VT106_reproductive
advertisement

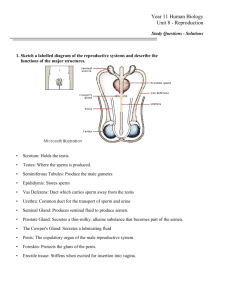
VT 106 Comparative Anatomy and Physiology Reproductive System REPRODUCTIVE SYSTEM Functions of Reproductive System production of offspring – continuation of species genetic recombination – individual variation, adaptation SEXUAL REPRODUCTION gametogenesis – production of gametes (reproductive cells) female – oogenesis produces oocytes (ovum) male – spermatogenesis produces spermatozoa (sperm) copulation – male gametes transmitted to female fertilization – ovum and sperm united gestation – development of offspring from fertilization till birth parturition – giving birth GAMETOGENESIS gonads – site of gamete production female – ovaries male – testes somatic cells – all cells throughout body diploid (2N) – contain pairs of chromosomes (N depends on species) one member of pair from each parent 1 pair of sex chromosomes X chromosome, Y chromosome XX = female XY = male gametes – ovum and sperm haploid (1N) – contain unpaired chromosomes from sire or dam ovum always contains X chromosome sperm – 50% contain X chromosome 50% contain Y chromosome sperm determines sex of offspring zygote – cell produced by fertilization; divides and differentiates into offspring diploid – pairs of chromosomes combined chromosomes from ovum and sperm Mitosis – cell division which produces 2 identical, diploid daughter cells 1 MEIOSIS – 2 stage cell division which produces 4 haploid gametes occurs in gonads gametes produced are not genetically identical to parent cell Stages of Meiosis: meiosis I – a diploid cell divides and forms 2 haploid cells genetic recombination haploid cells randomly receive 1 chromosome from each chromosome pair crossing-over – random exchange of genes between chromosome pairs meiosis II – the 2 haploid cells divide again, forming 4 haploid cells each is genetically unique due to genetic recombination MALE REPRODUCTIVE SYSTEM TESTES – male gonads site of spermatogenesis – production of spermatozoa produce androgens – masculinizing hormones testes develop in abdominal cavity near kidneys normal sperm production requires a temperature below body temperature Descent of the Testes – testes move out of abdomen and into scrotum scrotum – sac of integument and superficial fascia inguinal canals – tunnels through anterior abdominal wall gubernaculum – connective tissue cord that pulls testis through inguinal canal into scrotum spermatic cord – ductus deferens, blood vessels, and nerves running through inguinal canal to testis Regulation of Testicular Temperature vascular heat exchange mechanism cools testes pampiniform plexus (venous network) cools testicular artery cremaster muscle – skeletal muscle in spermatic cord elevates testes close to body when too cold drops testes away from body when too warm cryptorchidism – one or both testes fail to descend completely animal is sterile – can’t produce normal sperm still produces androgens – normal male appearance and behaviors ANATOMY OF TESTES vaginal tunics – layers of peritoneum covering testes visceral vaginal tunic – on surface of testis parietal vaginal tunic – continuous with parietal peritoneum forms a fibrous sac around testis and spermatic cord open vs. closed castration 2 tunica albuginea – dense, tough connective tissue forming surface of testes and dividing it into lobules seminiferous tubules – coiled tubules within lobules sites of spermatogenesis spermatocytes – form spermatozoa Sertoli cells – support and protect spermatocytes secrete nutrients and hormones (some estrogen) protect spermatocytes from immune system (genetically different than parent animal) interstitial cells – lie between seminiferous tubules secrete androgens – mainly testosterone SPERMATOGENESIS – occurs continuously spermatogonia – diploid stem cells undergo mitosis to constantly produce new spermatocytes 1) primary spermatocyte – diploid cell on peripheral seminiferous tubule undergoes meiosis I 2) 2 secondary spermatocytes – haploid cells undergo meiosis II 3) 4 spermatids – haploid cells undergo differentiation (grow flagellum, etc.) 4) 4 spermatozoa (sperm) released into lumen of seminiferous tubule rete testis – network of tubules that collect sperm take sperm to epididymis to mature Anatomy of Sperm head acrosome – tip containing lysosome-like vesicle contains enzymes to penetrate oocyte nucleus – contains haploid chromosomes midpiece mitochondria – produce ATP for movement tail flagellum (microtubules) – propeller-like movement Hormonal Regulation of Spermatogenesis Hypothalamus – Gonadotropin Releasing Hormone (GnRH) stimulates anterior pituitary Anterior Pituitary Luteinizing Hormone (LH) – stimulates interstitial cells interstitial cells produce testosterone Follicle Stimulating Hormone (FSH) – stimulates Sertoli cells synergism of FSH and testosterone stimulates spermatogenesis 3 Functions of Testosterone prenatal – male reproductive development puberty – maturation of testes and genitals secondary sexual characteristics anabolic effects – increase mass of tissues (bone, muscle) behavior and libido (sex drive) MALE REPRODUCTIVE TRACT EPIDIDYMIS – long, comma-shaped, coiled tube on posterior testis site of sperm maturation and storage secretes nutrients, reabsorbs wastes old sperm digested and reabsorbed DUCTUS (VAS) DEFERENS – muscular tubule that carries sperm from epididymis to urethra ampulla – dilated distal end in some species may produce seminal secretions peristalsis expels sperm rapidly during copulation URETHRA – carries semen and urine to exterior pelvic urethra – in pelvic cavity passes through prostate gland collects sperm and seminal secretions penile urethra – in penis transmits semen to female ACCESSORY REPRODUCTIVE GLANDS – secrete seminal fluid alkaline fluid – neutralizes acid in female reproductive tract fructose – ATP source for sperm motility prostaglandins – stimulate smooth muscle contractions in female reproductive tract Seminal Vesicles – posterior to bladder none in cat or dog Prostate – surrounds urethra enlargement can compress urethra benign hyperplasia – testosterone stimulates growth Bulbourethral Glands – near pelvic outlet none in dog secrete mucus – lubricates urethra and end of penis 4 PENIS – organ of copulation transmits semen (sperm + seminal secretions) to female Anatomy of Penis stratified squamous epithelium tough fibrous connective tissue encloses internal structures roots – connective tissue attachment to pubis body – main portion corpus cavernosum – large, dorsal columns of erectile tissue cause penile erection corpus spongiosum – tube of erectile tissue around urethra prevents collapse of penile urethra during erection glans – distal tip containing erectile tissue and many sensory receptors appearance varies in species prepuce (sheath) – protective skin flap covering flaccid penis smegma – waxy secretion from glands of prepuce skeletal muscles – bulbospongiosus & ischiocavernosus muscles cause pumping contractions of penis during copulation Function of Penis erectile tissues – contain extensive blood sinuses erection – sexual stimulation causes a parasympathetic reflex dilates arteries to penis blood sinuses of erectile tissues fill expansion of erectile tissues compresses veins penis enlarges and stiffens (vasocongestion) emission – continuing stimulation triggers contraction of glands and ductus deferens discharges semen into urethra ejaculation – peak stimulation (orgasm) triggers contraction of penile muscles and urethra ejects semen into vagina or uterus Variations dog – os penis – bone in penis bulb of glans – enlarged erectile region at base of glans “tie” – penis remains stuck in vagina following copulation sigmoid flexure – S-shaped curve of proximal penis (bull, ram, boar) erect penis straightens flaccid penis is withdrawn into sheath by retractor penis muscle urethral process – tube-like extension of urethra beyond the glans (prominent in ram) 5 FEMALE REPRODUCTIVE SYSTEM OVARIES – female gonads site of oogenesis produce estrogens, progestins – female hormones caudal to kidneys usually ovoid anchored to dorsal body wall by suspensory ligament ANATOMY OF OVARIES Ovarian Cortex – outer region developing oocytes all oocytes are already present around the time of birth surrounded by cells that nourish oocytes and secrete hormones follicular cells – single layer of squamous cells surrounding inactive oocytes granulosa cells – 1 or more layers of cuboidal cells around developing oocytes; produce secretions Ovarian Medulla – inner region loose CT, blood vessels and nerves OOGENESIS AND FOLLICULAR DEVELOPMENT hormone levels periodically stimulate development of some oocytes and their surrounding follicles atresia – degeneration of some oocytes and their follicles 1) primary oocytes (diploid) primordial follicles – single layer of squamous follicular cells contain inactive primary oocytes ESTROUS CYCLE – begins at puberty hormones activate a group of primordial follicles periodically growing follicles follicular cells divide, forming multiple layers of granulosa cells granulosa cells secrete hormones and nutritional secretions antrum – fluid-filled pocket in center of follicle mature follicle – blister-like swelling on surface of ovary corona radiata – crown of granulosa cells around oocyte 2) secondary oocyte oocyte in mature follicle undergoes meiosis I, forming 2 haploid cells secondary oocyte – large cell; receives most of cytoplasm first polar body – small packet of chromosomes with no cytoplasm ovulation – mature follicle ruptures and releases ovum and its corona radiata number of ova ovulated varies with species 6 uniparous species – one offspring at a time multiparous species – multiple offspring at once (litters) Fate of Ovum 1) sperm in uterine tube (within 24 hr of ovulation) fertilization – sperm penetrates ovum ovum completes meiosis II – unequal cytokinesis ovum (haploid) – mature egg; large cell second polar body – small, discarded cell nuclei of sperm and ovum unite to form a zygote 2) no sperm in uterine tube degeneration of ovum and end of estrus cycle OVIDUCTS (uterine tubes, Fallopian tubes) normal site of fertilization convoluted tubes that carry sperm to ovum and zygote to uterus Anatomy of Oviducts infundibulum – funnel-shaped portion surrounding ovary fimbriae – fringe on border; sweep oocyte into infundibulum attached to dorsal body wall by mesosalpinx Histology of Oviducts ciliated columnar epithelium – sweeps oocyte through tube secretions nourish ovum, sperm, and zygote smooth muscle – peristalsis helps move ovum and zygote to uterus UTERUS – nourishes and protects the fetus during gestation period attached to dorsal body wall by mesometrium Anatomy of Uterus – varies with species body – caudomedial portion cervix – caudal smooth muscle sphincter; normally closed opens into vagina during estrus and parturition uterine horns – 2 craniolateral arms main sites of fetal development Histology of Uterus 1) perimetrium (outer layer) – visceral peritoneum 2) myometrium (middle layer) 3 layers of smooth muscle contracts during parturition 3) endometrium (inner layer) – supports developing fetus columnar epithelium highly vascular endometrial glands – secrete mucus, nutrients, hormones 7 Types of Uteri bicornuate – 2 long, narrow horns species that have litters (eg. bitch, queen, sow) bipartite – 2 short, thick horns species that have 1 fetus or 1/horn (eg. mare, cow, ewe) simplex – no horns species that have 1 fetus (eg. primates) duplex – 2 long horns, each with its own cervix species that have large litters (eg. rabbit) VAGINA canal from cervix to vulva site of copulation birth canal Histology of Vagina stratified squamous epithelium mucous glands lubricate during copulation normal bacterial flora – create an acidic environment inhibits other microbes (eg. yeast) harmful to sperm – semen buffers acid epithelium thickens and becomes keratinized (cornified) before copulation cytology can be used to time breeding VULVA – external genitals labia – lips of vulva vestibule – entrance to vagina urethral orifice – urethra opens into floor of vestibule clitorus – small erectile structure homologous to penis located just caudal to urethral orifice ESTROUS CYCLE – hormone cycle causes periodic development of ovarian follicles coordinates ovulation with development of the uterus induces behavioral changes and sensory cues that coordinate copulation with ovulation polyestrous – cycle continuously (one cycle ends and the next begins) non-seasonal polyestrous – cycle all year (eg. cow, sow) seasonal polyestrous – only cycle in certain seasons mare, queen – spring/summer ewe – fall/winter diestrous – 2 cycles/year (eg. bitch) 8 HORMONAL REGULATION Hypothalamus – Gonadotropin Releasing Hormone (GnRH) stimulates anterior pituitary Anterior Pituitary Follicle Stimulating Hormone (FSH) stimulates growth of ovarian follicles stimulates estrogen secretion by granulosa cells Luteinizing Hormone (LH) – secreted as estrogen increases stimulates follicle maturation LH peak triggers ovulation promotes differentiation of follicle after ovulation corpus luteum – granulosa cells differentiate secretes progestins, mainly progesterone Functions of Estrogen development of female reproductive tract in fetus stimulates physical and behavioral changes associated with estrus Functions of Progesterone – secreted by corpus luteum after ovulation supports physical and behavioral changes associated with pregnancy prevents further follicle development during pregnancy PHASES OF ESTROUS CYCLE 1) Proestrus follicles developing growing follicles produce increasing estrogen levels estrogen stimulates growth of oviducts, uterus, vagina, and vulva 2) Estrus (heat) estrogen peak prepares animal for breeding LH peak causes ovulation near end of estrus physical and behavioral changes attract males “standing heat” – female receptive to male 3) Metestrus LH stimulates formation of corpus luteum corpus luteum secretes progesterone endometrium prepares for pregnancy vascularity and glandular secretions increase follicle growth inhibited 4) Diestrus – corpus luteum reaches full size No Fertilization – corpus luteum degenerates to corpus albicans progesterone levels decline endometrium degenerates new estrous cycle begins or Anestrus – hormone production shuts down and estrous cycles stop temporarily 9 Fertilization hormone produced by implantation of embryo prevents degeneration of corpus luteum progesterone secretion continues and maintains pregnancy pseudopregnancy – prolonged diestrus in some animals (eg. bitch) corpus luteum fails to degenerate after failure of fertilization increasing progesterone level causes signs similar to pregnancy FERTILIZATION COPULATION – male ejaculates semen into vagina or uterus oxytocin and prostaglandins in semen stimulate contractions of female reproductive tract pumps sperm up into uterine tubes capacitation – male and female secretions activate sperm sperm require time to prepare for fertilization become more motile, prepare to release acrosome enzymes FERTILIZATION – union of ovum and sperm normally occurs in uterine tubes ovum is viable for a limited time following ovulation standing heat is timed to provide capacitated sperm in uterine tubes when ovum arrives sperm swim towards ovum acrosomal enzymes dissolve corona radiata and penetrate ovum male pronucleus – haploid female pronucleus – haploid pronuclei fuse to form diploid nucleus of zygote FETAL DEVELOPMENT zygote divides and differentiates to form a fetus CLEAVAGE – rapid mitotic divisions of zygote without growth occurs as zygote travels into the uterus morula – ball of cells monozygotic (identical) twins – cells separate into 2 separate embryos [dizygotic (fraternal) twins – develop from 2 different zygotes] blastocyst – fluid-filled ball of cells blastocoel – fluid-filled cavity in center trophoblast – wall of blastocyst develops into fetal placenta inner cell mass – cluster of cells near one wall develops into embryo 10 IMPLANTATION – blastocyst attaches to uterine endometrium ectopic pregnancy – abnormal site of implantation PLACENTAL DEVELOPMENT site of exchange with uterine endometrium provides oxygen and nutrients eliminates wastes protects growing fetus – cushions, prevents dessication and adhesions develops from 3 embryonic membranes Amnion – fluid-filled sac surrounding embryo Allantois – fluid-filled sac attached to urinary bladder contains fluid formed by fetal kidneys Chorion – outermost layer formed from the trophoblast umbilical cord – vascular cord connecting fetus to chorion Functions of Chorion: protects embryo from maternal immune system attaches to regions of uterine endometrium – forms functional placenta (site of exchange) diffuse placenta – loose attachment to entire uterine surface (horse, pig) zonary placenta – attached to belt-like region encircling fetus (dog, cat) discoid placenta – attached to a relatively small, circular region (primates, rabbit) cotyledonary placenta – many snap-like attachments to uterus (ruminants) placentome = fetal cotyledon + uterine caruncle form tight attachments that sometimes fail to detach (retained placenta) retained placentas occur less commonly in other types of placentas maternal and fetal blood doesn’t mix – diffusion occurs across the chorion diffusion of oxygen and nutrients to fetal blood diffusion of wastes and carbon dioxide to maternal blood FORMATION OF 3 PRIMARY GERM LAYERS ectoderm – dorsal epithelial layer forms nervous tissues and epidermal structures (skin, hair, etc.) mesoderm – middle loose connective tissue layer forms: all connective tissues, including blood all muscles kidneys and reproductive organs linings of body cavities endoderm – ventral epithelial layer forms linings of GI, respiratory, urinary tracts, digestive glands 11 PREGNANCY gestation period – fertilization to parturition varies widely between species 3 trimesters (3 months each in humans) 1st trimester – embryonic stage rapid division and differentiation of all basic tissues and organ systems all embryos look very similar 2nd trimester – fetal development growth and differentiation of systems into distinct species 3rd trimester – fetal growth dramatic growth and maturation of most systems PARTURITION – birth progesterone (hormone of pregnancy) – supports endometrium and inhibits uterine contractions early pregnancy – corpus luteum produces progesterone later in pregnancy – placenta produces progesterone late pregnancy – progesterone level declines fetus becomes stressed (limited space, uterine support no longer adequate?) secretes stress hormones – glucocorticoids (cortisol) stimulates uterine secretion of prostaglandin F2a prostaglandins + decreased progesterone increase uterine receptors for oxytocin oxytocin stimulates uterine contractions Signs of Parturition enlarged mammary glands (2-6 days prior) may drip colostrum mucous discharge from vulva large animals – dropping of belly, relaxation of pelvis dog – temperature drop of 1-2o F 24 prior behavior changes – restlessness and discomfort nesting behavior large animals – kicking at belly STAGES OF PARTURITION 1) dilation stage – stretching of cervix stimulates oxytocin release positive feedback increases strength of contractions dilates cervix 2) expulsion stage – delivery powerful uterine contractions assisted by abdominal contractions expel fetus stress to neonate causes sympathetic responses prepares infant for extrauterine life 12 3) placental stage powerful contractions expel placenta (afterbirth) dystocia – difficult parturition small dam/large fetus (eg. bred too young) abnormal presentation Caesarian section – surgery to remove fetus from uterus involution – uterus returns to original size (takes weeks) lochia – discharge during sloughing of endometrium MAMMARY GLANDS and LACTATION specialized skin glands location and number varies among species thoracic - inguinal regions 2-4 lactation – secretion of milk beginning shortly before parturition and continuing as long as young nurses proper levels of many hormones required FSH, LH, estrogen, progesterone, prolactin GH, thyroid hormones, glucocorticoids, insulin oxytocin to stimulate letdown of milk Cow Udder 4 “quarters” (separate glands) in inguinal region dairy cow – full udder can weigh over 100 pounds suspensory ligaments support weight of mammary gland medial ligament – tough but elastic 2 lateral ligaments – tough and inelastic compound alveolar glands sac-like glands with highly branched ducts drain into large lactiferous ducts lactiferous ducts drain into sinuses (cavities that store milk) glandular sinus in quarter teat sinus in teat (large papilla that young nurses on) streak canal – single canal through teat to outside sphincter muscle normally closes to prevent leaking myoepithelial cells – smooth musle cells around alveoli and ducts milk letdown – contraction expels milk into sinuses stimulated by oxytocin in response to suckling mammary glands are undeveloped until puberty estrous cycles estrogen and progesterone stimulate hyperplasia of alveoli and ducts near parturition, hormone levels stimulate prolactin release, which stimulates secretions 13 mastitis – infection of mammary gland usually isolated to one quarter unless spread by poor hygiene (milk infected quarter last) colostrum – first milk high levels of proteins, lipids, vitamins, antibodies gives passive immunity to neonate laxative effect – helps clear neonate GI tract meconium – dark, sticky first feces accumulation of dead, degenerate cells from GI tract 14 AVIAN REPRODUCTIVE SYSTEM MALE testes – in abdominal cavity near kidneys enlarge during breeding season seminal fluid – secreted by testes seminal vesicle – sperm storage pouch at distal end of ductus deferens site of sperm maturation – temperature is lower than body temperature no penis in most species sperm is passed by “cloacal kiss” FEMALE female gamete determines sex of offspring only one side of reproductive system develops in most species (usually left) left ovary – grape-like clusters of follicles ovulation – one ovum at a time ovum is attached to a yolk sac containing stored nutrients oviduct infundibulum – catches ovum magnum – secretes albumin (egg white) isthmus – secretes cell membranes uterus – secretes shell and pigment vagina – muscular tube, lays egg clutch – a usual number of eggs are laid one at a time incubation – parent holds eggs against body and or feet to maintain a specific temperature range EGG albumin – protects embryo and stores water yolk sac – vascular sac full of nutrients for embryo amnion – similar to mammals chorioallantois – chorion and allantois fuse and line inner shell exchanges gas across the shell allantois stores urinary waste HATCHING chick absorbs nutrients in yolk as it grows fluid in egg decreases during incubation air space in egg increases – chick begins breathing eggshell thins during incubation – chick uses calcium from shell to grow softens shell, making hatching easier egg tooth – sharp point on upper beak used to crack through shell 15