Chief, Division Of Neurology Program Director, Residency Program
advertisement

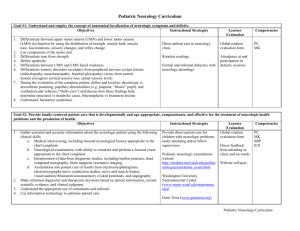
PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM SECTION 16: NEUROLOGY This section has been reviewed and approved by the Chief, Division of Neurology as well as the Program Director, Internal Medicine Residency Program at Prince George’s Hospital Center. ________________________ Chief, Division Of Neurology _____________________________ Program Director, Residency Program I. Overview Neurology encompasses the prevention and management of disorders of the central and peripheral nervous systems. Other conditions, such as headache, may be caused by non-neural dysfunction but are often considered under the category of neurology. The general internist should possess a broad range of competency in neurology. He/she should be able to perform and interpret a detailed neurologic examination; should be competent in the primary and secondary prevention of neurologic diseases; and should be familiar with the presenting features, diagnosis, and treatment of common neurologic disorders. The general internist may encounter neurologic disorders in various settings, including ambulatory care, hospital, long-term care, and home care. At the end of their training Internist should be able to manage common neurological problems like peripheral neuropathy and be able to identify neurologic emergencies like cord compression, herniation etc. and to obtain appropriate consults. In communities where a neurologist is not available, the general internist may be a consultant for some complex neurologic disorders. II. Principle Teaching Methods It consists of frequent encounters with the attending physician regarding patient care. The resident will discuss all patients with the attending physician and interpret clinical data to formulate a differential. The attending will assign reading topics on a regular basis and review the material with the residents. This will include accepted national guidelines used in the diagnosis and treatment of various neurologic diseases. The faculty will also critique the residents consult notes, examination and management plan. Rounds will include short 15-30 minute discussions on current topics driven by patient encounters and initiated by resident and completed by the attending physician on most days. Latest information dealing with the topic as provided by literature search and pertinent articles should be discussed. Residents will also be required to take a one-hour test at the beginning and end of the rotation. The test will help residents understand their weaknesses and work to improve their knowledge during the rotation. The residents are required to report to the program coordinator at the beginning and end of the rotation for this exercise. III. Strengths and Limitations The residents will be exposed to a broad range of clinical problems typical of a community-based practice with emphasis on inpatient illness and care. The teaching faculty for the rotation is committed to teaching and patient care with strong role model presentation. There is on site neurological surgery, giving residents exposure to surgical management of acute bleeds, space-occupying lesions of spinal cord and shunt placement. ; but the increasing use of lytics and stent placement is more typical for community based care. The hospital does not have the ability to perform stereotactic biopsies at this time. For patients with exceptionally unusual clinical problems, the care may require transfer to a tertiary referral center. Outpatient experience in the subspecialty can be obtained by shadowing the attending physician in their private office. Patients in the continuity clinic at Glenridge Medical Center also offer learning opportunities. IV. Goals and Objectives Legend of Learning Activities Learning Venues: 1. Direct Patient Care/Consultation 2. Attending Rounds 3. Core Lecture Series 4. Self Study Evaluation Methods: A. Attending Evaluation B. Direct Observation C. Nurses’ Evaluation D. In-training Examination E. Pre and post rotation test Competency: Patient Care Learning Venues Evaluation Methods 1,2 A,B 1,2 A,B Demonstrate the ability to develop a differential diagnosis, diagnostic strategy, and management plan for patients with central nervous system disorders. 1,2 A,B,D,E Demonstrate the ability to develop a differential diagnosis, diagnostic strategy, and management plan for patients with peripheral 1,2 A,B,D,E Demonstrate proficiency in performing a detailed neurologic exam, and interpreting its results in a patient with neurologic disease. Demonstrate the ability to interpret ancillary tests, and radiographic studies pertinent to diseases of the nervous system and diagnose neurologic emergencies like status epilepticus and cord compression. nervous system disorders. Demonstrate the ability to manage the care and complications of patients with chronic neurologic disease, including chronic pain syndromes. 1,2 A,B,D,E Competency: Medical Knowledge Learning Venues Evaluation Methods 1,2,3,4 A,B,D,E 1,2,3,4 A,B,D,E 1,2,3,4 A,B,D,E 1,2,3,4 A,B,D,E 1,2,3,4 A,B,D,E 1,2,3,4 A,B,D,E Learning Venues Evaluation Methods 1,2 A,B,C 1,2 A,B Learning Venues Evaluation Methods 1,2 A,B 1,2 A,B,C Understand the pathophysiology, evaluation, and management of cerebrovascular accidents. Understand the pathophysiology, evaluation, and management of seizure disorders. Understand the pathophysiology, evaluation, and management of peripheral neuropathies. Understand the pathophysiology, evaluation, and management of dementia, including Alzheimer’s disease. Understand the pathophysiology, evaluation, and management of chronic pain syndromes, including headaches and low back pain. Know the appropriate indications for commonly ordered neurology tests and procedures, including: EEG, EMG, nerve conduction studies, evoked potentials, lumbar puncture, CT and MR imaging of brain and spinal cord Competency: Interpersonal and Communication Skills Interact in an effective way with physicians, nurses, and other personnel participating in the care of patients. Interact in an effective way with patients, and caregivers of those with neurologic disease. Competency: Professionalism Treat team members, primary care-givers, and patients with respect. Actively participate in rounds. Attend and participate in all scheduled conferences. Competency: Practice-Based Learning Identify limitations of medical knowledge and uses medical literature to address gaps in medical knowledge Competency: Systems-Based Practice Understand barriers to optimal care of patients with neurologic disease. Attendance sheet Learning Venues Evaluation Methods 1,2, A, D,E Learning Venues Evaluation Methods 1,2,3 A,B Understand the need for teamwork and a multidisciplinary approach in caring for those with neurologic disease. 1,2,3,5 A,B,C V. Educational Content A. Common presentations 1) Understand the causes for presentation of patients with: Abnormal speech Abnormal vision Altered mental status Syncope Altered sensation or weakness Memory loss Disturbance of gait or coordination Dizziness and vertigo Hearing loss Headache Localized pain syndrome: facial pain, radiculopathy Seizure Tremor 2) Perform thorough history and physical and order and interpret results of appropriate tests: Toxicology screen CSF findings Imaging studies: CT scan, MRI, carotid dopplers Electromyography, nerve conduction studies Electroencephalography, evoked potentials (visual, auditory, sensory Mini mental exam Anticonvulsant drug levels B. Central Nervous System Infection 1) Understand the causes, presentation, differential diagnosis, and management of: Brain abscess Encephalitis Meningitis: bacterial, viral and cryptococcal 2) Know indications and contraindications of lumbar puncture and interpret results of: Cerebrospinal fluid findings Imaging studies: MRI, CT scans Serum titers C. Cerebrovascular Accidents 1) Understand causes, presentations and management of: Stroke: ischemic, hemorrhagic TIA 2) Recognize complications of strokes including edema, bleeding into large CVA etc. 3) Know indications and contraindications of lumbar puncture and interpret results of: Cerebrospinal fluid findings Imaging studies: MRI, CT scans Serum titers D. Miscellaneous 1) Understand the causes, diagnostic criteria and management of: Benign positional vertigo Labrynthitis Headaches: cluster headache, migraines, tension headache Syncope Toxic encephalopathies like alcohol withdrawal, uremic and hepatic encephalopathy 2) Understand the indication and role of diagnostic tests including tilt table test E. Dementias 1) Understand the causes, diagnostic criteria and management of: Alzheimer’s Multi-infarct Lewy Body Normal Pressure Hydrocephalus Pseudodementia 2) Order appropriate tests and interpret results of Mini-mental test, cognitive evaluation Imaging studies Thyroid function CSF F. Spinal Cord Disease 1) Understand the causes, diagnostic criteria and management of Cord compression Epidural abscess Lumbar and cervical disc syndromes Spinal stenosis 2) Order appropriate tests, know indications for surgical evaluation of these conditions G. Peripheral Nervous System 1) Understand causes and management of peripheral neuropathy secondary to: Systemic disease like diabetes Toxins like alcohol Infections like HIV Nutritional deficiencies like Vitamin B12 2) Know the indications and interpretation of results of Nerve conduction studies EMG H. Neuromuscular Diseases/Movement Disorders 1) Understand the presentation, diagnosis and management of Amyotropic lateral sclerosis Guillain-Barre Syndrome Multiple sclerosis Muscular dystrophy Parkinsons disease Myasthenia gravis 2) Know indications and interpretations of appropriate tests including but not limited to: Imaging studies CSF results Edrophonium test Negative inspiratory force I. VI. Bleeding 1) Recognize the signs and symptoms and know the management of: Subarachnoid hemorrhage Subdural hematoma Recommended Readings All senior residents are encouraged to read the MKSAP for Neurology during their onemonth rotation. Questions will help develop analytical thinking. Residents should also consult the following texts during their rotation regarding the key clinical issues in diagnosis, pathophysiology and therapy raised by the patients they evaluate and care for on the neurology consult rotation: Harrison’s Principles of Internal Medicine Residents are also encouraged to use MDConsult and Up To Date to read on a case-by-case basis. Residents must also discuss latest guidelines for management of patients with stroke. A. Encephalopathy 1) Practice parameters for determining brain death in adults. Neurology 1995;45:1012-1014. 2) Booth C, Boone R, Tomlinson G, et al. Is this patient dead, vegetative or severelyneurologically impared? Assessing outcome for comatose survivors of cardiac arrest.JAMA 2004; 291(7):870-879. 3) Levy D, Caronna J, Singer B, et al. Predicting outcome from hypoxic-ischemic coma. JAMA 1995;253;10:1420-1426. (Abstract) 4) Mangano D, Mangano C. Perioperative stroke; ecephalopathy and central nervous system dysfunction. J Intensive Care Med 1997;12:148-160. B. Stroke 1) Adams H, Adams R, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: A scientific statement from the Stroke Council of the American StrokeAssociation. Stroke 2003;34:1056-1083. 2) Straus S, Majumdar S, McAlister E. New evidence for stroke prevention: Scientific Review JAMA 2002;288(11):1388-1395. 3) Straus S, Majumdar S, McAlister E. New evidence for stroke prevention: Clinical Applications. JAMA 2002;288(11):1396-1398. 4) Donnan G, David S. Controversies in stroke. Stroke 2002;33:2137-2140. 5) Adams H. Patent foramen ovale: paradoxical embolism and paradoxical data. Mayo Clin Proc 2004;79:15-20. 6) Horton S, Bunch T. Patent foramen ovale and stroke. Mayo Clin Proc. 2004;79:79-88. 7) Hiott B, Lentz S. Prothrombotic states that predispose to stroke. Current Treatment Options in Neurology 2002;4:417-425. 8) Muir K. Secondary prevention for stroke and transient ischaemic attacks. BMJ 2004;328:297-298 9) Brott T., Bogousslavsky J. Drug Therapy: Treatment of Acute Ischemic Stroke N Engl J Med 2000; 343:710-722, Sep 7, 2000. 10) Blacker DJ - Lancet Neurol In-hospital stroke 01-DEC-2003; 2(12): 741-6 C. Seizure 1) Manno E. New management strategies in the treatment of status epilepticus. Mayo Clin Proc 2003;78:508-518. 2) Herman S. Single unprovoked seizures. Current Treatment Option in Neurology 2004;6:243-255. 3) Kaufmann H, Bhattacharya K. Diagnosis and treatment of neurally mediated syncope.The Neurologist 2002;8:175-185. 4) Browne T. R., Holmes G. L. Epilepsy N Engl J Med 2001; 344:1145-1151, Apr 12, 2001. D. Headache 1) Diamond M. Emergency room treatment of migraine headache. Current Treatment Options in Neurology 2002;4:351-356. 2) Lucas S. Initial abortive treatments for migraine headache. Current Treatment Options in Neurology 2002;4:343-350. 3) Moore K. Management of chronic headache in the era of managed care. The Neurologist 1997;3:209-240. E. Dementia 1) Bolla LR, Filley CM, Palmer RM. Office diagnosis of the four major types of dementia. Geriatrics 2000; 55:34-46 F. Neuromuscular Disease 1) Van der Meche F, Van Doorn P. Guillain-Barre Syndrome. Current Treatment Options in Neurology 2000;2:507-516. 2) Briemberg H, Amato A. Dermatomyositis and polymyositis. Current Treatment Options in Neurology 2003;5:349-356. 3) Bolton C, Young GB. Critical illness polyneuropathy. Current Treatment Options in Neurology 2000;2:489-498. 4) Rowland L. P., Shneider N. A. Medical Progress: Amyotrophic Lateral Sclerosis. N Engl J Med 2001; 344:1688-1700, May 31, 2001 G. Multiple Sclerosis 1) O’Conner P. Key issues in the diagnosis and treatment of multiple sclerosis. Neurology 2002;59(6)(3):1-33. 2) Noseworthy, et al, Multiple Sclerosis, NEJM 343(13): 938-952, 2000 3) Corboy JR, Goodin DS, Frohman EM. Disease-modifying Therapies for Multiple Sclerosis. Curr Treat Options Neurol. 2003 Jan;5(1):35-54. H. Peripheral Neuropathy 1) Irving GA. Neurology Contemporary assessment neuropathic pain.- 28-JUN-2005; 64(12 Suppl 3): S21-7 I. and management of Aphasia 1) Damasio AR. Aphasia. New Engl J Med 1992; 326: 531-539 J. Movement Disorders 1) Rubino F. Gait Disorders. The Neurologist 2002;8;254-262. (Abstract) 2) Bertoni JM. Long-term medical treatment for Parkinson’s disease. Current treatment options in Neurology 2001; 3: 495-506. K. Concussion 1) Kelly JP, Nichols JS, Filley CM, Lillehei KO, Rubinstein D, KleinschmidtDeMasters BK. Concussion in Sports: Guidelines for the Prevention of Catastrophic Outcome. JAMA 1991;266(20):2867-2869. 2) Kelly JP. Traumatic brain injury and concussion in sports. JAMA 1999;282:989991.