ch_19_Case Study 1_Answer_Key
advertisement
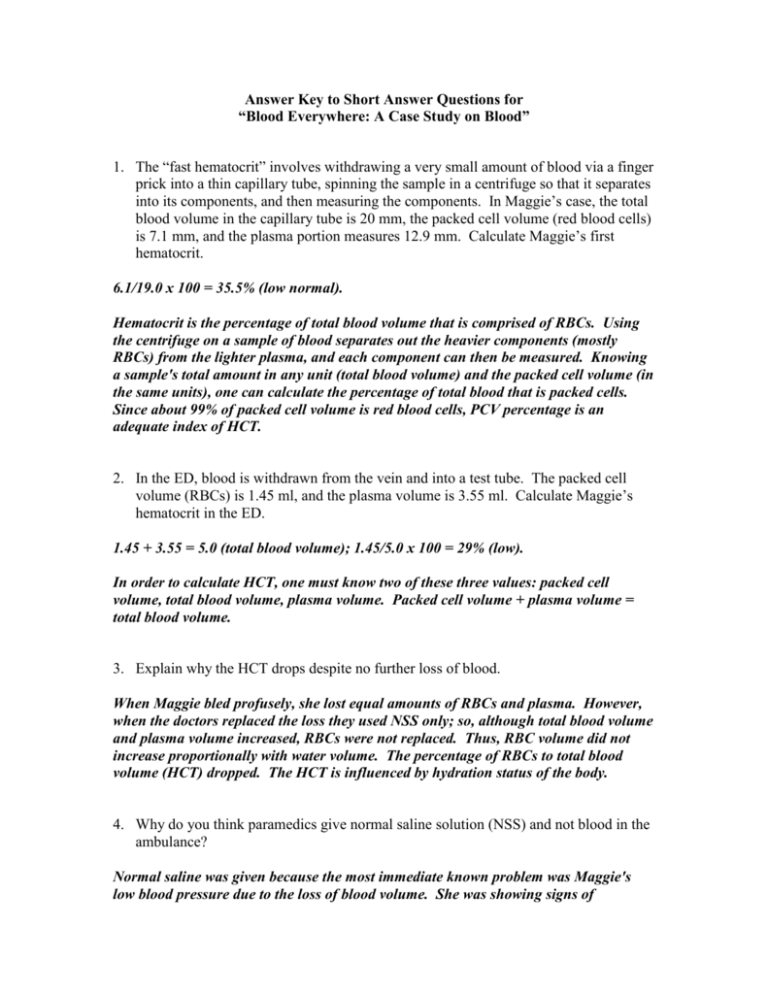
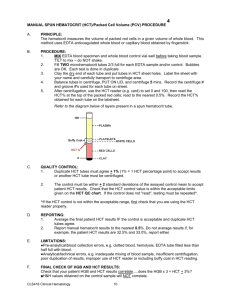
Answer Key to Short Answer Questions for “Blood Everywhere: A Case Study on Blood” 1. The “fast hematocrit” involves withdrawing a very small amount of blood via a finger prick into a thin capillary tube, spinning the sample in a centrifuge so that it separates into its components, and then measuring the components. In Maggie’s case, the total blood volume in the capillary tube is 20 mm, the packed cell volume (red blood cells) is 7.1 mm, and the plasma portion measures 12.9 mm. Calculate Maggie’s first hematocrit. 6.1/19.0 x 100 = 35.5% (low normal). Hematocrit is the percentage of total blood volume that is comprised of RBCs. Using the centrifuge on a sample of blood separates out the heavier components (mostly RBCs) from the lighter plasma, and each component can then be measured. Knowing a sample's total amount in any unit (total blood volume) and the packed cell volume (in the same units), one can calculate the percentage of total blood that is packed cells. Since about 99% of packed cell volume is red blood cells, PCV percentage is an adequate index of HCT. 2. In the ED, blood is withdrawn from the vein and into a test tube. The packed cell volume (RBCs) is 1.45 ml, and the plasma volume is 3.55 ml. Calculate Maggie’s hematocrit in the ED. 1.45 + 3.55 = 5.0 (total blood volume); 1.45/5.0 x 100 = 29% (low). In order to calculate HCT, one must know two of these three values: packed cell volume, total blood volume, plasma volume. Packed cell volume + plasma volume = total blood volume. 3. Explain why the HCT drops despite no further loss of blood. When Maggie bled profusely, she lost equal amounts of RBCs and plasma. However, when the doctors replaced the loss they used NSS only; so, although total blood volume and plasma volume increased, RBCs were not replaced. Thus, RBC volume did not increase proportionally with water volume. The percentage of RBCs to total blood volume (HCT) dropped. The HCT is influenced by hydration status of the body. 4. Why do you think paramedics give normal saline solution (NSS) and not blood in the ambulance? Normal saline was given because the most immediate known problem was Maggie's low blood pressure due to the loss of blood volume. She was showing signs of circulatory shock. Low blood pressure could diminish adequate perfusion to vital organs. A rapid NSS infusion will restore some volume and improve blood pressure. Also, NSS, unlike blood, can be easily stored on the ambulance, does not require special refrigeration, and has a longer shelf life. It is usually abundantly available (compared to blood) and presents no risk of a transfusion reaction. 5. Why might a physician be reluctant to order a blood transfusion for Maggie, or for any patient for that matter, unless absolutely necessary? Blood is sometimes (and in some communities) in short supply and should be used only when absolutely necessary. Any blood transfusion carries with it an increased risk of transfusion reaction, though crossmatch screening processes are strict when followed. Though rare (due to thorough screening procedures), blood may carry blood-borne diseases such as hepatitis, human immunodeficiency virus, malaria, etc. Given time, an otherwise healthy body has the ability to replace its own red blood cells. Blood is more expensive to obtain, process, and store than saline solution. 6. Despite no blood transfusion, Maggie’s hematocrit improves by the time she visits her physician for the removal of her sutures a week later. [See multiple choice question 3 for the calculation.] She is adequately hydrated. Explain the physiological mechanism for the improvement in her hematocrit. When RBCs are lost, HCT drops, and this leads to low oxygen delivery to the tissues (hypoxia). Hypoxia is a signal for the kidney to secrete erythropoietin (EPO). EPO is a hormone that targets red bone marrow to produce more red blood cells, which then restores HCT to normal. This is a negative feedback mechanism. 7. Besides the HCT, what other component of blood could be measured to give a better understanding of oxygen-carrying capacity? Explain your answer. Hemoglobin (Hb) is an index of oxygen-carrying capacity; it is the actual molecule within an RBC that binds oxygen. A normal Hb value for healthy females is 12-16 g/100 ml of blood, and for healthy males it is 13-18 g/100 ml. Typically, HCT and Hb are measured and evaluated together to give a fuller hematological understanding. 8. Explain the relationship between Maggie’s low blood pressure (when the paramedics first examine her) and her blood loss. How are her rapid heart rate and pale, clammy skin related to her low blood pressure? Maggie lost a significant amount of blood volume due to bleeding. When blood volume drops, blood return to the heart is diminished (decreased preload), and cardiac output drops. Blood pressure is determined by cardiac output (stroke volume x heart rate) and peripheral vascular resistance. So, when cardiac output is diminished, the blood pressure drops. It's helpful to recognize primary versus secondary (compensatory) responses. The drop in blood pressure in this case is a primary effect of significant blood loss. A secondary and compensatory effect is for heart rate to increase in an attempt to restore cardiac output, and increased peripheral vasoconstriction, in order to maintain perfusion pressure. These compensations (an effort to maintain circulatory homeostasis) are driven by the sympathetic nervous system. A rapid heart rate and clammy skin are physiological signs of cardiac and peripheral vascular compensation, respectively. Students should begin to identify hallmark signs of shock (decomposition or loss of homeostasis). In this case, it is due to the loss of blood known as hemorrhagic or circulatory shock.