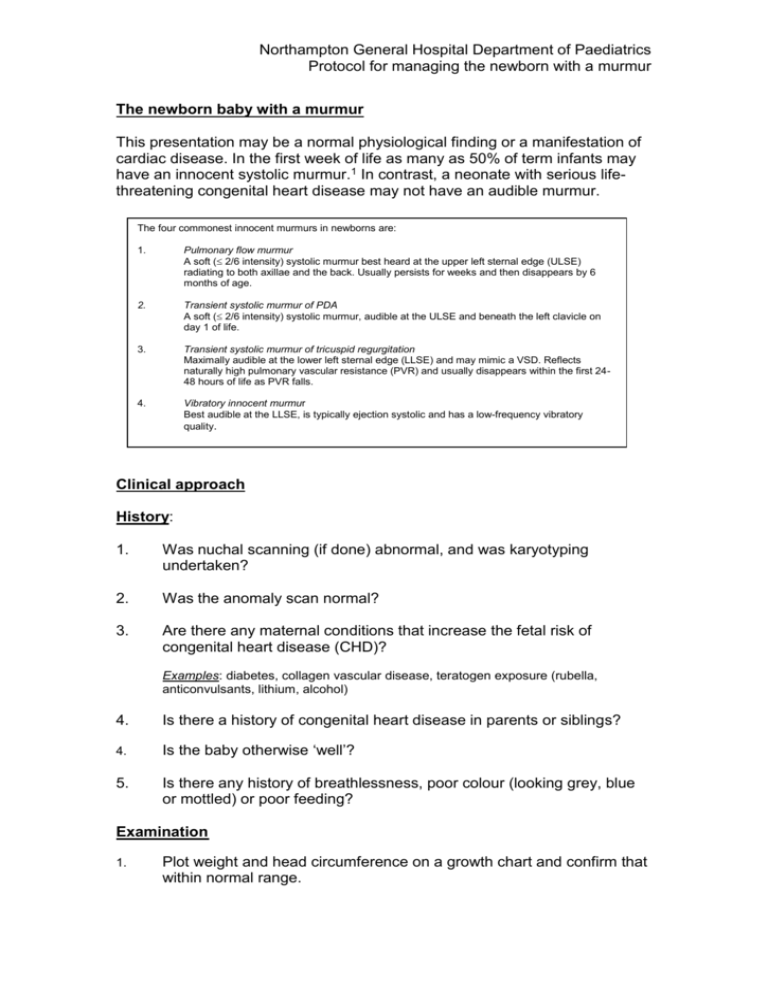
Northampton General Hospital Department of Paediatrics Protocol for managing the newborn with a murmur The newborn baby with a murmur This presentation may be a normal physiological finding or a manifestation of cardiac disease. In the first week of life as many as 50% of term infants may have an innocent systolic murmur.1 In contrast, a neonate with serious lifethreatening congenital heart disease may not have an audible murmur. The four commonest innocent murmurs in newborns are: 1. Pulmonary flow murmur A soft ( 2/6 intensity) systolic murmur best heard at the upper left sternal edge (ULSE) radiating to both axillae and the back. Usually persists for weeks and then disappears by 6 months of age. 2. Transient systolic murmur of PDA A soft ( 2/6 intensity) systolic murmur, audible at the ULSE and beneath the left clavicle on day 1 of life. 3. Transient systolic murmur of tricuspid regurgitation Maximally audible at the lower left sternal edge (LLSE) and may mimic a VSD. Reflects naturally high pulmonary vascular resistance (PVR) and usually disappears within the first 2448 hours of life as PVR falls. 4. Vibratory innocent murmur Best audible at the LLSE, is typically ejection systolic and has a low-frequency vibratory quality. Clinical approach History: 1. Was nuchal scanning (if done) abnormal, and was karyotyping undertaken? 2. Was the anomaly scan normal? 3. Are there any maternal conditions that increase the fetal risk of congenital heart disease (CHD)? Examples: diabetes, collagen vascular disease, teratogen exposure (rubella, anticonvulsants, lithium, alcohol) 4. Is there a history of congenital heart disease in parents or siblings? 4. Is the baby otherwise ‘well’? 5. Is there any history of breathlessness, poor colour (looking grey, blue or mottled) or poor feeding? Examination 1. Plot weight and head circumference on a growth chart and confirm that within normal range. Northampton General Hospital Department of Paediatrics Protocol for managing the newborn with a murmur 2. Does the baby look dysmorphic? 3. Confirm that both brachial and both femoral pulses are palpable. Confirm that there is no difference in strength of pulse when comparing right brachial pulse with the other three pulses, or when comparing the brachial pulses with femoral pulses. 4. Record blood pressure in both arms and 1 leg. Normal systolic blood pressure in a settled term baby is between 60-80mmHg.There should not be a difference of more than 20mmHg between the arms and the selected leg, or when comparing the blood pressure in each arm. 5. Look clinically for cyanosis and measure pulse oximetry in both arms and one leg. Normal oxygen saturations are at least 95% in all limbs. 6. Record heart rate and respiratory rate with baby awake and settled. Normal heart rate 100-140* Normal respiratory rate 1st 48 hours After 48 hours 40-60 40 *Resting heart rate in a normal sleeping term neonate may fall to as low as 85. Of no concern provided otherwise completely well, examination normal and ECG demonstrates sinus rhythm. 7. Precordial and suprasternal palpation a. Confirm that the apex beat is left-sided and situated around the 5th intercostal space in the mid-clavicular line. b. Ensure that there is no thrill palpable anywhere over the precordium. If present, document where best felt. 8. For the murmur, record the following: a. Whether heard in systole, diastole or in both phases of the cardiac cycle. If you are uncertain, listen whilst palpating brachial pulse (murmur with pulse is systolic, after pulse is diastolic). b. Intensity (Grade 1-4) Grade 1 Grade 2 Grade 3 Grade 4 Barely audible Soft, but easily audible Moderately loud but not associated with a thrill Louder and associated with a thrill c. Where heard loudest and where it radiates to Northampton General Hospital Department of Paediatrics Protocol for managing the newborn with a murmur Assess the ‘work of breathing’ with the baby settled. Ensure that it looks ‘comfortable’ and that none of the following are present: 9. Grunting Tracheal tug Subcostal or intercostal recession 10. Listen to the lung fields and ensure that the breath sounds are vesicular. 11. Palpate the abdomen and ensure that you can palpate no more than just the leading edge of the liver 1cm beneath the right costal margin. Initial investigations Note: In an unwell baby with a murmur investigation should be deferred until a senior clinician (StR grade or consultant) has reviewed the baby and confirmed that no immediate medical intervention is required. 1. ECG should be done in all. If the infant is otherwise perfectly well, (in particular, has normal pulses and is not breathless or cyanosed) he/she can go to the department of cardiology for the ECG technician on duty would prefer such. 2. Indications for chest x-ray: Tachypnoea/elevated work of breathing Oxygen saturations <95% Clinical suggestion of dextrocardia Northampton General Hospital Department of Paediatrics Protocol for managing the newborn with a murmur Murmur ‘Well’ baby Unwell baby Senior opinion immediately Resuscitate Admit to Gosset ward Inform Gosset ward consultant Consider cardiology opinion Consider need for echocardiogram Pre-discharge echocardiogram not indicated provided: Pre-discharge echocardiogram mandatory if: History unremarkable (see questions) Murmur intensity 2/6 No difference in upper and lower limb pulses No significant difference in upper/lower limb blood pressure Otherwise normal physical examination Oxygen saturations all limbs 95% Normal ECG Murmur intensity 2/6 Difference in limb pulses Significant difference in limb blood pressures Oxygen saturation < 95% in any limb Dextrocardia or elevated work of breathing Abnormal ECG StR or Consultant concurs with assessment Prompt review by StR Consider pre-discharge echocardiogram if: Murmur + otherwise normal cardiorespiratory examination, but: Abnormal karyotype or anomaly scan Maternal condition associated with CHD CHD in a first-degree relative Dysmorphic baby e.g. Down Syndrome Discuss case with attending consultant Discharge Follow-up options: (confirm with consultant*) 1. Sign and send standard proforma letter to GP, copy of GP letter into set of baby notes, give parents information leaflet and copy of GP letter 2. OPA with attending consultant Discuss with attending Consultant* Arrange in-patient echocardiogram * For infants admitted to Gosset ward, attending consultant is Gosset consultant of the week; for infants never admitted to Gosset ward attending consultant is general paediatric consultant of the week Northampton General Hospital Department of Paediatrics Protocol for managing the newborn with a murmur References 1. 2. 3. 4. 5. Park MK 2002 Manifestations of Cardiac Problems in Newborns. In: Pediatric Cardiology, 4 th edition, Mosby, St Louis. Ainsworth SB, Wyllie JP, Wren C. Prevalence and clinical significance of cardiac murmurs in neonates. Arch Dis Child Fetal Neonatal Ed 1999; 80:F43-F45. Arlettaz R, Archer N, Wilkinson A. Natural history of innocent heart murmurs in newborn babies: controlled echocardiographic study Arch. Dis. Child. Fetal Neonatal Ed., May 1998; 78: F166 - F170. Farrer KFM, Rennie JM. Neonatal murmurs: are senior house officers good enough? Arch. Dis. Child. Fetal Neonatal Ed., Mar 2003; 88: F147 - F151. C Patton and E Hey. How effectively can clinical examination pick up congenital heart disease at birth? Arch. Dis. Child. Fetal Neonatal Ed., Jul 2006; 91: F263 - F267. Written by Date For review Dr Nick Barnes, Consultant Paediatrician May 2008 May 2011