Physical Activity and Years of Healthy Life in Older Adults

1
MS E-112 Physical Activity and Healthy Life Draft v1
Physical Activity and Years of Healthy Life in Older Adults: Results from the
2
Cardiovascular Health Study
5
6
3
4 Calvin H. Hirsch, MD 1 , Paula Diehr 2 , Anne B. Newman, MD 3 , Shirley A. Gerrior, Ph.D
4 ,
Charlotte Pratt, PhD 5 , Michael D. Lebowitz, MD 6 , Sharon A. Jackson, PhD 7 for the
7 Cardiovascular Health Study Research Group
8 Funding sources: Contracts N01-HC-35129, N01-HC-45133, N01-HC-75150, N01-HC-85079
9 through N01-HC-85086, N01 HC-15103, N01 HC-55222, and U01 HL080295 from the National
10 Heart, Lung, and Blood Institute, with additional contribution from the National Institute of
11 0Neurological Disorders and Stroke.
1
(Corresponding author) Depts. of Medicine and Public Health Sciences, Div. of General
Medicine, University of California, Davis Medical Center, PSSB-2400, Sacramento, CA 95817.
Ph: 916-734-7005; Fx: 916-734-2732. E-mail: chhirsch@ucdavis.edu
2 (Alternate corresponding author) Dept. of Biotatistics, University of Washington, Seattle, WA
98195. Ph: 206-543-8004; Fx: 206-543-3286 E-mail: pdiehr@u.washington.edu
3
Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA
4
Human Nutrition Research and Extension, US Dept. of Agriculture, Washington, DC
5
Div. of Epidemiology and Clinical Applications, National Heart, Lung, and Blood Institute,
Bethesda, MD
6
Depts. of Medicine and Public Health Sciences, Univ. of Arizona, Tucson, AZ
7
Div. for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention,
Atlanta, GA
1 of 22
14
15
16
12
MS E-112 Physical Activity and Healthy Life
13 Presented in part at the national meeting of the American Geriatrics Society, May, 2006
Draft v1
2 of 22
17
MS E-112
ABSTRACT
Physical Activity and Healthy Life Draft v1
18 Objective : To determine the number of years associated with survival and disability-free years
19 at different levels of physical activity (PA) in older adults from different age groups.
20 Design: Longitudinal cohort study.
21 Participants: 5,392 participants of the Cardiovascular Health Study.
22 Measurements : We assessed the independent contribution of self-reported PA to survival and
23 years with self-reported good or better health over 11 years, and to years free of disability over 6
24 years. Quintiles of PA, measured in kcal/week, were established for 3 age groups: 65-69, 70-74,
25 and > 74. Multivariable linear regression adjusted for a wide array of demographic and health-
26
27
28 related variables.
Results
: At baseline, participants’ mean age was XX (range: XX-YY), xxxx (XX%) were men, and xxxx (XX%) reported dependence in
1 IADL. [RESULTS NEED TO BE UPDATED
29 BASED ON THE EVALUABLE SAMPLE OF 5392.] Survival averaged 9.96 (
2.34) [Note.
30 This is a standard error. Elsewhere in the paper, the quantity in parentheses represents a standard
31 deviation. I suggest that you present a confidence interval here (9.6-1.96*2.34, 9.6 +
32
33
1.96*2.346 here, and explain elsewhere that you mean standard deviation]. years for participants aged 65 to 69 and 8.09 (
3.31) years for those over age 74. Compared to the least active
34 quintile after adjusting for covariates, PA had no significant impact on survival in the 2 younger
35 age groups. Among participants > age 74, those in the most active quintile lived 1.02 (± 0.22)
36 years longer than those in the least active quintile (p < .001). PA increased disability-free years
37 for ADL, IADL, and mobility in subjects aged > 69. Compared to the least active quintile,
38 disability-free years increased with higher activity and age, but only slightly (≤ 1.01 years).
3 of 22
39
MS E-112 Physical Activity and Healthy Life Draft v1
Conclusions : The increased longevity and years of healthy life associated with higher physical
40 activity accrue mostly to persons over age 74.
41 (250 words)
42 Key words: Aging, Exercise, Mortality, Activities of Daily Living, Mobility Limitation
4 of 22
43
MS E-112
44
Physical Activity and Healthy Life Draft v1
45 INTRODUCTION
46 It is well-established that a physically active lifestyle is associated with a reduced risk of
47 mortality in middle-aged adults. This mortality benefit appears remarkably stable over time,
48 persisting for 16 years among men and women in the Framingham heart Study cohort and 22
49 years among male participants of the Harvard Alumni Health Study. (Lee, 1992; Lee 2000;
50 Sherman 1994a) Among the middle-aged, the reductions in mortality correlate in a dose-
51 response fashion with the energy consumed in intense physical activities or with exercise
52 capacity, with negligible benefit from non-vigorous activities, regardless of the net energy
53 expended . (Lee, 1994; Gulati, 2003) Epidemiologic studies focusing on persons over age 65
54 likewise have demonstrated a reduced risk of mortality in those who are physically active
55 compared to being sedentary.(1-11) Although the studies differ in the ways they assessed
56 physical activity and defined a physically active lifestyle, overall they demonstrate that older
57 individuals need to perform less vigorous physical activity than middle-aged adults to achieve a
58 significant reduction in mortality risk.
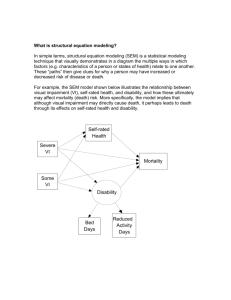
59 In middle-aged and older adults, regular physical activity also protects against functional
60 decline and the development of disability.(5, 8, 12-19) Consistent with the pathway of
61 disablement hypothesized by Verbrugge and Jette,(20) physical activity’s ability to prevent
62 disability appears to derive from its ability to reduce the development of functional
63 limitations.(8) In an older cohort (median age = 70), Tager et al. showed that high levels of
64 leisure-time physical activity independently protected against the development of severe
65 functional limitations in men. In women, however, their results suggested that physical activity
5 of 22
66
MS E-112 Physical Activity and Healthy Life Draft v1 reduces the risk of severe functional limitation by its effect on the proportion of lean body mass
67 to fat mass. (18)
68 Although higher levels of physical activity reduce the risk of dying and functional decline,
69 compared to staying sedentary, there has been little effort to date to translate the impact of a
70 physically active lifestyle into the actual number of years it can increase survival or years free of
71 functional limitations. Using data from the Framingham heart study, Franco et al. calculated
72 mean life expectancy after age 50 from the hazard ratio for mortality, stratifying by level of
73 physical activity.(21) However, the comparative benefits of physical activity for survival and
74 disability-free years, compared to being sedentary, have not been established in older adults from
75 different age groups. To ascertain this, we utilized 11 years of follow-up data for survival and
76 self-rated health, and 6 years of follow-up data for disability from the Cardiovascular Health
77 Study, a population-based cohort study of men and women aged 65 and older at study entry.
78
79 METHODS
80 Study Cohort
81 The Cardiovascular Health Study (CHS) is an ongoing, observational, population-based
82 cohort study of persons aged 65 and over recruited from 4 communities in the United States:
83 Sacramento County, California; Allegheny County, Pennsylvania; Forsyth County, North
84 Carolina; and Washington County, Maryland. CHS supplemented the original cohort of 5,201
85 men and women, which was enrolled between 1989 and 1990, with an additional 687 African-
86 Americans during the 4 th
study year (1992-1993). Details of the study design are described
87 elsewhere. (3, 22)
88 Data Collection
6 of 22
89
MS E-112 Physical Activity and Healthy Life Draft v1
Using standardized questionnaires and procedures, trained technicians collected demographic
90 and psychosocial information; data on health habits; a standardized medical history for selected
91 conditions and current medications; objective cardiovascular data; reported and objective
92 measures of physical performance; data on affective state and cognitive functioning; and blood
93 samples for a variety of laboratory analyses performed at the Laboratory for Clinical
94 Biochemistry Research at the University of Vermont. Participants returned for annual clinic
95 visits and underwent telephone interviews 6 months after each visit through 1999. Limited
96 telephone surveillance for study outcomes has continued since 2000. Deaths initially were
97 identified by interview with an informant and listings in obituary columns, and later confirmed
98 by reviewing medical records, death certificates, and the HCFA health care utilization database
99 for hospitalizations. There has been 100% ascertainment of participant mortality.
100 Variables
101 Outcome variables: Our outcomes of interest were the average number of additional years of life
102 and years of healthy life (years in good, very good, or excellent health) (YHL), over 11 years of
103 follow-up, associated with being physically active compared to being sedentary at study entry. [I
104 strongly prefer years of healthy life and YHL because it’s what I (and a few others) have always
105 used.] Additional outcomes included average additional years free from disability over 6 years of
106 follow-up as a result of physical activity. Disability in activities of daily living (ADL) was
107 defined as any reported difficulty walking around the home, getting out of bed, eating, dressing,
108 bathing, or using the toilet. We defined disability in instrumental activities of daily living
109 (IADL) as reported difficulty performing heavy housework, doing light housework, shopping,
110 preparing meals, paying bills, or using the telephone. We defined upper-extremity disability as
7 of 22
111
MS E-112 Physical Activity and Healthy Life Draft v1 reported difficulty lifting, reaching, or gripping. Mobility disability was defined as reported
112 difficulty walking ½ mile or ascending 10 steps.
113 Predictor variable: The principal predictor variable was the energy in kilocalories (kcal)
114 consumed in weekly leisure-time physical activity plus household chores estimated from the
115 Minnesota Leisure Time Activities Questionnaire, which was based on the 2 weeks prior to the
116 baseline visit.(23) [Did we ever consider a combined outcome, for years without any of those
117 problems? I guess it would be hard to explain. But we did do this on a different paper for
118 several measures of balance].
119 Analytic approach
120 These analyses include both the original and African-American cohorts. [A lot of this seems
121 to be understandable only by CHS people. For others, it is TMI (too much information). We
122 used multivariable linear regression to assess the independent contribution of baseline physical
123 activity to each of the outcome measures. Participants were divided into 3 age groups: 65-69,
124 70-74, and ≥ 75. Physical activity in kcal was divided into age-category-specific quintiles, with
125 participants in the lowest quintile serving as the reference group. For each outcome, separate
126 regressions were run for the 3 age groups. As potential confounders, we selected variables that
127 previously had been shown to predict 5-year mortality in the CHS.(24). We also selected
128 variables which had a bivariate association with one or more of the functional outcome measures
129 or which plausibly could contribute to functional impairment. Covariates included demographic
130 and personal characteristics, reported chronic illness such as arthritis, established risk factors for
131 cardiovascular disease (CVD) such as smoking and hypertension, assessed subclinical CVD
132 (e.g., ankle-brachial index, internal carotid wall thickness), inflammatory markers, adjudicated
133 prevalent cardiovascular disease and congestive heart failure, depressive symptoms measured by
8 of 22
134
MS E-112 Physical Activity and Healthy Life Draft v1 a 10-item version of the Center for Epidemiological Studies depression questionnaire (CES-
135 D),(25) historical physical activity, and age-gender interaction term, and cognitive function
136 measured by the Digit Symbol Substitution Test(26) plus the Mini-Mental State Examination
137 (MMSE).(27) Because the CHS switched to the 100-item Modified MMSE(28) after the first
138 year, we converted the Modified MMSE back into a 30-point scale to allow the merger of data
139 from the original and African-American cohorts. [TMI?] Baseline scores for SRHL [I usually
140
141 call this EVGGFP, but I’m ok with SRHL], ADL, IADL, and upper-extremity function, as well as the presence or absence of difficulty walking ½ mile or up 10 steps, were included as
142 covariates in each model. The same covariates were used in all regressions, so that any
143 differences seen in the results for the different outcomes could be attributed to the outcomes
144 themselves, rather than to differences in the covariates selected. Covariates with a non-normal
145 distribution were normalized by log transformation.
146 The valid N for individual variables ranged from 5729 to 5868. Preliminary regressions
147 using the chief predictor, kcal, plus all selected covariates yielded models with a valid N of 4,399
148 due to missing values. Eight covariates (income, bioresistance [a measure of lean body mass],
149 low-density lipoprotein, pack-years of cigarettes smoked, calculated renal disease status,
150 fibrinogen, and the Digit Symbol Substitution Test score) each had more than 80 missing values
151 and were not significantly correlated with any outcome measure. [TMI?] Removing them
152 increased the valid N to 5,392. The remaining variables, listed in Table 1, were included as
153 covariates in the regressions reported below.
9 of 22
154
MS E-112
RESULTS
Physical Activity and Healthy Life Draft v1
155 Table 1 shows the baseline characteristics of the study cohort. African Americans made up
156 16.4% of the sample. The participants were well-educated with an average of 1.7 years beyond
157 secondary school; 74.4% reported good to excellent health. Among the 5858 participants with
158 evaluable data on functional status, the prevalence of disability was substantially higher among
159
160 women compared to men. Ten percent of women but only 5.6% of men reported dependence in
1 basic ADL. Among women, 30.7% reported dependence in
1 IADL, compared to 19.1%
161 of men. More than twice as many women than men reported difficulty walking ½ mile or
162 climbing up 10 steps (17.8% v 8.3%), as well as difficulty reaching, lifting, or gripping (17.8% v
163 8.3%). [These numbers are identical, which seems a bit coincidental. Was there an error in the
164 tables?] [As I mentioned in my e-mail, I had fixed that but then apparently reverted to an earlier
165 version – I work at chs only 1 day a week, so probably updated this on one of my other
166 computers. Whine whine. Anyway, it works now. Or does it?] The amount of baseline
167 leisure-time and chore-related physical activity ranged from a low of 0 kcal per week to over
168 13,000 kcal per week, regardless of age group. The mean weekly energy expenditure declined in
169 the older age groups and was consistently lower in women than men (Table 2a). However,
170 within a given quintile of physical activity, the mean and median energy consumed remained
171
172 relatively stable with increasing age (Table 2).
Survival in the 11 years after baseline averaged 9.96 (
2.34) [as I mentioned above, the 2.34
173
174 is a standard deviation. You should say so, perhaps right here, because a lot of people would present the standard error using this notation]. years for participants aged 65 to 69 and 8.09 (
175 3.31) years for those aged 75 and older (Table 3). Over 11 years of follow-up, years with
176 reported good to excellent health averaged 2.21 to 2.66 years less than mean survival, depending
10 of 22
177
MS E-112 Physical Activity and Healthy Life Draft v1 on age group. Over 6 years of follow-up, older participants on average had fewer disability-free
178 years than younger participants. The study cohort had fewer mean years free of IADL disability
179 than ADL disability, with the disparity widening slightly with age (0.71 years for those 65-69,
180 0.97 years for those 75+). On average, study participants experienced slightly fewer years free
181 of mobility impairment than upper-extremity impairment, and this difference increased with age,
182 from 0.13 year for those 65-69 to 0.46 year for the oldest age group.
183 The outcome measures were highly associated with exercise variables in the hypothesized
184 direction. However, adjusting for the covariates decreased the apparent benefit of exercise by
185 nearly a year, on average. In the following we present only the adjusted outcomes. [I think this
186 is interesting and cautionary].
187 Higher baseline levels of physical activity among individuals aged 65-69 did not significantly
188 improve either survival or years with reported good to excellent health over 11 years of follow-
189 up, compared to those in the least active quintile (Figures 1a and 1b). A similar lack of impact
190 was observed for the 70-74 age group, except for persons in the most active quintile. However,
191 among participants aged 75 and older at study entry, additional years of life and healthy life
192 [here you do refer to years of healthy life. I am happy.] increased monotonically with increasing
193 levels of physical activity. After adjustment for covariates, the most active individuals at
194 baseline lived an average of 1.02 years longer and experienced an average of 1.23 more years of
195 self-reported healthy life than their inactive peers.
196 Greater physical activity enabled all 3 age groups to achieve longer independence in IADLs
197 than those in the least-active quintile during 6 years of follow-up, after adjusting for covariates
198
199
(Figure 2a). For the 65-69 group, the relationship between higher levels of physical activity and additional years of IADL independence was asymptotic, peaking at 0.42
0.11 additional years.
11 of 22
200
201
MS E-112 Physical Activity and Healthy Life Draft v1
The 70-74 and > 74 age groups experienced linear increases in years free of IADL dependence as a function of increasing levels of physical activity, with gains of 0.72
0.12 and 0.78
0.13
202 years, respectively, for the most active seniors. Relative to the least active quintile, higher levels
203 of physical activity yielded fewer additional years free of ADL dependence than IADL
204 independence, after adjustment for covariates, and did not yield significant gains in either of the
205 2 highest activity levels in the 65-69 group (Figure 2b). The gains in ADL-free years, relative to
206 the least active quintile, rose with increasing levels of physical activity among participants over
207 age 69, but were highest in the oldest age group.
208 Figure 2c demonstrates a generally linear trend, for each age group, in the gain of years free
209 of mobility impairment with higher activity quintiles, compared to the least active quintile. The
210 relative gains in years of mobility independence, which were small and mostly statistically
211
212 insignificant in those aged 65-69, became larger with each successive age group. The most active quintile in the 70-74 and
75 age groups respectively experienced 0.65
0.14 and 1.01
213 0.14 more years of mobility independence than the least active quintile of their respective age
214 groups. In contrast to mobility independence, the benefits of physical activity for years free of
215 upper-extremity dependence were essentially confined to the most active seniors in the oldest
216 age group (Figure 2d).
217
12 of 22
218
MS E-112
219 DISCUSSION
Physical Activity and Healthy Life Draft v1
220 Our study suggests that the survival advantage associated with physical activity in persons
221 over age 65 accrues primarily to persons of advanced old age (75+) who expend more than 1000
222 kcal per week in physical activity. The lack of association between physical activity and survival
223 in the young-old may reflect, in part, their low overall mortality rate. While performing
224 moderate to intense physical activity in advanced old age could be construed simply as a marker
225 of robust health leading to greater survival, our adjustment for an extensive array of personal and
226 health characteristics casts doubt on such an explanation. The threshold of approximately 1000
227 kcal/wk in physical activity for a statistically significant survival benefit is consistent with the
228 results of Manini et al. (7), who assessed energy expenditure in high-functioning community-
229 dwelling adults over age 69 and followed them for an average of 6.2 years. Active energy
230 expenditure (AEE) between 521 and 770 kcal/day (measured by double-labeled water) was
231 associated with a 35% lower mortality risk, compared to individuals with an AEE < 521
232 kcal/day. An AEE of 521-770 kcal/day corresponded to an average of 1204 kcal/wk derived
233 from reported physical activity. By contrast, analysis of data from the Study of Osteoporotic
234 Fractures (SOF) cohort study (7553 women, mean age 76.9) revealed a lower threshold of 163-
235 503 kcal/week to achieve a significant reduction in mortality. SOF also did not find a clear dose-
236 response effect on mortality risk reduction with increasing activity quintiles. The lower
237 threshold activity may have been due, in part, to the use of different methodology to assess
238 physical activity (4).
239 Although reported exercise behavior before age 65 was not associated with any study
240 outcomes in our multivariable models, we did not have information on exercise for the years
13 of 22
241
MS E-112 Physical Activity and Healthy Life Draft v1 immediately preceding enrollment for participants older than 65 at study entry. [This reminds
242 me that we (or at least I) once discussed one more set of regressions where we remove all the
243 variables that might conceivably be in the causal pathway --- just in case some readers think we
244 over-controlled. Maybe that is just too complicated. I don’t recall if we decide *not* to do this.]
245 Consequently, we were unable to determine whether the survival benefit of physical activity was
246 driven by a long-term, cumulative effect on health or by a more near-term effect. In the Study
247 of Osteoporotic Fractures, 7553 women underwent 2 assessments approximately 6 years apart
248 and were followed for an additional 6.7 years. The investigators found that staying or becoming
249 active was associated with similar reductions in the hazard rate ratios for all-cause and
250 cardiovascular mortality, after adjusting for age, smoking, BMI, self-reported health, and a
251 variety of comorbidities. Conversely, becoming sedentary was equivalent to remaining
252 sedentary in conferring an increased risk of dying (4). The Gregg study, too, is prone to
253 selection bias, in that persons who changed their level of exercise were likely to have done so
254 because of their health. Although restricted to women, the results suggest that current, not past,
255 physical activity in old age confers survival benefit, and that this survival benefit attenuates over
256 the span of a few years once an individual becomes inactive. By contrast, our analysis, as well
257 as results for women (but not men) from the Framingham Study, have shown that a single
258 assessment of physical activity in persons aged 75 and older can predict a lower risk of mortality
259 as far out as 10 to 11 years(10). A major confounder in interpreting epidemiological studies of
260 exercise and mortality in the elderly is the lack of information on the variability of exercise
261 behavior following activity assessment and the role of this variability in determining the
262 longitudinal effects of exercise on mortality.
14 of 22
263
MS E-112 Physical Activity and Healthy Life Draft v1
A striking finding of our study was the manner in which the effect of baseline physical
264 activity on the number of years with reported good health closely paralleled the effect on actual
265 survival. [I do think this is a striking finding, and have even written a paper about it –
266 unpublished to date. However, most people will think that this is obvious, because YHL are
267 limited by YOL – can’t be healthy and dead. Maybe remove this sentence? FYI, my manuscript
268 is at http://faculty.washington.edu/~pdiehr/nsick_current.doc
if you care.]Poor self-rated health
269 (SRH) has been shown to be a robust predictor of mortality in older persons, even after
270 adjustment for comorbidities (29). In turn, physical activity has been shown to correlate
271 significantly with SRH in middle-aged and older adults, as well as in persons with chronic illness
272 and disability (30-32). Using logistic regression, Leinonen et al. observed that a decline in
273 physical activity, but not baseline physical activity, predicted a decrease in SRH [a new name for
274 this variable? I usually called in evggfp, but ok with me to do something different, just be
275 consistent] over 5 years in a Finnish cohort of 75-year-old men and women (33). [there is
276 probably self-selection bias in this paper too, right?] More research is required to explore the
277 inter-relationships between physical activity and other known determinants of self-rated health.
278 Although muscle strength declines with age, it may remain above the threshold for an effect
279 on physical performance among sedentary young-old adults. With advancing age, this threshold
280 has a greater likelihood of being crossed (34), enabling the relative benefits of a physically active
281 versus sedentary lifestyle on the development of disability to become manifest. We have
282 previously shown in the CHS cohort that weekly physical activity expressed in kilocalories
283 independently correlates with gait speed and the time to complete 5 chair stands (35), measures
284 that are directly related to quadriceps strength (34, 36). As with survival, we could not
285 determine in the present analysis whether the protective effect of baseline physical activity on
15 of 22
286
MS E-112 Physical Activity and Healthy Life Draft v1 disability-free years occurred as a result of cumulative physical activity throughout old age, or
287 whether the effect was more proximal. Christensen et al. analyzed the impact of inactivity on
288 mortality among 387 survivors of the Glastrup (Denmark) 1914 age cohort (13). After
289 adjustment for gender, smoking, and household composition, physical inactivity at age 70
290 predicted disability at age 75, whereas cumulative physical activity between ages 50 and 70 did
291 not.
292 Unlike its effect on years free of impaired mobility, physical activity did not significantly
293 increase years free from upper-extremity impairment until after age 74, and only in the those in
294 the 2 uppermost activity quintiles. [NEED RESULTS ON AGE-STRATIFIED PREVALENCE
295 OF UE DYSFXN.] These observations could reflect better preservation of upper-extremity than
296 lower-extremity function in advanced old age. The type of exercises, like weight lifting, that
297 would benefit lifting, reaching, and grasping may not require a greater expenditure of energy per
298 se, but might only occur as part of more overall intensive exercise regimens. The selection of
299 activities in the CHS activity questionnaire could also bias against showing a benefit for upper-
300 extremity function. Of the 17 activities, 7 emphasize lower-body exercise (eg, walking, hiking),
301 8 involve mixed upper- and lower-body activity (eg, swimming, gardening), and only 2 reflect
302 mostly upper-body activity (bowling and raking).
303 Some studies are restricted to healthy people. A strength of our study is that it refers to
304 persons in a general population (subject to their having enough baseline data). We also account
305 for death when looking at the other non-survival outcomes, by looking at the number of years in
306 which there are good outcomes.
307 Conclusions
16 of 22
308
MS E-112 Physical Activity and Healthy Life Draft v1
In cross-sectional analysis, the mean leisure-time energy expenditure declines in successively
309 older age groups, but when stratified by quintile of activity, the mean energy expenditures of
310 seniors over age 74 are similar to those of seniors aged 65-69. [this weird statement is a function
311 of my having given you tables using the non-age-specific quintiles. You’ll see that it’s no longer
312 true.] A single measurement of physical activity predicts survival and years with self-reported
313 good health up to 11 years later, as well as years free of disability up to 6 years later. After
314 adjustment for demographic and health characteristics, the extra survival and years of healthy life
315 within an age group associated with leisure-time physical activity (compared to being sedentary)
316 are proportionate to the amount of physical activity, are generally not statistically significant
317 until after age 74, and are modest even at the highest weekly energy expenditures. Relative to
318 sedentary older adults, seniors who are physically active also have more disability-free years for
319 ADL, IADL, mobility, and upper-extremity function. With the exception of upper-extremity
320 function, extra disability-free years can be observed before age 75 with less weekly energy
321 expenditure than required to show a survival benefit. The absolute gain in disability-free years
322 is small, even for the most active seniors.
323 This study has several important limitations. Although we controlled for an extensive array
324 of health-related variables, physical activity may still be a marker for unmeasured good health.
325 That is, it may not be exercise that makes older individuals healthier, but rather that being
326 healthy allows older individuals to exercise. Because the CHS does not have accurate estimates
327 of pre-baseline physical activity, we were unable to determine whether taking up exercise in old
328 age confers the same benefit for survival and disability-free years as always being active.
17 of 22
329
MS E-112
330 ACKNOWLEDGEMENTS
Physical Activity and Healthy Life Draft v1
331 The research reported in this article was supported by contracts N01-HC-35129, N01-HC-45133,
332 N01-HC-75150, N01-HC-85079 through N01-HC-85086, N01 HC-15103, N01 HC-55222, and
333 U01 HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution
334 from the National Institute of Neurological Disorders and Stroke. A full list of participating CHS
335 investigators and institutions can be found at http://www.chs-nhlbi.org.
336
18 of 22
344
345 3.
346
347 4.
348
349 5.
350
351
352 6.
353
337
MS E-112
REFERENCES
338
339
340
1.
341
342 2.
343
89.
Physical Activity and Healthy Life
Bijnen FC, Feskens EJ, Caspersen CJ, et al. Baseline and previous physical activity in relation to mortality in elderly men: the Zutphen Elderly Study. Am J Epidemiol.
Draft v1
Aijo M, Heikkinen E, Schroll M, et al. Physical activity and mortality of 75-year-old people in three Nordic localities: a five-year follow-up. Aging Clin Exp Res. 2002;14:83-
1999;150:1289-1296.
Fried LP, Borhani NO, Enright P, et al. The cardiovascular health study: Design and
Rationale. Ann Epidemiol. 1991;1:263-276.
Gregg EW, Cauley JA, Stone K, et al. Relationship of changes in physical activity and mortality among older women. Jama. 2003;289:2379-2386.
Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc. 2000;48:493-498.
Landi F, Cesari M, Onder G, et al. Physical activity and mortality in frail, communityliving elderly patients. J Gerontol A Biol Sci Med Sci. 2004;59:833-837.
Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. Jama. 2006;296:171-179.
354 7.
355
356 8.
357
358 9.
359
Miller ME, Rejeski WJ, Reboussin BA, et al. Physical activity, functional limitations, and disability in older adults. J Am Geriatr Soc. 2000;48:1264-1272.
Rakowski W, Mor V. The association of physical activity with mortality among older adults in the Longitudinal Study of Aging (1984-1988). J Gerontol. 1992;47:M122-129.
19 of 22
360
MS E-112 Physical Activity and Healthy Life Draft v1
10. Sherman SE, D'Agostino RB, Cobb JL, et al. Does exercise reduce mortality rates in the
361 elderly? Experience from the Framingham Heart Study. Am Heart J. 1994;128:965-972.
362 11. Stessman J, Maaravi Y, Hammerman-Rozenberg R, et al. The effects of physical activity
363 on mortality in the Jerusalem 70-Year-Olds Longitudinal Study. J Am Geriatr Soc.
364
366
2000;48:499-504.
365 12. Berk DR, Hubert HB, Fries JF. Associations of changes in exercise level with subsequent disability among seniors: a 16-year longitudinal study. J Gerontol A Biol Sci Med Sci.
367 2006;61:97-102.
368 13. Christensen U, Stovring N, Schultz-Larsen K, et al. Functional ability at age 75: is there
369
370 an impact of physical inactivity from middle age to early old age? Scand J Med Sci
Sports. 2006;16:245-251.
371 14. Leveille SG, Guralnik JM, Ferrucci L, et al. Aging successfully until death in old age:
372 opportunities for increasing active life expectancy. Am J Epidemiol. 1999;149:654-664.
373 15. Mor V, Murphy J, Masterson-Allen S, et al. Risk of functional decline among well elders.
374
376
J Clin Epidemiol. 1989;42:895-904.
375 16. Patel KV, Coppin AK, Manini TM, et al. Midlife physical activity and mobility in older age: The InCHIANTI study. Am J Prev Med. 2006;31:217-224.
377 17. Schroll M, Avlund K, Davidsen M. Predictors of five-year functional ability in a
378 longitudinal survey of men and women aged 75 to 80. The 1914-population in Glostrup,
379
381
Denmark. Aging (Milano). 1997;9:143-152.
380 18. Tager IB, Haight T, Sternfeld B, et al. Effects of physical activity and body composition on functional limitation in the elderly: application of the marginal structural model.
382 Epidemiology. 2004;15:479-493.
20 of 22
383
MS E-112 Physical Activity and Healthy Life Draft v1
19. Wang BW, Ramey DR, Schettler JD, et al. Postponed development of disability in
384 elderly runners: a 13-year longitudinal study. Arch Intern Med. 2002;162:2285-2294.
385 20. Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1-14.
386 21. Franco OH, de Laet C, Peeters A, et al. Effects of physical activity on life expectancy
387
389 with cardiovascular disease. Arch Intern Med. 2005;165:2355-2360.
388 22. Tell GS, Fried LP, Hermanson B, et al. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:358-366.
390 23. Taylor HL, Jacobs DR, Jr., Schucker B, et al. A questionnaire for the assessment of
391 leisure time physical activities. J Chronic Dis. 1978;31:741-755.
392 24. Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older
393 adults: the Cardiovascular Health Study [see comments]. Jama. 1998;279:585-592.
394 25. Orme JG, Reis J, Herz EJ. Factorial and discriminant validity of the Center for
395 Epidemiological Studies Depression (CES-D) scale. J Clin Psychol. 1986;42:28-33.
396 26. Wechsler D. Manual for the Wechsler Adult Intelligence Scale-
397 Revised San Antonio: The Psychological Corporation; 1981.
398 27. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for
399 grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-198.
400 28. Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin
401 Psychiatry. 1987;48:314-318.
402 29. Bosworth HB, Siegler IC, Brummett BH, et al. The association between self-rated health
403
404 and mortality in a well-characterized sample of coronary artery disease patients. Med
Care. 1999;37:1226-1236.
21 of 22
405
MS E-112 Physical Activity and Healthy Life Draft v1
30. Kanagae M, Abe Y, Honda S, et al. Determinants of self-rated health among community-
406 dwelling women aged 40 years and over in Japan. Tohoku J Exp Med. 2006;210:11-19.
407 31. Cott CA, Gignac MA, Badley EM. Determinants of self rated health for Canadians with
408 chronic disease and disability. J Epidemiol Community Health. 1999;53:731-736.
409 32. Wolinsky FD, Stump TE, Clark DO. Antecedents and consequences of physical activity
410 and exercise among older adults. Gerontologist. 1995;35:451-462.
411 33. Leinonen R, Heikkinen E, Jylha M. Predictors of decline in self-assessments of health
412 among older people--a 5-year longitudinal study. Soc Sci Med. 2001;52:1329-1341.
413 34. Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, et al. Functionally relevant thresholds of
414
416 quadriceps femoris strength. J Gerontol A Biol Sci Med Sci. 2002;57:B144-152.
415 35. Hirsch CH, Fried LP, Harris T, et al. Correlates of performance-based measures of muscle function in the elderly: the Cardiovascular Health Study. J Gerontol A Biol Sci
417 Med Sci. 1997;52:M192-200.
418 36. Brown M, Sinacore DR, Host HH. The relationship of strength to function in the older adult. J Gerontol A Biol Sci Med Sci. 1995;50 Spec No:55-59. 419
420
421
22 of 22