La insuficiencia renal crónica (IRC) es en la actualidad una

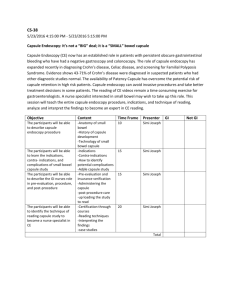
Institution, country and year
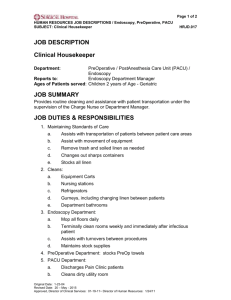
Table 6. Systematic reviews that have assessed the usefulness of capsule endoscopy
Main conclusions
Blue Cross Blue Shield
Association, USA 42
February 2003
Health Technology Assessment
Unit of the McGill University
Centre (MUHC) 43
Quebec, Canada
March 2003
Capsule endoscopy meets the five Blue Cross criteria established to determine that this technology improves health outcomes among patients with obscure gastrointestinal bleeding with possible localization in the small bowel.
CE detects approximately 21% of additional lesions in comparisonother techniques but could not replace them, as they are necessary for conducting biopsies and administering treatments.
No evidence of lower cost.
Few patients benefited.
Insufficient evidence for recommending that this technology be adopted in clinical practice.
The Medical Advisory
Secretariat Ministry of Health and Long-Term Care 44
Ontario, Canada
May 2003
Medical Services Advisory
Committee (MSAC) 45
Canberra, Australia
August 2003
Comité d`Evaluation et de
Diffusion des Innovations
Technologiques (CEDIT) 46
Paris, France
October 2003
Blue Cross Blue Shield
Association 47 .
USA
December 2003
Agencia d`Evaluació de
Tecnología i Recerca Mediques
(AATRM), 34
Spain
December 2003
Agencia de Evaluación de
Tecnologías Sanitarias de
Galicia (avalia-t)
Spain 36
January 2004
National Institute for Clinical
Excellence (NICE) 35
London
December 2004
Capsule endoscopy is indicated for use in small-bowel-related OGB in cases where lesions cannot be identified by endoscopy.
Capsule endoscopy must in all cases be preceded by endoscopy and by radiography to exclude the presence of fistulae or stenosis.
No evidence for evaluating the effectiveness of CE in CD.
Capsule endoscopy could be used as an initial test in some patients with intestinal bleeding.
Specific estimates of diagnostic yield were 58% for CE, 30% for PE, and 4% for SBFT.
Data on adverse effects was of poor quality but nonetheless highlight the fact that such effects are infrequent and of a mild nature.
Economic analysis highlights the fact that, in comparison to SBFT, CE can reduce total patient cost by
$1007.
MSAC recommends that the cost of this procedure be refunded to patients with recurrent OGB, after negative results are obtained in colonoscopy and endoscopy.
CE outperforms PE in evaluation of OGB.
Real diagnostic value (Se, Sp) for OGB is difficult to establish since there is no standard reference test.
Cause-effect relationship between the lesions found in patients with OGB and symptoms cannot be established.
The therapeutic impact on OGB has not being evaluated.
Diagnostic use and therapeutic impact on Crohn's disease has not being clearly evaluated.
Use in pediatrics is unknown.
CEDIT recommends that CE be adopted at health centers with experience.
CE shows lesions indicative of Crohn's disease in 43%-71% of patients with negative results in other tests.
Insufficient evidence to determine the usefulness of CE in patients with suspected Crohn's disease, who have not been previously assessed.
Insufficient evidence for other disorders evaluated.
CE indicated in CD not diagnosed by other tests.
Capsule endoscopy seems to have a greater diagnostic capacity than other alternative technologies in diagnosis of OGB.
For CD, capsule endoscopy should be considered experimental.
No studies addressing diagnostic accuracy (Se,Sp,PPV,NPV)
Economic assessment enabled an algorithm to be proposed, i.e., after EGD, duodenoscopy , gammagraphy, re-endoscopy and CE.
CE outperforms other techniques in OGB.
CE outperforms other techniques in CD.
CE should be used as a complementary technique, ancillary to other procedures and after performing a
SBFT.
Appropriately designed studies are called for.
CE can detect source of bleeding in 31%-76% of patients but it is not possible to ascertain diagnostic efficacy or changes in health outcomes.
CE identifies CD in 43%-71% of patients with negative tests. Insufficient evidence in terms of quantity and quality for diagnostic efficacy to be ascertained in unselected patients.