Zager_-_Pediatric_Heart_Murmurs
advertisement
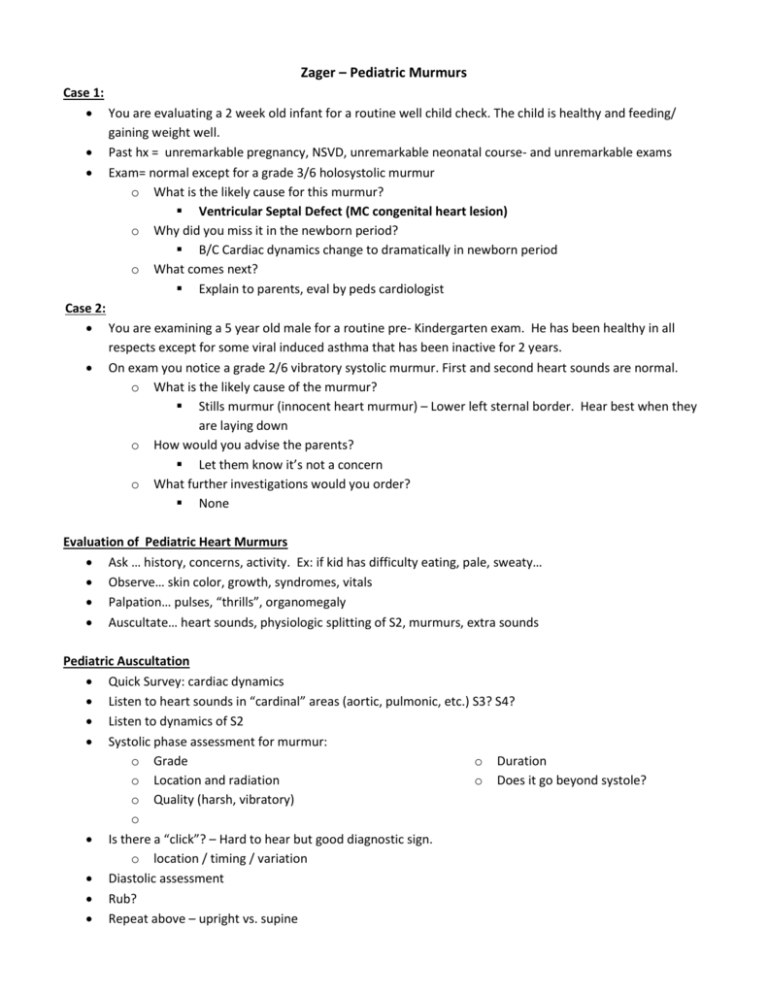
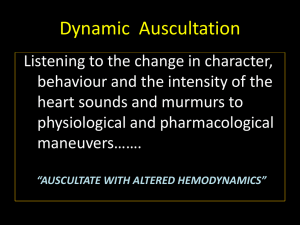
Zager – Pediatric Murmurs Case 1: You are evaluating a 2 week old infant for a routine well child check. The child is healthy and feeding/ gaining weight well. Past hx = unremarkable pregnancy, NSVD, unremarkable neonatal course- and unremarkable exams Exam= normal except for a grade 3/6 holosystolic murmur o What is the likely cause for this murmur? Ventricular Septal Defect (MC congenital heart lesion) o Why did you miss it in the newborn period? B/C Cardiac dynamics change to dramatically in newborn period o What comes next? Explain to parents, eval by peds cardiologist Case 2: You are examining a 5 year old male for a routine pre- Kindergarten exam. He has been healthy in all respects except for some viral induced asthma that has been inactive for 2 years. On exam you notice a grade 2/6 vibratory systolic murmur. First and second heart sounds are normal. o What is the likely cause of the murmur? Stills murmur (innocent heart murmur) – Lower left sternal border. Hear best when they are laying down o How would you advise the parents? Let them know it’s not a concern o What further investigations would you order? None Evaluation of Pediatric Heart Murmurs Ask … history, concerns, activity. Ex: if kid has difficulty eating, pale, sweaty… Observe… skin color, growth, syndromes, vitals Palpation… pulses, “thrills”, organomegaly Auscultate… heart sounds, physiologic splitting of S2, murmurs, extra sounds Pediatric Auscultation Quick Survey: cardiac dynamics Listen to heart sounds in “cardinal” areas (aortic, pulmonic, etc.) S3? S4? Listen to dynamics of S2 Systolic phase assessment for murmur: o Grade o Duration o Location and radiation o Does it go beyond systole? o Quality (harsh, vibratory) o Is there a “click”? – Hard to hear but good diagnostic sign. o location / timing / variation Diastolic assessment Rub? Repeat above – upright vs. supine Innocent Murmurs: Systolic o Still’s murmur: medium pitch, audible from near apex to left sterna boarder. Buzzing, cooing or ‘twangy string’ quality. Early-mid systole o Pulmonic murmur: Vibratory, somewhat rough, L upper sterna border. Short midsystolic o Peripheral pulmonic: vibratory, radiates well to back and axillae, midsystolic. <6mo o Supraclavicular: rough, vibratory, best heard above clavicles and base of neck. Midsystolic Continuous o blowing, louder in diastole, best heard w/ pt sitting. Goes away if compress jugular Characteristics of “Abnormal Murmur” Grade 3 or louder Diastolic “Harsh” in quality Associated with click or abnormal heart sounds Presence of a “thrill” Associated with unusual precordial activity “Big picture” suggests a medical diagnosis commonly associated with congenital heart disease Syndromes- Cardiac Lesions Down – ventricular septal defect, endocardial cushion defect Fetal Alcohol Syndrome- VSD Marfan- aortic root dissection, MVP Noonan- pulmonic stenosis, ASD Turner- coarctation of aorta, bicuspid valve Congenital Rubella- PDA DiGeorge- aortic arch abnormality, Tetralogy of Fallot CATCH 22: Cardiac, Abnl facies, absent Thymus, Cleft Palate, Hypoglycemia The “Problem” Heart Murmur- What to do? Noncardiac studies- chromosomes, CBC, ABG, etc. CXR- might give useful pulmonary info ECG- cardiac dynamics, rhythm ECHOcardiogram- expensive, much variability in quality by technique Referral to Pediatric Cardiologist (often most “cost-effective”) Case 3: A 15 year old male comes as new patient seeking a refill of antihypertensive medications. He was diagnosed with essential hypertension 3 years ago by a pediatrician in another community after extensive studies, including renal imaging, urine catecholamines, and an abdominal CT are negative. Past history is otherwise unremarkable. On exam you find a BP of 158/102. After completing a detailed cardiovascular exam you are able to give the father a definitive diagnosis of his hypertension. He has no heart murmur- what is his diagnosis?